Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
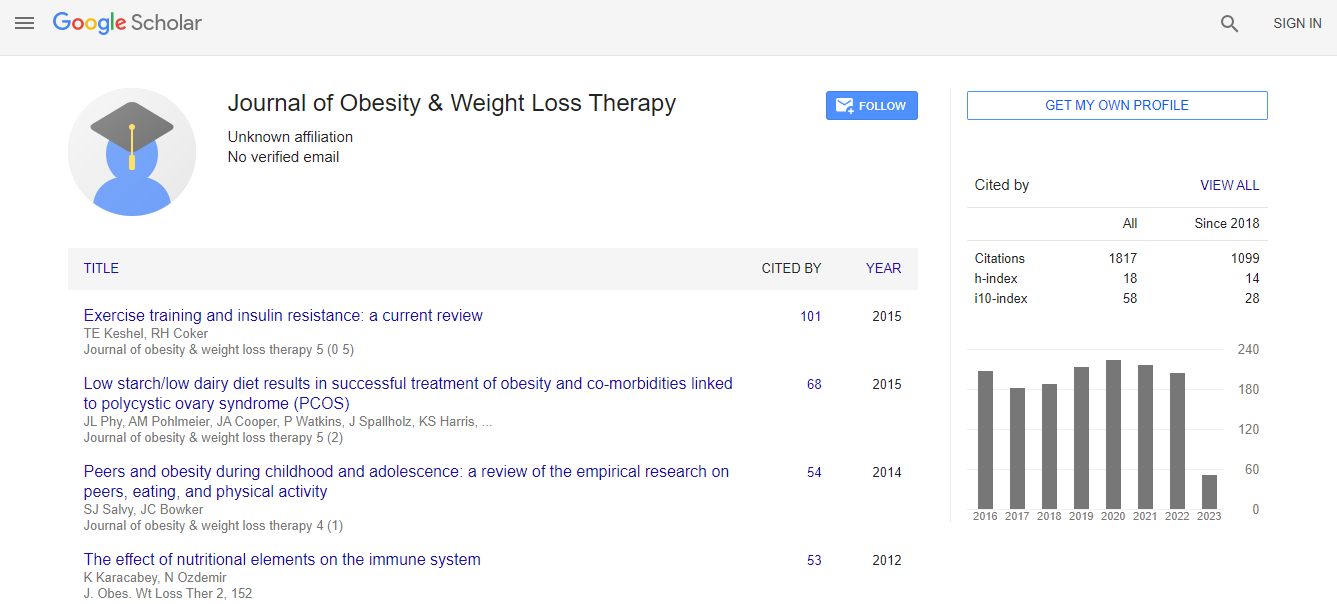
Google Scholar citation report
Citations : 2305
Journal of Obesity & Weight Loss Therapy received 2305 citations as per Google Scholar report
Journal of Obesity & Weight Loss Therapy peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- CABI full text
- Cab direct
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- University of Bristol
- Pubmed
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Obesity and severe Crohns disease
20th Global Obesity Meeting
Wita Tando, Haerani Rasyid, Mardiana Madjid
Hasanuddin University, Indonesia
Posters & Accepted Abstracts: J Obes Weight Loss Ther
Abstract
Background: About 15–40% of patients with IBD are obese, which might contribute to the development of IBD. Obesity is recognized as a state of chronic low-grade inflammation. There are two approaches that are suspected to link obesity to IBD that is the role of visceral adiposity “creeping fat” and dysbiosis. Visceral adiposity has been independently associated with increased risk of IBD-related complications and disease severity. Obesity might modify response to immunomodulator therapy in IBD. Case report: A 31 year-old man, was referred to us in September 2017 with Severe Crohn’s Disease with hematochezia. In 2013, he was diagnosed with Crohn’s Disease and his BMI was 28.6 kg/m2 (weight 78 kg). Before illness, patient used to consume traditional foods containing red meat, fried food and soft drinks. He rarely ate vegetables and fruits, and rarely exercise. In early 2017 patient were diagnosed with Chronic Kidney Disease on regular hemodialysis. His metabolic status was anemia, immune depletion, hypoalbuminemia, and electrolyte imbalance. On primary survey, his weight was 45 kg. Upper Gastrointestinal Endoscopy showed gastritis hemorrhagic. Lower Gastrointestinal Endoscopy revealed signs of severe Crohn’s disease, stricture, entero-colic fistula, and anal fissure. Nutritional therapy was given in order to meet energy requirement, considering the nutritional route and macronutrient composition also type of formula (polymeric vs elemental). Supplementation should be given to prevent micronutrient deficiencies, decrease inflammation and improve the immune system (vitamin D and zinc). After 34 days of nutritional therapy, the frequency of hematochezia was decreased, accompanied by increase of plasma albumin and lymphocyte count. Conclusion: Epidemiological studies, in particular prospective cohort study, implicating obesity in the development of IBD are limited, although there is an evidence from a pathophysiological perspective. This case report may encourage more prospective research about effects of obesity on incidence, course of disease, and treatment response to IBD and also the effect of obesity treatment to IBD outcomes. The aim of nutritional therapy in Crohn’s disease is to reduce inflammation, improve the immune system and intestinal homeostasis, also induce and maintain of remission.Biography
Wita Tando is Clinical Nutrition Specialist Program participant in Faculty of Medicine, Hasanuddin University, Makassar, Indonesia. She earned her Medical Doctor in 2007. She worked at Community Health Centre for 8 years, focus on prevention and treatment of non-communicable disease. In 2015, she enrolled in Clinical Nutrition Specialist Program at Hasanuddin University.
E-mail: witatando@gmail.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi