Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
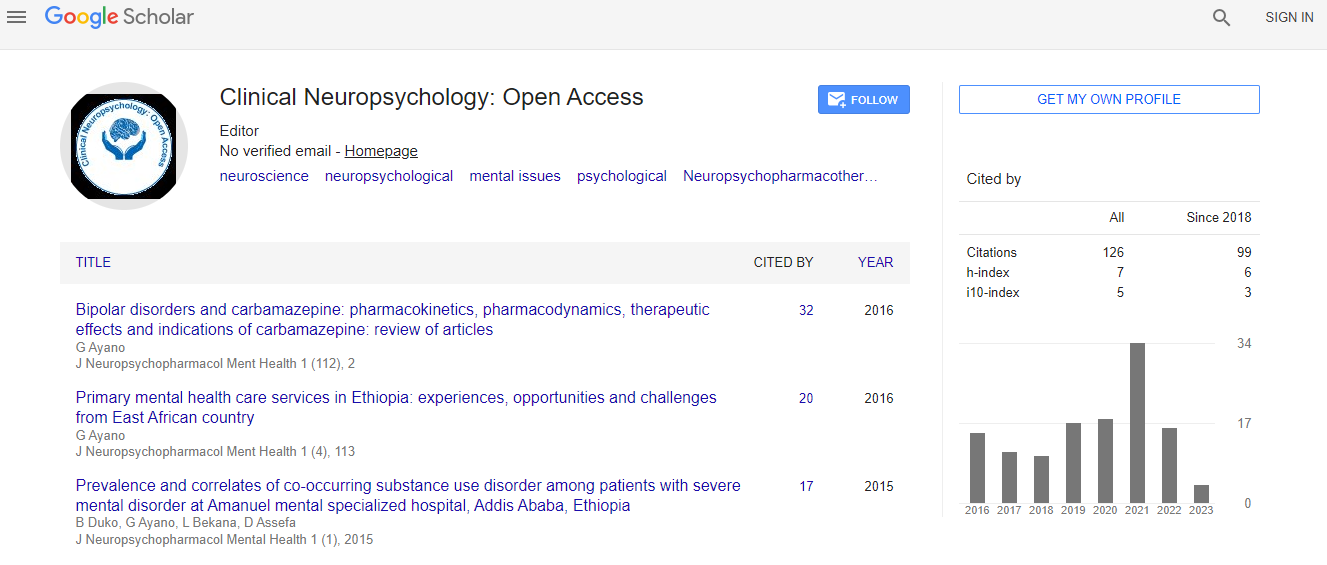
Google Scholar citation report
Citations : 141
Clinical Neuropsychology: Open Access received 141 citations as per Google Scholar report
Indexed In
- Google Scholar
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
Useful Links
Recommended Journals
Related Subjects
Share This Page
Neurophysiological monitoring during epilepsy in surgeries
8th Global Experts Meeting on Advances in Neurology and Neuropsychiatry
Sergio E Kosac
University of Buenos Aires, Argentina
Posters & Accepted Abstracts: ClinNeuropsychol
Abstract
Epilepsy surgery originates in the early 20th century since the discovery of functional areas, by Broca, Hitzog, and many others, on one hand. On the other hand, Jackson’s findings, describing the irritative cortical foci and proposing their excision, until the experiences of W Penfield, who generated a most complete functional cortical map, until that time, specifying motor and sensitive/sensorial areas, allowed surgical techniques to advance significantly. Nowadays, surgeries for reduction or elimination of cortical irritative foci are carried out in cases of: Cortical dysplasia, cortical tumors, vascular malformations, etc. Although more and more accurate and satisfactory surgical techniques were developed, in same cases it is imperative to preserve functional areas, whenever they are near or over the surgical area. To prevent or minimize damages to such functional areas, it is necessary to perform intraoperative neurophysiologic techniques. In cases of epilepsy surgeries, there are two ways: One is the electroencephalogram over the cortex, named electrocorticogram. The other one is the Neurophysiologic Intraoperative Monitoring (IOM). It is possible through a technique that applies somatosensory evoke potentials, recorded with a strip of electrodes. Through this technique, we can map out cortex areas, allowing the surgeon to know, before opening the dura, where those functional areas are. Another technique is, once motor and sensory areas are located to find some functions over and into the motor area more accurately. This is made with a stimulator given to the surgeon, connected to the neurophysiologist’ equipment, through which, we can map out more accurate areas i.e., hand area, leg area, etc., applying the stimulator over some points, and the neurophysiologist delivering stimuli to activate cortical motor neurons, and recording in the corresponding muscles.Biography
E-mail: Coolser_4@yahoo.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi