Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
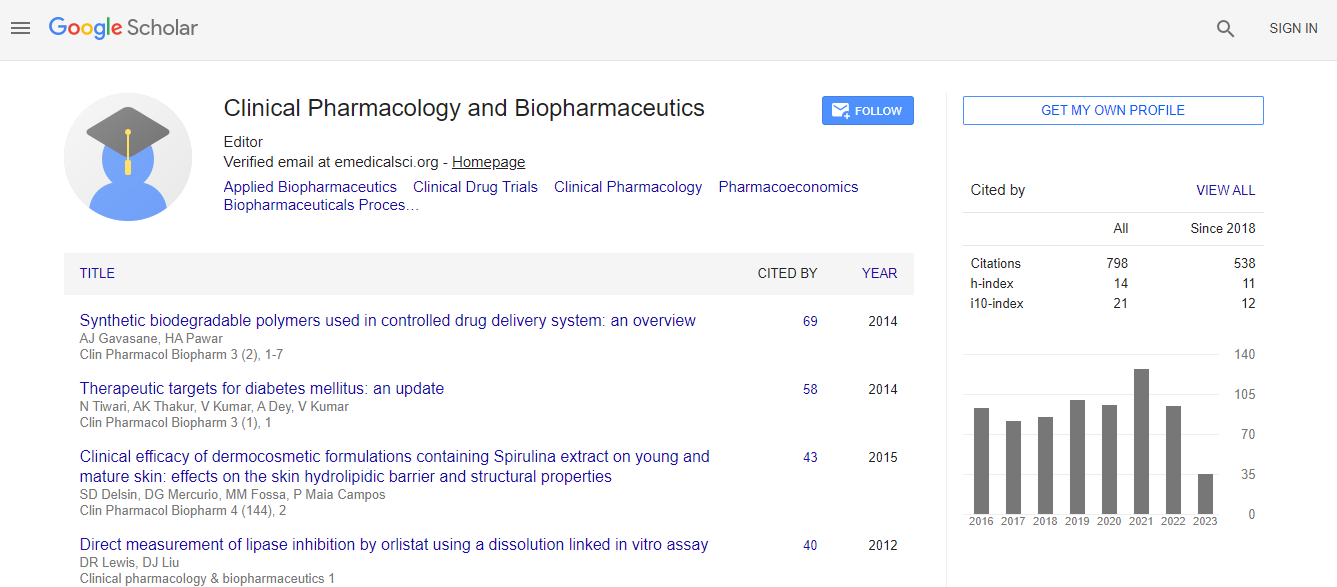
Google Scholar citation report
Citations : 1089
Clinical Pharmacology & Biopharmaceutics received 1089 citations as per Google Scholar report
Clinical Pharmacology & Biopharmaceutics peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
The Protect�?±ve Effect Of Prophylact�?±c Ozone Adm�?±n�?±strat�?±on Aga�?±nst Ret�?±nal Ischem�?±a Reperfus�?±on Injury
International Conference and Expo on Biopharmaceutics
Ali Kal, Oznur Kal, Ishak Akillioglu, Esin Celik, Mustafa Yilmaz, Saban Gonul, Merve Solmaz, Ozkan Onal
Selcuk University Medical Faculty Department of Anesthesiology and Reanimation, Turkey Baskent University Medical Faculty Department of Ophtalmology , Turkey Baskent University Medical Faculty Department of Nephrology, Turkey Baskent University Me
Posters-Accepted Abstracts: Clin Pharmacol Biopharm
Abstract
Introduction: Many retinal diseases are associated with vascular dysfunction accompanied by neuroinflammation. Retinal ischemia/ reperfusion (IR) injury is associated with many ocular diseases, including acute glaucoma, diabetic retinopathy, and retinal vascular occlusion. Retinal ischemia/reperfusion injury leads to the death of retinal ganglion cells (RGCs), morphological degeneration of the retina, the loss of retinal function, and ultimately, vision loss. The intraocular pressure-induced retinal ischemia reperfusion (IR) model is a useful tool for studying the neuronal response to a transient ischemic injury. Ozone (O3) has been used as a therapeutical agent for the treatment of different diseases . Moreover, ozone could prepare the host to face physiopathological events mediated by reactive oxygen species. Additionally its triggering the formation of new capillary, increasing the number of defensive cells in immune response, and cellular energy release, and anti-oxidant efficacy may be mentioned. The aim of the present study was to show the protective effect of prophylactic ozone administration against retinal ischemia reperfusion injury. Material and Method: Control group (n:6) was administered SF intraperitoneally seven days without creating ischemia reperfusion injury and at eight day the rats were sacrified. Ozone group (n:7) was administered 1 mg/kg ozone intraperitoneally for seven days without creating ischemia reperfusion injury and at eight day the rats were sacrified. Ischemia Reperfusion (IR) group (I/R) (n:7) were subjected to retinal ischemia by cannulating the anterior chamber of the right eye with a 27- gauge infusion needle connected to a reservoir containing normal saline and by raising the intraocular pressure (IOP) to 130 mmHg for 1 hour by elevating the saline reservoir and then reperfusion for two hours. In Ozone + IR group, 1 mg/kg ozone was administered intraperitoneally for seven days before the ischemia/reperfusion procedure and at eight day the ischemia reperfusion injury was created (as in group 3) and rats were sacrified at the same day. Subsequently, ischemia was terminated after 1 hour and 2nd hour of reperfusion rats were anesthetized with 80 mg/kg ketamin and their intracardiac blood was drawn completely and they were sacrificed. Blood samples were sent to laboratory for superoxide dismutase (SOD), glutation peroxidase (GSH-Px), malondyaldehide (MDA) total oxidant score (TOS) and total antioxidant capacity (TAC) analysis. The degree of retinal injury was evaluated according to changes in retinal cells (ganglion cell layer, inner plexiform layer, inner nuclear layer, outer plexiform layer and outer nuclear layer) and necrotic and apoptotic cells by Tunel method. Data were evaluated statistically by Kruskal Wallis test. Results: The number of retinal ganglion cells and the inner retinal thickness were significantly decreased at 7 days after ischemia, treatment with ozone significantly inhibited retinal ischemic injury even increased compared to all groups. In ischemia-reperfusion group, the degree of retinal injury was found highest and statically significantly compared to the other groups (p<0.05). In the group administered ozone before ischemia reperfusion procedure, retinal injury was found to be decreased in comparison to IR group (p<0.05). In ozone group administered only sf without creating retinal ischemia/reperfusion injury, retinal injury score was the lowest in comparison to the other groups (p<0.05). The difference according to the antioxidant parameters SOD, GPX TAC values were found to be increased in ozone group and lowest in IR group (p<0.05). The difference according to the oxidant parameters MDA and TOS were found to be highest in IR group and decreased in ozone group (p<0.05). Discussion: The present study demonstrated that ozone administration prevented ischemia-reperfusion injury. The formation of reactive oxygen and nitrogen components lead to activation and inflammatory cells, and production of systemic mediators and cytokins and apoptosis resulting in increase in retinal cells. Retinal diseases invariably involve a combination of neurodegeneration, vascular dysfunction and inflammation in various proportions. The retinal IR injury model has primarily been used to explore means to prevent the neurodegenerative response triggered by a transient ischemic insult, but it also provides a useful means to explore the prevention of vascular and inflammatory responses to injury. The production of reactive oxygen species is a major pathophysiological component of retinal ischemia/reperfusion injury. The generation of reactive oxygen species is also positively correlated with the degree of early apoptosis, inflammation, and necrosis in retinal ischemia/reperfusion injury. In conclusion, this study demonstrated that the ozone, can attenuate subsequent ischemic damage in the rat retina by antioxidative effect.Biography
Email: drozkanonal@selcuk.edu.tr

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi