Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
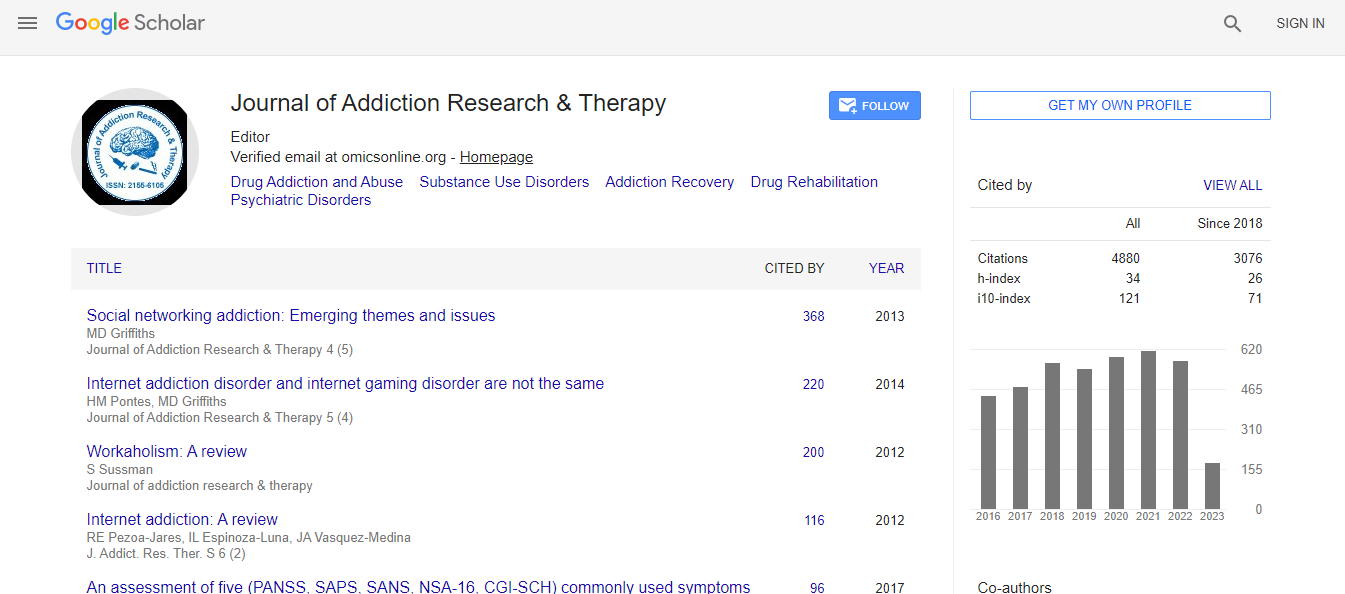
Google Scholar citation report
Citations : 4859
Journal of Addiction Research & Therapy received 4859 citations as per Google Scholar report
Journal of Addiction Research & Therapy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- SafetyLit
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Sublingual suboxone (buprenorphine/naloxone) leading to acute urinary retention requiring emergent attention
3rd International Conference and Exhibition on Addiction Research & Therapy
Abhishek Rai
Posters: J Addict Res Ther
Abstract
Introduction: Acute urinary retention (AUR) is the inability to urinate and is the most common urologic emergency. Etiologies include trauma, medication, neurologic disease, infection and occasionally, psychological issues. AUR is commonly associated with epidural or intrathecal buprenorphine. It is, however, rarely reported with the use of sublingual buprenorphine with naloxone preparation (Suboxone). We report a case of acute urinary retention precipitated by initiating sublingual buprenorphine and naloxone (Suboxone). Case Report: Mr. X is a 58-year-old Caucasian male with a history of opiate dependence, benzodiazepine dependence, and cannabis dependence, depression with no prior hospitalization for mental health issues or substance detoxification. Patient started on pain medications for his osteoarthritis and chronic pain. Two years ago, he started abusing his pain medications. His opioid use was associated with regular abuse of cannabis and benzodiazepine. His medical history was significant for benign prostatic hyperplasia (BPH, treated with tamsulosin which was diagnosed during the hospital stay) and hepatitis C. Patient never reported any episode of urinary retention in the past. Mr. X was admitted to the chemical dependency unit (CDU) for opioid dependence. He started on sublingual Suboxone, phenobarbital taper and gabapentin to treat his opioid and benzodiazepine dependence. Initial dose of Suboxone was 8 mg daily. The dose was further titrated to 12 mg daily on day 2. Patient then complained of urinary retention on day 3 of his admission to CDU. His complaint of inability to urinate was complicated by suprapubic discomfort and bladder distention which was only relieved by immediate urethral catheterization. Urology was consulted, and cystoscopy was done. Patient was found to have mild to moderate BPH and was started on tamsulosin with a long-term plan of prostatectomy. At that point, it was believed that Suboxone contributed partially to his urinary hesitancy. His dose of Suboxone was tapered to 4 mg daily. Patient was discharged home with regular self-catheterization and 4 mg of Suboxone daily. Patient continued his self-catheterization while at home as his urinary retention decreased but never resumed to spontaneous urination. 3 days later, patient again presented to the emergency department with severe withdrawal symptoms of opioid dependence. Patient was re-admitted to CDU, and decision was made to discontinue Suboxone and detoxify him using the traditional method of using clonidine and phenobarbital. On day 2 of discontinuation of Suboxone, patient resumed spontaneous urination. Patient was detoxified using traditional method for the next 5 days and discharged home with no Suboxone with plan for intensive outpatient treatment. Discussion: Suboxone, a sublingual tablet consisting of buprenorphine and naloxone, is very commonly used to treat opioid dependence. Buprenorphine is a partial agonist at mu opiate receptor and antagonist to kappa receptor. Naloxone, a competitive antagonist at the mu opioid receptor is inactive when used sublingually. The inhibition of bladder afferents at the dorsal horn via mu receptor activation decreases bladder sensation and thereby leading to urinary hesitancy and chronic urinary retention with only long term use. Acute urinary retention associated with suboxone is much less common. Conclusion: Initial management of AUR requires prompt bladder decompression by urethral or suprapubic catheterization. Over 50% of AUR are precipitated by BPH. It is likely that in our case, the patients urinary symptoms are due to BPH exacerbated by initiation of Suboxone. In elderly male patients with a known history of urinary hesitancy or BPH, it becomes important to take that into consideration before initiating Suboxone. Patients should also be checked routinely for urinary symptoms after the medication is initiatedBiography
Abhishek Rai, MD, is a full time psychiatry resident at St. Mary Mercy Hospital in Livonia, MI. After graduating from one of the most prestigious medical schools in India, Dr. Rai moved to the USA. In a brief stint at Mayo Clinic Rochester MN (2010-2011), he gained firsthand experience in the department of psychiatry after which he joined the child psychiatry unit of New York State Psychiatry Institute (Columbia University) and has worked there before joining his residency. He is an active member of American Psychiatry Association. He has a number of med indexed publications to his credit and has presented several posters and cases at International conferences. In addition Dr. Rai is an active member of and voluntary editor to AAAP (American academy of addiction psychiatry)

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi