Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
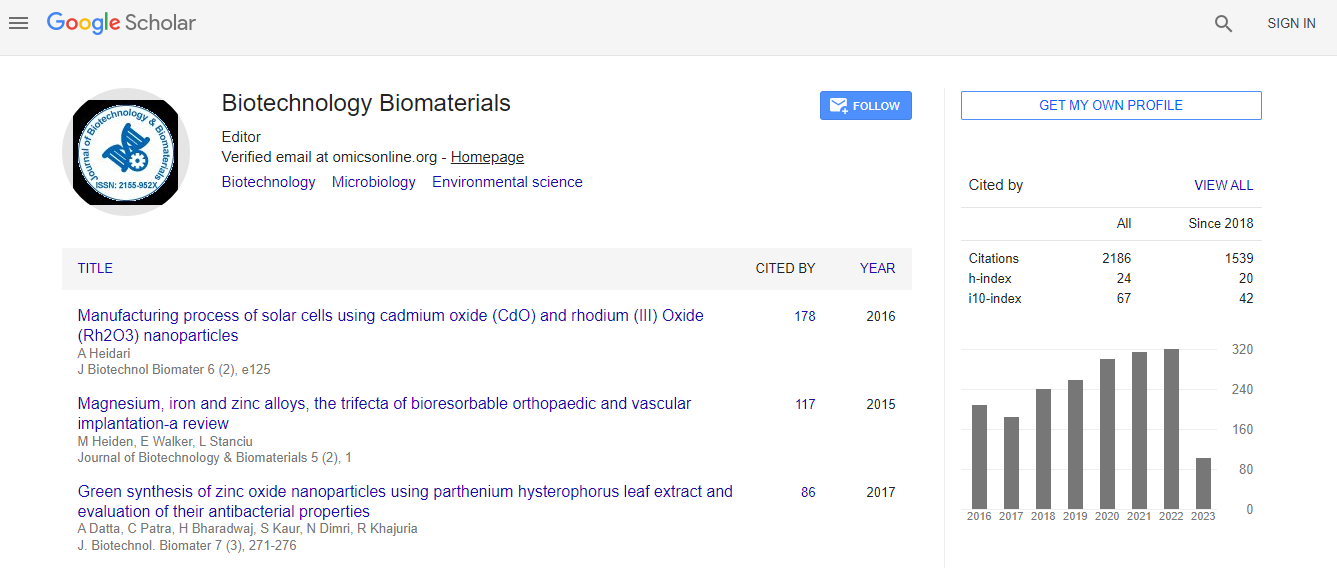
Google Scholar citation report
Citations : 3330
Journal of Biotechnology & Biomaterials received 3330 citations as per Google Scholar report
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Stem cell therapy for the treatment of severe tissue damage after radiation exposure
Biotechnology World Convention
A Chapel, A Semont, N Mathieu, C Linard, L Douay, N C Gorin, M Mothy, J M Simmon, J J Lataillade, J Voswinke, R Tamarat and M Benderitter
Institute of Radiological Protection and Nuclear Safety, France Saint Antoine Hospital AP-HP, France Pitie-Salpetriere University Hospital, Paris, France Percy Military Hospital, France UPMC University, France
Posters & Accepted Abstracts: J Biotechnol Biomater
Abstract
Radiotherapy may induce irreversible damage on healthy tissues surrounding the tumor. It has been reported that the majority of patients receiving pelvic radiation therapy shows early or late tissue reactions of graded severity as radiotherapy affects not only the targeted tumor cells but also the surrounding healthy tissues. The late adverse effects of pelvic radiotherapy concern 5 to 10% of them, which could be life threatening. However, a clear medical consensus concerning the clinical management of such healthy tissue sequelae does not exist. Although no pharmacologic interventions have yet been proven to efficiently mitigate radiotherapy severe side effects, few preclinical researches show the potential of combined and sequential pharmacological treatments to prevent the onset of tissue damage. Our group has demonstrated in preclinical animal models that systemic MSC injection is a promise approach for the medical management of gastrointestinal disorder after irradiation. We have shown that MSC migrate to damaged tissues and restore gut functions after irradiation. We carefully studies side effects of stem cell injection for further application in patients. The clinical status of four first patients suffering from severe pelvic side effects resulting from an over-dosage was improved following MSC injection in a compassional situation. Bone marrow-derived MSC from the patients├ó┬?┬? children were injected to four patients. A quantity of 2├?┬?106-6├?┬?106 MSC/kg was infused intravenously to the patients. Pain, hemorrhage, frequency of diarrheas and fistulisation as well as the lymphocyte subsets in peripheral blood were evaluated before MSC therapy and during the follow-up. Two patients revealed a substantiated clinical response for pain and hemorrhage after MSC therapy. In one patient pain reappeared after 6 months and again substantially responded on a second MSC infusion. A beginning fistulisation process could be stopped in one patient resulting in a stable remission for more than 3 years of follow-up. The frequency of painful diarrhea diminished from an average of 6/d to 3/d after the first and 2/d after the 2nd MSC injection in one patient. A decline of CD4+ and CD8+ T lymphocytes and an increase of potentially regulatory CD25+ T cells accompanied the clinical response in this patient after the MSC injections. In all patients, prostate cancer remained in stable complete remission. A modulation of the lymphocyte subsets towards a regulatory pattern and diminution of activated T-cells accompanies the clinical response in refractory irradiation-induced colitis. No toxicity occurred. MSC therapy was safe and effective on pain, diarrhea, hemorrhage, inflammation, fibrosis and limited fistulisation. For patients with refractory chronic inflammatory and fistulising bowel diseases, systemic MSC injections represent a safe option for salvage therapy. A clinical phase II trial will start in 2016.Biography
Email: alain.chapel@irsn.fr

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi