Page 49
conferenceseries
.com
Volume 20, Issue 7 (Suppl)
J Psychiatry
ISSN: 2378-5756 JOP, an open access journal
Psychiatry and Mental Health 2017
November 20-21, 2017
November 20-21, 2017 Melbourne, Australia
28
th
International Conference on
Psychiatry and Mental Health
The prevalence and associations of psychological distress in Australian junior medical officers
Michelle W Lau, Wenlong Li, Anthony Llewellyn and Allan M Cyna
Nepean Hospital in New South Wales, Australia
Objective:
To determine the prevalence of psychological distress
in Australian Junior Medical Officers (JMOs) and to investigate the
determinants associated with psychological distress over a three-
year (2014-2016) period.
Methods:
JMOs were surveyed using the 2014-2016 JMO Census
(n=220, 399 and 466 each year, response rate approximately 15%).
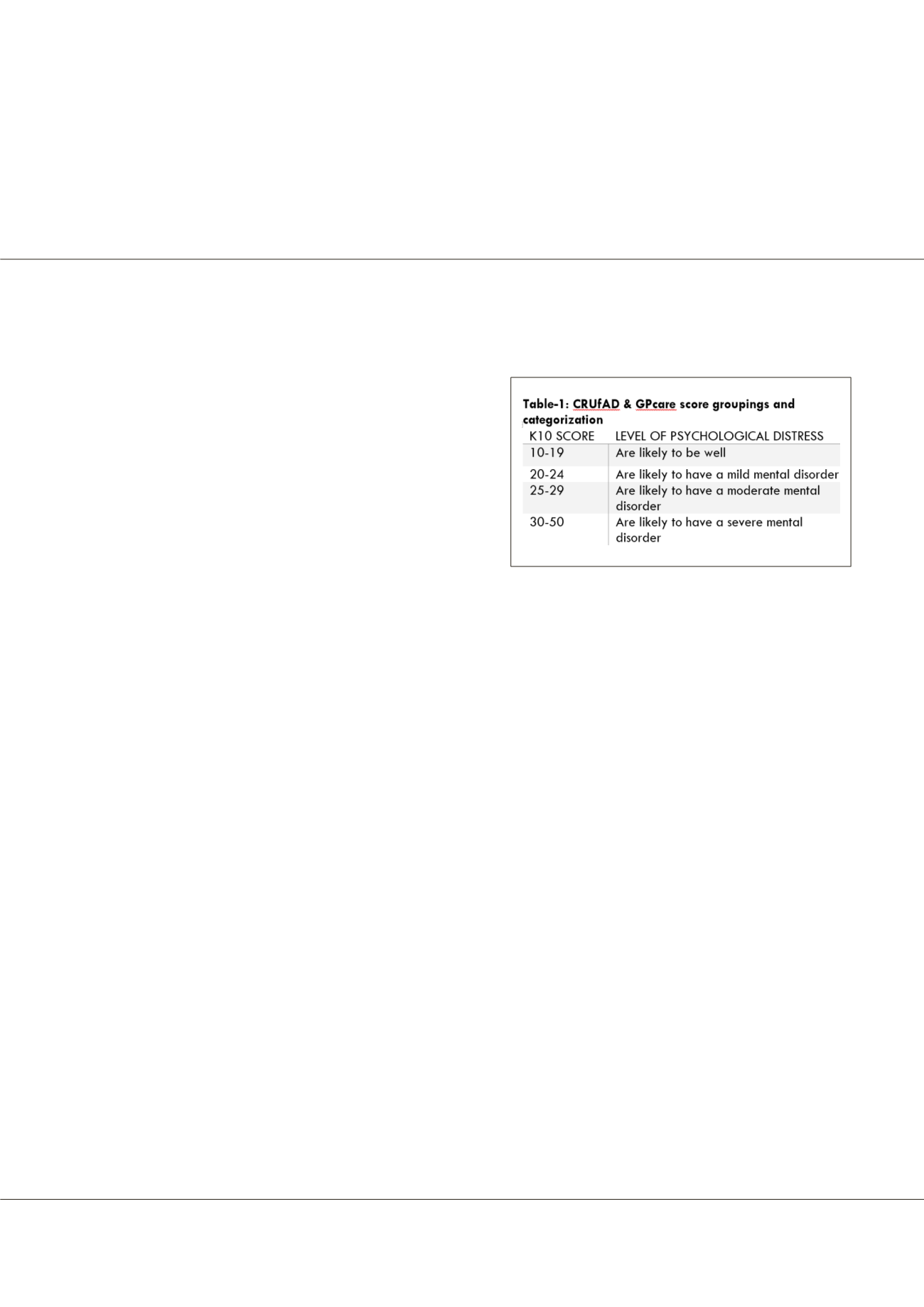
Levels of psychological distress were assessed using the Kessler
Psychological Distress Scale (K10). A K10≥25 was chosen to indicate
high psychological distress and this determinant was compared to
various demographic and work-related factors.
Results:
Australian JMOs experience a high level of psychological distress (mean of 18.1, median 16.0). There were no differences
in demographical variables such as age, sex, marital status, dependents and between PGY 1 and 2. Increasing hours worked per
week was associated with a higher K10, with every hour worked increasing odds by 3%. Attitudinal items including feeling
unwilling to study medicine again, feeling poorly trained and experiences of bullying were related to high psychological distress.
Coping strategies like exercise and spending time with friends correlated positively with lower distress, whilst time off work,
frequent alcohol use, smoking and drug use were associated with increased distress levels. 54.5% of those with a high K10
indicated that they did not use any form of professional support. 17.83% expressed that given their time again; they would not
choose to study medicine.
Conclusion:
A focused approach to JMO support and education regarding significant risk factors identified is likely to assist
health policies that aim to improve the mental wellbeing of Australian JMOs.
References
1. Visser M, Smets E, Oort F, et al. (2003) Stress, satisfaction and burnout among Dutch medical specialists.
CMAJ
; 168: 271-275
2. Antoniou A S, Davidson M J and Cooper C L (2003) Occupational stress, job satisfaction and health state in male and female
junior hospital doctors in Greece.
Journal of Managerial Psychology
; 20(6): 592-621.
3. Tyssen R and Vaglum P (2002) Mental health problems among young doctors: an updated review of prospective studies.
Harv Rev Psychiatry
; 10: 154-165.
4. Mc-Manus I C, Winder B C and Gordon D (2002) The causal links between stress and burnout in a longitudinal study of UK
doctors.
Lancet
; 359: 2089-2090.
5. Newbury-Birch D, Kamali F (2001) Psychological stress, anxiety, depression, job satisfaction, and personality characteristics
in preregistration house officers.
Postgrad Med J
; 77: 109-111.
Biography
Michelle W Lau is a Resident Medical Officer and currently working at Nepean Hospital in New South Wales, Australia. She has keen interest in clinical governance
and improvement in the welfare of junior doctors and doctors in training. Her area of interest is in the mental health and wellbeing of her fellow residents and interns,
who are a high-risk group known for working long hours and manage high stress situations in the workplace.
mich.lau@hotmail.comMichelle W Lau et al., J Psychiatry 2017, 20:7 (Suppl)
DOI: 10.4172/2378-5756-C1-030
















