Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
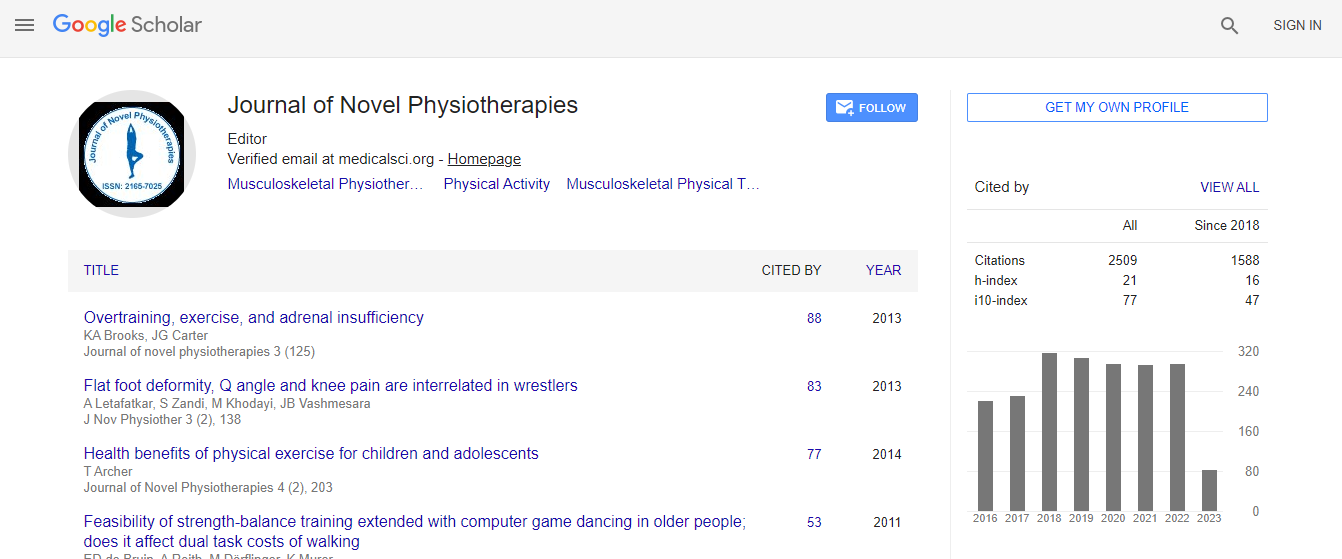
Google Scholar citation report
Citations : 3145
Journal of Novel Physiotherapies received 3145 citations as per Google Scholar report
Journal of Novel Physiotherapies peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Sensitization in myofascial pain syndrome
2nd International Conference and Expo on Novel Physiotherapies
Areerat Suputtitada
Chulalongkorn University, Thailand King Chulalongkorn Memorial Hospital, Thailand
Keynote: J Nov Physiother
Abstract
Sensitization in corresponding spinal segments plays a major role in the formation of continuous pain in a given part of the body. The term called by Professor Andrew A. Fischer for this phenomenon is â�?�?spinal segmental sensitizationâ�? (SSS). Chronic pain is contributed by sensitization of spinal nociceptive neurons, regardless of the original provoking events. SSS is a hyperactive state of the spinal cord caused by irritative foci sending nociceptive impulses from a sensitized damaged tissue to dorsal horn neurons. The clinical manifestation of dorsal horn sensitization includes hyperalgesia of the dermatome, pressure pain sensitivity of the sclerotome and myofascial trigger points within the myotomes, which are supplied by the sensitized spinal segment. In Myofascial pain syndrome (MPS) first described by Professor Janet G Travell and Professor David G Simons, active myofascial trigger points present lower pressure pain threshold when compared to people with no pain or the presence of only latent trigger points. There are significant elevated levels of substance P, calcitonin gene-related peptide (CGRP), bradykinin, tumor necrosis factor-�?± (TNF-�?±) and interleukin- 1�?² (IL-1�?²), serotonin, and norepinephrine in the vicinity of the active myofascial trigger point. Overall, pH was significantly lower in the active trigger point. Treatment rationale and techniques may evolve from this information, and should be taken into account when dealing with chronic patients with amplified pain responses. The mechanism consists of the nociceptive stimuli generated in the sensitized areas bombarding the dorsal horn of the spinal cord. This causes central nervous system sensitization with resultant hyperalgesia of the dermatome and sclerotome and spreads from the sensory component of the spinal segment to the anterior horn cells, which control the myotome within the territory of the SSS. The importance of SSS is emphasized by the fact that it is consistently associated with musculoskeletal pain. The development or amplified activity of MTrPs is one of the clinical manifestations of SSS. The segmental desensitization treatment consists of injection of local anesthetic agents in the involved dermatome to block the posterior branch of the dorsal spinal nerve along the involved paraspinal muscles. In addition, local anesthetic injection is applied peripherally near the foci of irritation in local soft tissue, directly into taut bands and trigger points, using a needling and infiltration technique. Stretching exercises, local heat application and additional transcutaneous electrical nerve stimulation (TENS) treatment complete the muscular relaxation after the injections. Extracorporeal shockwave therapy (ESWT) can also play a role in desensitization.Biography
Areerat Suputtitada, MD, is a Professor of Physical and Rehabilitation Medicine. She is the Chairperson of Neurorehabilitation Research Unit at Chulalongkorn University and Chairperson of Excellent Center for Gait and Motion at King Chulalongkorn Memorial Hospital in Thailand. She was invited as international speaker for more than 60 times around the world. She received 18 international and national awards, and published more than 60 international and national articles in the areas of her expertise including neurological rehabilitation, spasticity and dystonia, gait and motion, and pain. She is an expert clinician in ESWT for various indications in the field of physical and rehabilitation medicine. She has been elected and appointed to important positions at ISPRM such as the Chair of Women and Health Task Force and the International Exchange Committee.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi