Page 64
conferenceseries
.com
Volume 7
Journal of Pain & Relief
ISSN: 2167-0846
Pain Management 2018
October 11-12, 2018
October 11-12, 2018 | Zurich, Switzerland
7
th
International Conference and Exhibition on
Pain Research and Management
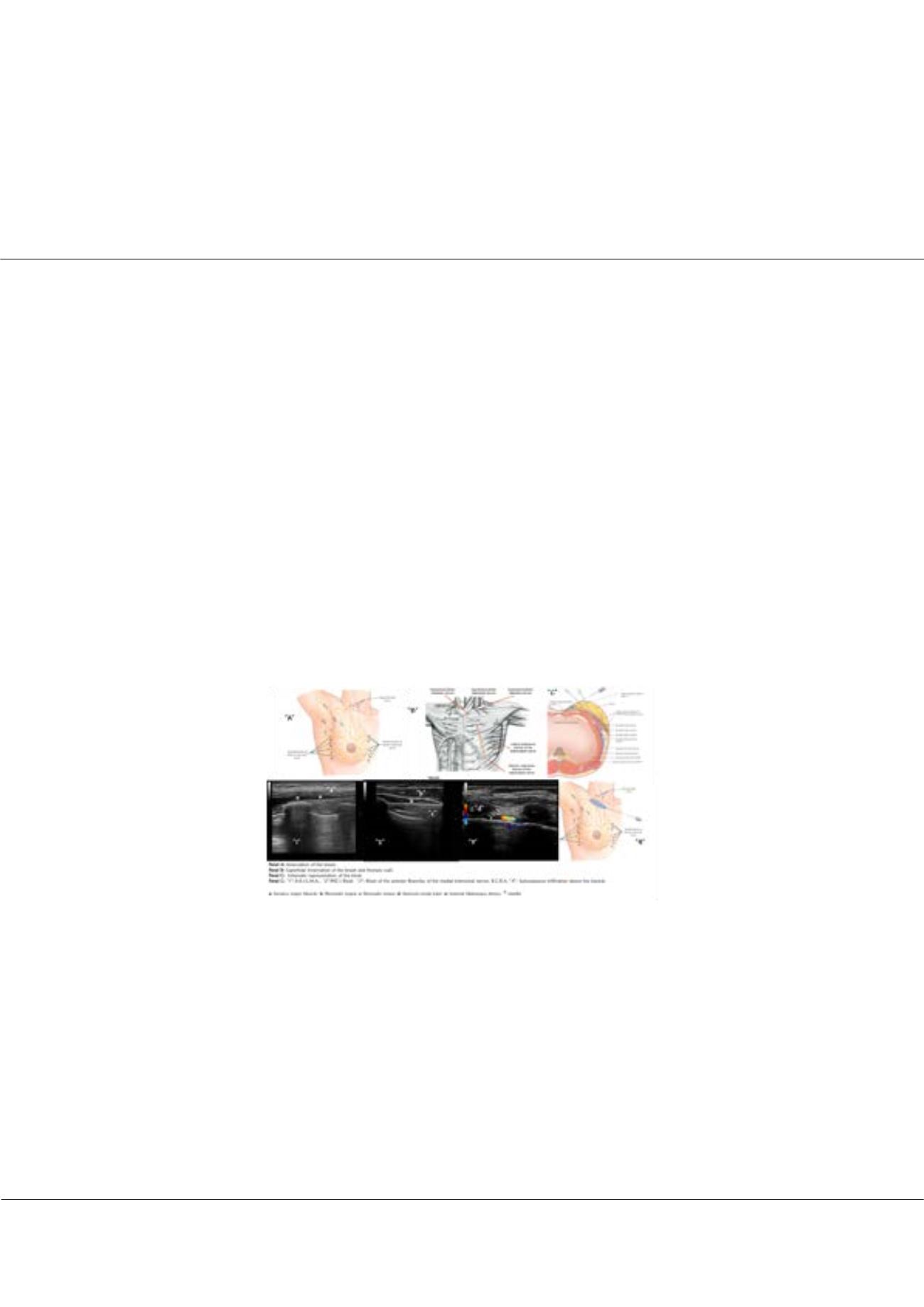
The complete breast block, an approach to prevent the postmastectomy chronic pain progression
Juan Bernardo Schuitemaker
General University Hospital of Catalonia, Spain
T
he breast cancer is the most common cancer suffered by woman in the United States, the lifetime risk of developing breast
cancer is about 12% for the average woman, which means 1 in 8 women in the United States will develop it. An estimated
253,000 women in the United States will be diagnosed with invasive breast cancer in 2017, and another 63,000 with
in situ
breast cancer. According to a recent epidemiologic study, higher breast cancer rates were expected between 2009 and 2015.
Acute postoperative pain is an integral risk factor in the development of chronic postmastectomy pain; 40% of women will
have severe acute postoperative pain after breast cancer surgery, whereas 50% will develop chronic postmastectomy pain with
impaired quality of life. For the cohort of women receiving breast cancer surgery (BCS), accumulating evidence suggests a
substantial prevalence of chronic postsurgical pain estimated to range between 29 and 57%. Similarly, available studies suggest
that from one-fourth to one-half of women who undergo post-mastectomy breast reconstruction surgery report chronic
postsurgical pain. Based on this, we proposed in 2015 a new approach of complete breast block for breast surgeries, based in
the complex breast innervation, so we perform a modified PECS II, B.R.I.L.M.A., B.R.C.A. plus a subcutaneous infiltration in
the inferior edge of the clavicle to block the cutaneous branches of the superficial cervical plexus. With this approach we have
performed more than 500 breast surgeries, using it as a part of a multimodal approach, general anesthesia with laryngeal mask
airway (LMA), remifentanil for the air way management, with an excellent hemodynamic stability and pain free postoperative
period. We believe that using this approach the patients must have a pain free intraoperative and postoperative period and will
fall the progression to chronic pain. Future studies are needed to validate this observation.
Recent Publications:
1. Schuitemaker Requena J B, Mayoral Ripamonti J T, Sala Blanch X, Muñoz S L, Imbiscuso Esqueda A T, Pesa Vendrell
N, Arteaga Mejía D, Braso Vicen C, Tintore Caicedo X and Sanchez Cohen A P (2015) In plane lateral approach of the
pectoral nerves. A PEC II modification. Reg Anesth Pain Med. 40(5):e123.
2. Desantis C, Ma J, Bryan L and Jemal A (2014) Breast cancer statistics, 2013. CA Cancer J Clin. 64(1):52–62.
3. Sbitany H (2018) Breast reconstruction. Surg Clin North Am. 98(4):845–57.
4. Hirko K A, Soliman A S, Hablas A, et al. (2013) Trends in breast cancer incidence rates by age and sage at diagnosis in
Gharbiah, Egypt, over 10 years (1999-2008). J Cancer Epidemiol. DOI: 10.1155/2013/916394.
5. Poleshuck E L, Katz J, Andrus C H, Hogan L A, Jung B F, Kulick D I and Dworkin R H (2006) Risk factors for chronic
pain following breast cancer surgery: a prospective study. J Pain. 7:626–34.
Juan Bernardo Schuitemaker, J Pain Relief 2018, Volume 7
DOI: 10.4172/2167-0846-C1-020
















