Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
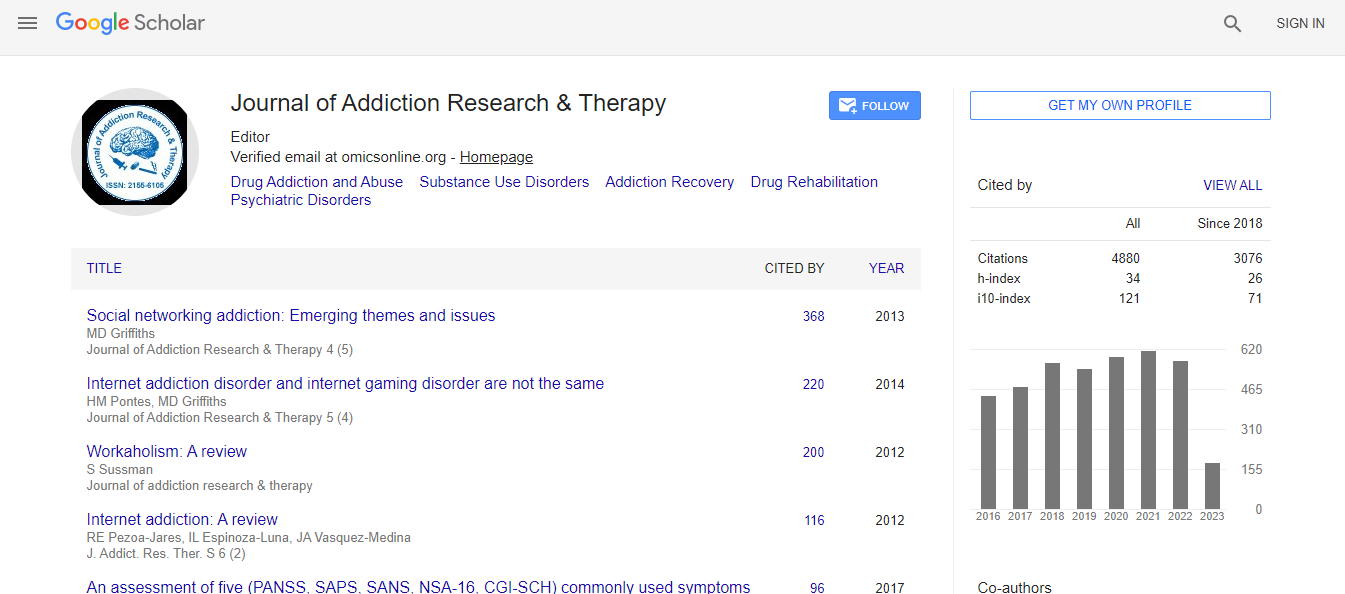
Google Scholar citation report
Citations : 4859
Journal of Addiction Research & Therapy received 4859 citations as per Google Scholar report
Journal of Addiction Research & Therapy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- SafetyLit
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Patient dropout from opioid substitution treatment
9th International Conference on Addiction & Psychiatry
Sohail Akhtar
Waikato District Health Board, New Zealand
Keynote: J Addict Res Ther
Abstract
Opioid Substitution Treatment (OST) is an established treatment for opioid dependence. In New Zealand, OST programs are regulated by the Ministry of Health and Methadone and Buprenorphine/Naloxone (Suboxone) are the primary medications. Retention on OST is a key indicator for stabilization of patients with opioid dependence. As yet, there have been no studies exploring the factors associated with New Zealand OST patient dropout, which is defined as discontinuation of OST by patients, against medical advice, for at least one month. Previous studies have showed that patients who drop out of treatment have a higher risk of harm to themselves by taking fatal overdoses and to society by engaging in criminal activities. Previous research has demonstrated that the effectiveness of OST is strongly correlated with patient retention. The purpose of the present research was to study dropout rates and identify factors associated with the dropout of patients from OST at the Community Alcohol and Drug Service (CADS), Hamilton, from 1st January 2013 to 30th April 2014. It was a retrospective, longitudinal, quantitative study. A retrospective clinical audit of patients on OST was conducted. There were 150 patients on OST in Hamilton under the CADS team during the period of study. Nine patients dropped out during the study period. 64 patients were randomly selected from the remaining 141 patients who remained on treatment as a comparison group and for the study sample to be approximately half of the overall population of 150 patients. Time and resources were also factors in determining the size of the sample group. File review was conducted and potential predictors of dropout were identified. 35 independent variables were selected and dropout was the dependent variable. The statistical program SPSS 22 was used to analyze the data. Fisher’s exact test was used and four variables were identified as being associated with dropout, history of intravenous drug use, (Fisher’s exact p value=0.05) history of lifetime imprisonment (Fisher’s exact p value=0.05), other medications prescribed, (Fisher’s exact p value=0.04) and opioid type prescribed during the study, i.e. Methadone or Suboxone. Patients on Suboxone dropped out more than those on methadone, (Fisher’s exact p value=0.00). The overall dropout rate was 6%, which was less than the rates of 15-85% found in previous studies. The limitations of the study were that it was retrospective and the number of dropouts was small. Furthermore, only patient factors associated with dropout were included in the study and service factors were not included. Therefore, the results of the study should be interpreted with caution. There is scope for a future study with a larger sample size and the inclusion of service factors to validate the finding.Biography
Sohail Akhtar has completed his Medical degree from the University of the Punjab, Pakistan. He has completed the Psychiatric Training and was then a Diplomat in Mental Health from College of Psychiatrists of South Africa. He has worked as a Senior Medical Superintendent at Polokwane/Mankweng Hospital Complex and Thabamoopo Psychiatric Hospital in South Africa. He has also completed Post Graduate Diploma in Public Management from Regenesys School of Public Management, South Africa. He has worked as a Senior Medical Officer in Psychiatry in New Zealand, completed his Post Graduate Diploma in Addiction and Co- Existing Disorders from University of Otago New Zealand. He also completed Masters in Addiction from University of Otago. He is the Senior Medical Officer in Community Alcohol and Drug Service of Waikato District Health Board, Hamilton, New Zealand. He is a Member of RANZCP vocational CPD program and Member of National Association of Opioid Treatment Providers, New Zealand and contributed in drafting the National Guidelines of Opioid Substitution Treatment.
E-mail: akif_sohail@xtra.co.nz

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi