Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
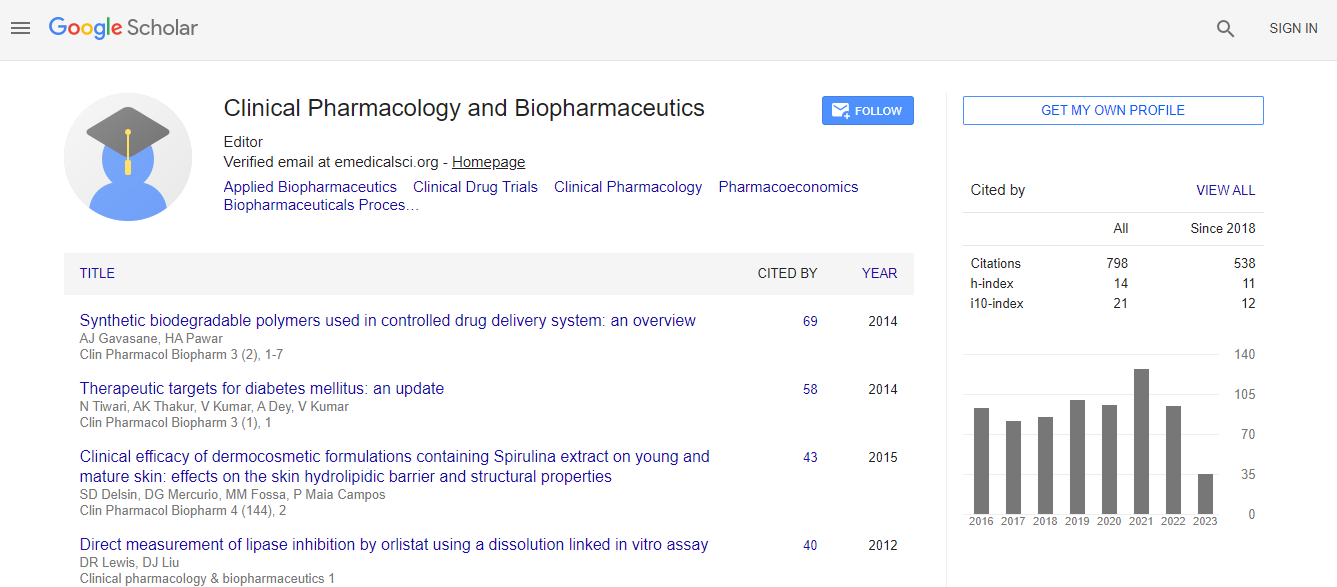
Google Scholar citation report
Citations : 1089
Clinical Pharmacology & Biopharmaceutics received 1089 citations as per Google Scholar report
Clinical Pharmacology & Biopharmaceutics peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Psychotropic prescription patterns for inpatients with schizophrenia: 10-year comparison in a university-affiliated Hospital in South Korea
3rd International Conference on Clinical Pharmacy
Jisang Byun and Daeho Kim
Hanyang University Medical School & Center, South Korea
Posters-Accepted Abstracts: Clin Pharmacol Biopharm
Abstract
Objective: The literature on the prescription change among patients with schizophrenia from real-world setting is scarce. And most of studies investigated only antipsychotic use. Given the polypharmacy is a routine process in clinical practice, we examined the patterns of all psychotropic medications from a psychiatric inpatient unit of university-affiliated hospital. Methods: All admission records at a psychiatric unit of Hanyang University Guri Hospital with discharge diagnoses of schizophrenia during two different five-year time frames (1997-2000 and 2006-2010) were reviewed. We investigated the socio-demographic and clinical data and discharge medications. The data were gathered from a total of 207 patients (95 in 1990ΓΆΒ?Β?s and 112 in 2000ΓΆΒ?Β?s). Results: The frequency in use of atypical anti-psychotics (98.2% vs 62.1%, chi square=44.7, p<0.01), anti-depressants (8.9% vs. 1.1%, chi square=6.3, p<0.05), beta-blockers (33.0% vs. 15.8%, chi square=8.1, p<0.01), and benzodiazepine (41.1% vs. 20.0%, chi square=10.6, p<0.01) were significantly higher in 2000ΓΆΒ?Β?s. Anticholinergic drugs were less likely used in 2000ΓΆΒ?Β?s (58.9% vs. 76.8%, chi square=7.5, p<0.01). We did not find significant differences in the equivalent dose of antipsychotic drugs, the use of mood stabilizers and cholinergic drugs between two time frames. Conclusion: Increased proportion of atypical antipsychotics and decreased use of anti-parkinsonian drugs are in line with literature. And our results show that more diverse classes of psychotic medications are used for schizophrenia in recent years. It is likely that psychiatrists are becoming more conscious of negative symptoms, anxiety, and depression as well as positive symptom of schizophrenia.Biography
Email: bjisang@naver.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi