Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
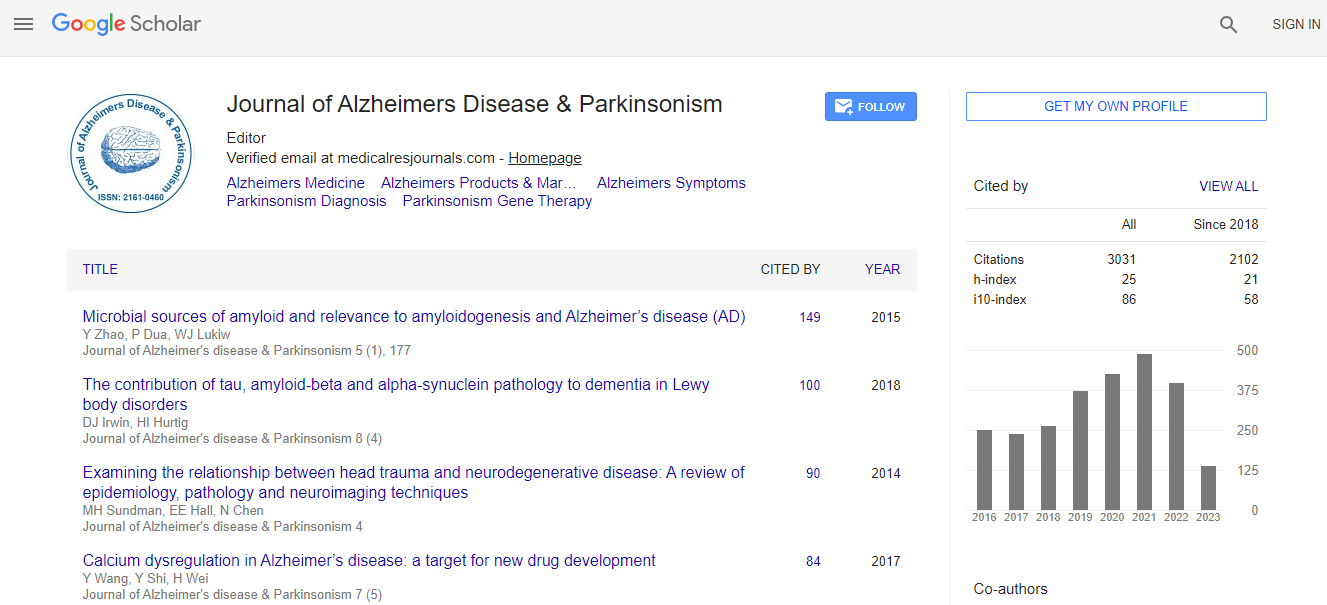
Google Scholar citation report
Citations : 4334
Journal of Alzheimers Disease & Parkinsonism received 4334 citations as per Google Scholar report
Journal of Alzheimers Disease & Parkinsonism peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Neuroprotective and Neurorestorative effects of disease-modifying single-domain Antibody fragments in Aged Beagles
5th International Conference on Alzheimer’s Disease & Dementia
Mourad Tayebi
The University of Melbourne, Australia
ScientificTracks Abstracts: J Alzheimers Dis Parkinsonism
Abstract
An active and promising area of research for Alzheimerâ�?�?s disease (AD) is immunotherapy using antigens (active) or antibodies (passive) that target AD neuropathology. Senile plaques contain the beta-amyloid (A�?²) peptide that is derived from a longer precursor protein, amyloid precursor protein. Amyloid beta is produced as either a 40 or 42 amino acid peptide, the latter being more fibrillogenic and toxic than the shorter isoform. Initially produced as a soluble peptide, A�?² subsequently can form oligomers, a molecular complex of monomer units. A�?² oligomers are highly toxic to neurons and particularly damaging to synapses. There is strong evidence that oligomer accumulation may seed plaque aggregation and serves as an early molecular target for preventing AD. Interestingly, oligomers can be detected by antibodies based upon structure with less of a need to target the amino acid sequence of an individual protein making antibody development for oligomers a fascinating area to pursue. Antibodies developed against oligomers may be able to bind several misfolded proteins implicated in neurodegenerative diseases. Immunotherapy studies have typically used transgenic mouse models of AD, and subsequently translated to human clinical trials. However, the success rate of these translational studies has been limited. In contrast, studies in another animal model, the aged canine, indicated that immunotherapy led to similar outcomes in AD clinical trials; reduced A�?² plaque pathology with no improvements in cognition but indications of a slowing of cognitive decline. We have previously developed and characterized unique anti-A�?² single domain antibodies derived from camelids. These antibodies, we called PRIOAD, were able to (i) cross the in vitro and in vivo blood brain brain (BBB) in mice rats and in vitro human BBB model; (ii) bind with high affinity to soluble oligomers derived from synthetic and native human A�?² but not their monomeric and fibrils counterparts; and (iii) not induce neurotoxic effects and host immune responses in mice. PRIOADs were evaluated for their therapeutic efficacy in a pilot sutdy using aged beagles with mild cognitive impairment. Following intraventricular infusion of PRIOAD for 3 months, there was a significant reduction of A�?² plaque burden in these animals. More importanly, PRIOADs led to reversal of the cognitive deficits in beagles. The study was very encouraging and will be expanded to include larger number of animal cohorts prior to translation into human clinical trials.Biography
Tayebi is a Senior academic at the University of Melbourne and heads the protein misfolding disease group. Dr Tayebi has previously very successfully led to startup biotechnology companies in the UK and the US.
Email: mourad.tayebi@unimelb.edu.au

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi