Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
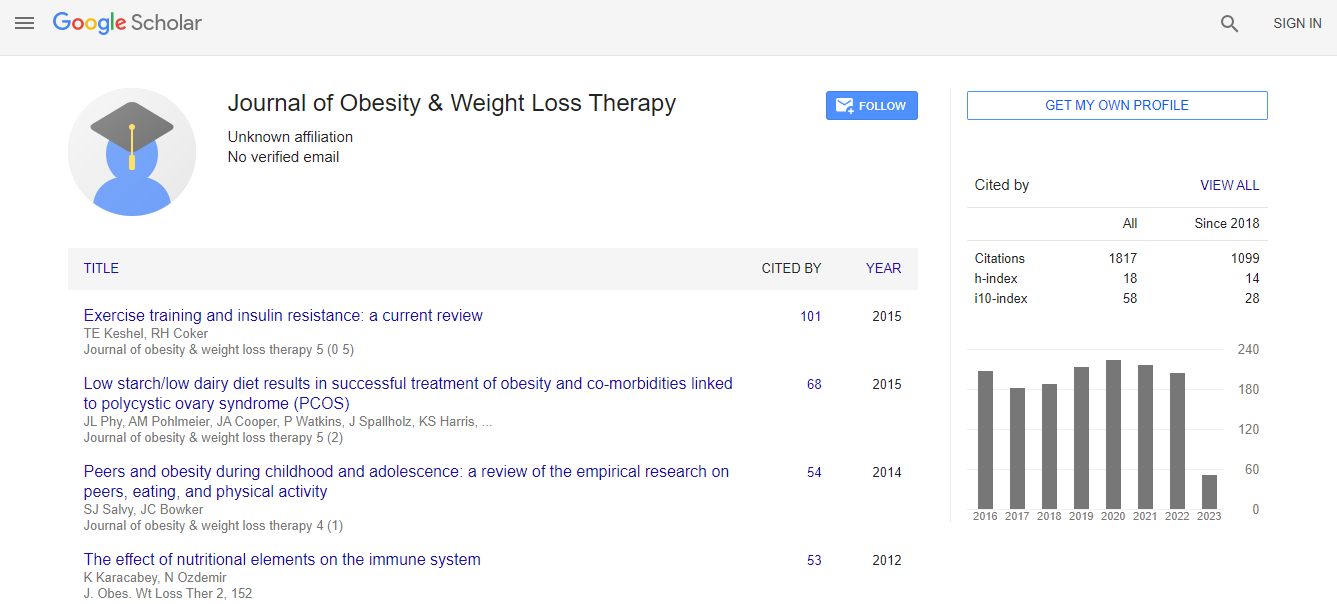
Google Scholar citation report
Citations : 2297
Journal of Obesity & Weight Loss Therapy received 2297 citations as per Google Scholar report
Journal of Obesity & Weight Loss Therapy peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- CABI full text
- Cab direct
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- University of Bristol
- Pubmed
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Multi-dimensional validated reporting of dysphagia post sleeve gastrectomy
JOINT EVENT 10th International Conference on Childhood Obesity and Nutrition & 2nd International Conference on Metabolic and Bariatric Surgery
Sukaina Jaffar and Michael Devadas
Nepean Hospital, Australia
ScientificTracks Abstracts: J Obes Weight Loss Ther
Abstract
Background: Few studies have reported the prevalence of dysphagia, as its own clinical entity in the bariatric population; without being examined under the umbrella of gastro-oesophageal reflux disease. This is compounded by studies not outlining methodologies used to assess dysphagia. Moreover, varying follow-up periods and different bariatric procedures have led to conflicting results. Objectives: To assess the prevalence of dysphagia using a statistically robust patient-reported tool, Dysphagia Handicap Index (DHI) post Laparoscopic Sleeve Gastrectomy (LSG). DHI is a validated tool which additionally measures the handicapping effects of dysphagia on emotional and functional domains of living. Methods: DHI questionnaire was administered to 124 patients who underwent LSG at least 1 year prior. Post-operative weight, change in BMI, percent Total Weight Loss (%TWL) and percent Excess Weight Loss (%EWL) were calculated. Physical, emotional and functional subscales were analyzed separately and altogether. Three additional questions were added to the DHI to delineate oesophageal dysphagia. Results: Average pre-operative weight and BMI is 123.8 kg and 43 kg/m2, respectively. Median %TWL and %EWL are 32% and 76.2%, respectively. An average reduction in BMI value of 14 kg/m2 was found. 41% of our cohort reported to mild dysphagia and 54% reported moderate to severe dysphagia based on the Modified DHI Score (DHI+Oesophageal Specific Dysphagia Score). No patient required corrective intervention. Patients reporting higher DHI scores were less likely to achieve the median TWL of 35.4 kg (OR 0.40, 95% CI 0.17-0.91). Dysphagia is a common symptom reported in our cohort and was found to have an impact on weight loss outcomes. Conclusion: Prospective, single-institution analysis using a validated tool reveals post-operative dysphagia to be a common clinical entity in our population with functional and psychological influences.Biography
Sukaina Jaffar is working as a Surgeon in Nepean Hospital, Australia. Sukaina Jaffar has participated in National and International conferences in the field of bariatric surgery and she has published many research articles in various International and National journals.
Email: jaffar.su@gmail.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi