Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
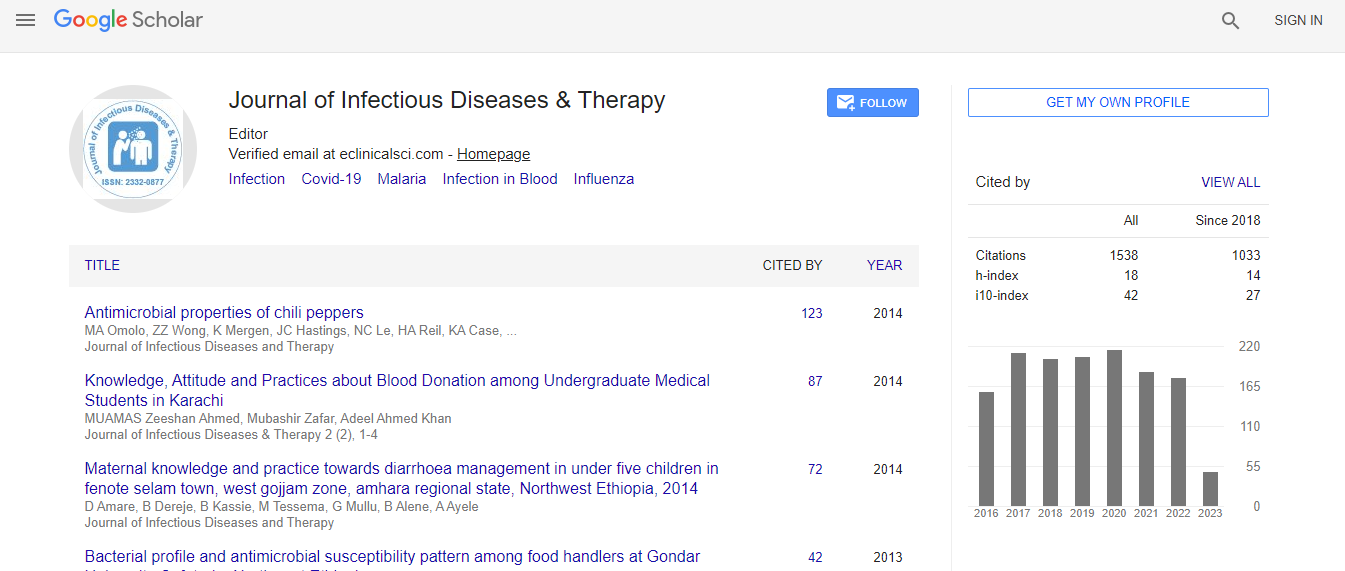
Google Scholar citation report
Citations : 1529
Journal of Infectious Diseases & Therapy received 1529 citations as per Google Scholar report
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Recurrent cardiac tamponade secondary to coxsackie B type 4
Joint Event on 2nd World Congress on Infectious Diseases & International Conference on Pediatric Care & Pediatric Infectious Diseases
Moamen AL Zoubi, Sujata Situla and Carmen Jan Liao
Advocate Illinois Masonic Medical Center, USA
Posters & Accepted Abstracts: J Infect Dis Ther
Abstract
Cardiac tamponade is a life threatening condition often requiring urgent or emergent pericardiocentesis and close monitoring in the ICU. We report a 51 year-old spanish speaking female with a history of hypothyroidism who presented with facial swelling , SOB and orthopnea for 3 weeks. She denies joint pain, rash, fever, chills, weight loss. She had travelled to Mexico 6 years ago but did not remember exposure to TB patients. She had not received BCG vaccine as a child. In the ER her vitals were stable. Labs were remarkable for Alk phos 230, AST 63 and ALT 102. Otherwise, unremarkable including normal thyroid function test. ANA comprehensive panel and HIV test were negative. The ECG showed sinus rhythm and low QRS amplitude. Chest X-ray demonstrated bilateral pleural effusion. Echocardiogram showed large pericardial effusion with features consistent with tamponade physiology. Urgent pericardiocentesis was done with 450 ml fluid withdrawn. Thoracentesis was done as well and samples were sent for analysis. The fluids was an exudate. AFB smears and fungal culture came back negative. Repeated Echo showed complete resolution of pericardial effusion. Patient was discharged on colchicine 0.6 mg by mouth twice a day x2 weeks. Two weeks later the patient presented again with dyspnea and found to have cardiac tamponade after performing Echocardiography. Patient was taken to the operating room and a pericardial window was performed. TB quantiferon test found to be positive from the previous admission and she was started empirically on anti-TB medication as recommended by infectious diseases service. The results of pericardial biopsy showed no evidence of TB or sarcoidosis. No granulomas or malignant cells were seen. AFB smear was negative in three consecutive samples and Anti-TB medication were discontinued. Viral serology sent and came back elevated as high as 320:1 for coxsackie B type 4. Repeated Echocardiogram showed no pericardial effusion and patient reported improvement of her symptoms. The patient was discharged on indomethacin 50 mg BID with a cardiology follow up in 2 weeks. To the best of our knowledge, this is the first reported case of cardiac tamponade secondary to group B coxsackieviruses. We encourage considering viral causes as a probable etiology for cardiac tamponade of unknown etiology.Biography
Moamen AL Zoubi is affiliated to Advocate Illinois Masonic Medical Center, USA moamen.
Email: alzoubi@gmail.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi