Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
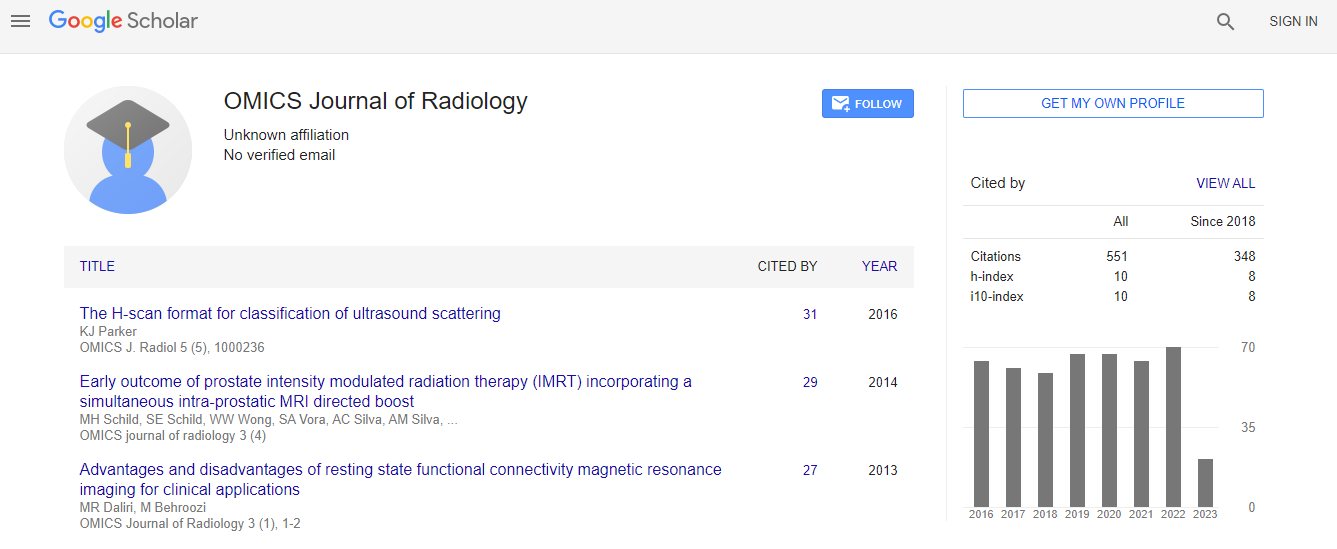
Google Scholar citation report
Citations : 551
Journal of Radiology received 551 citations as per Google Scholar report
Journal of Radiology peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Share This Page
Prognostic significance of magnetic resonance imaging in patients with severe nonpenetrating traumatic brain injury requiring decompressive craniectomy
2nd World Congress on Radiology and Oncology
Ravi Ambati, Kwok M Ho and Stephen Honeybul
Royal Perth Hospital, Australia
ScientificTracks Abstracts: OMICS J Radiol
Abstract
Background: Diffuse Axonal Injury (DAI) detected on Magnetic Resonance Imaging (MRI) may be useful to predict outcome after Traumatic Brain Injury (TBI). Aim & Method: This study compared the ability of the International Mission for Prognosis and Analysis of Clinical Trials (IMPACT) prognostic model with DAI on MRI to predict the 18-month neurologic outcome in 56 patients who had required decompressive craniectomy after TBI. Results: Of the 56 patients included in the study (19 scans occurred within 14 days, median time for all patients 24 days, interquartile range 14-42), 18 (32%) had evidence of DAI on the MRI scans. The presence of DAI on the MRI Diffusion- Weighted (DW) T2*-weighted gradient echo and Susceptibility-Weighted (SWI) sequences was associated with an increased risk of unfavorable outcome at 18 months compared with patients without DAI (44% vs. 17%, difference = [ 27%, 95% confidence interval 2.4-46.7% ; P = 0.032), particularly when the brainstem was involved. However, neither the grading (1 to 4) nor the number of brain regions with DAI was as good as the IMPACT model in discriminating between patients with unfavorable and favorable outcomes (area under the receiver operating characteristic curve: 0.625 and 0.621 vs. 0.918, respectively; P<0.001 for both comparisons). After adjustment for the IMPACT prognostic risks, DAI in different brain regions and the grading of DAI were also not independently associated with unfavorable outcome. Conclusion: The prognostic significance of DAI on MRI may, in part, be captured by the IMPACT prognostic model. More research is needed before MRI should be routinely used to prognosticate the outcomes in patients with TBI requiring decompressive craniectomy.Biography
Ravi Ambati is a medical doctor at Department of General Surgery, Royal Perth Hospital, Australia.
E-mail: kwok.ho@health.wa.gov.au

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi