Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
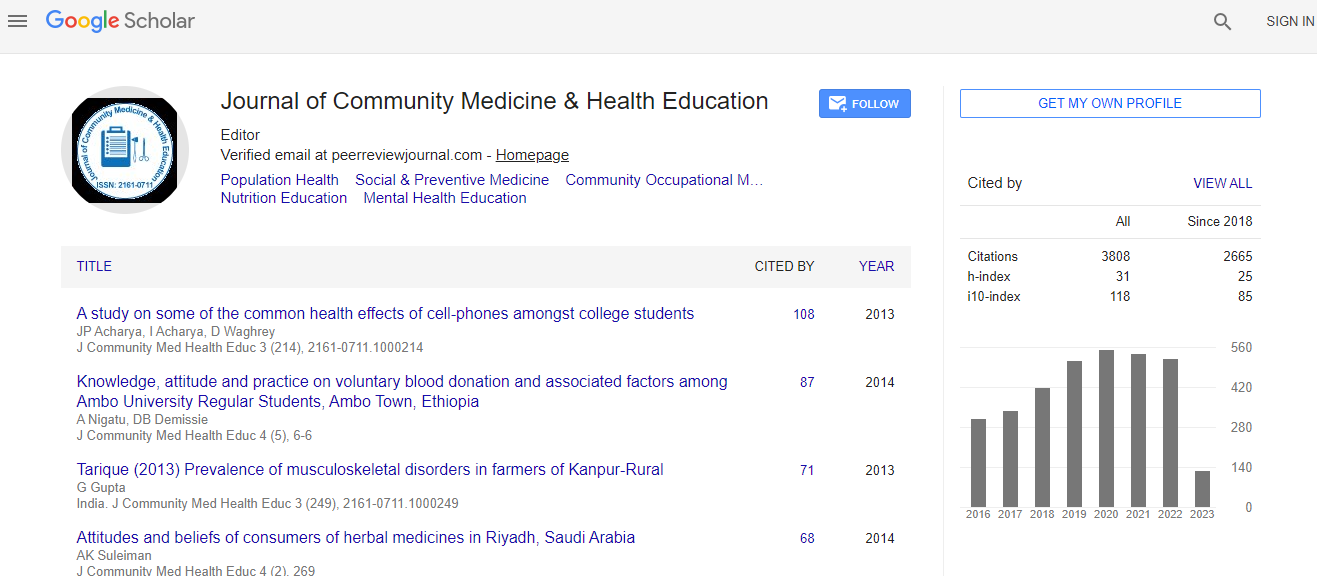
Google Scholar citation report
Citations : 5447
Journal of Community Medicine & Health Education peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Maternal birth preparedness and complication readiness remains low in low- and middle-income countries: a systematic review and meta-analysis of observational studies
3rd Global Summit on Public Health
Minyahil Tadesse Boltena
Public Health Faculty, Institute of Health, Jimma University, Ethiopia
ScientificTracks Abstracts: J Community Med Health Educ
Abstract
Background: The global maternal mortality rate due to preventable pregnancy related complications is 810 per 100, 000 live births. Poor maternal involvement in birth preparedness and complications readiness (BPCR) practice contributes to poor maternal and child health outcomes in low- and middle-income countries (LMICs). This systematic review and metaanalysis determined the pooled prevalence of maternal BPCR in LMICs. Methods: Literature published in English language from 2004 through 2022 was retrieved from CINAHL, EMBASE, Google Scholar, Scopus, PubMed, and Web of Science databases. Egger√ʬ?¬?s test and I 2 statistics were used to assess the publication bias and heterogeneity. The publication bias and heterogeneity was validated using the Duval and Tweedie√ʬ?¬?s nonparametric trim and fill analysis using the random-effect analysis. The summary prevalence and the corresponding 95% confidence interval (CI) of BPCR was estimated using random effect model. The review protocol has been registered in PROSPERO with registration code CRD42020213129. The steps to recruit eligible studies and reports of each section of the manuscript were described in PRISMA flow chart and PRISMA 2020 checklist. The Joanna Briggs Institute√ʬ?¬?s quality assessment tool for prevalence studies was used. STATA Version 16.0 was used to conduct the pooled meta-analysis. Results: Sixty one studies with a total of 44, 554 pregnant women and postpartum nursing mothers√ʬ?¬? were included. The pooled prevalence of maternal BPCR was 41%. Maternal arrangement of blood donor and knowledge of danger signs of pregnancy and postpartum complications were 15% and 42% respectively. Only 42% of pregnant women and mothers within 42 days of delivery of the baby arranged transport service to the health facility. Conclusions: Maternal BPCR remains low in LMICs. Maternal knowledge of dangers signs of pregnancy and postpartum complications, arrangement of transport service, and potential blood donor was low in LMICs. Health systems in LMICs must revise their health promotion policies and design evidence-based BPCR implementation strategy to enable active maternal involvement and improved community engagement in BPCR. Point of care access to blood and transport service during pregnancy and postpartum period must be improved to achieve better maternal and child health outcomes in LMICs.Biography
Minyahil Tadesse Boltena has completed his PhD in Evidence-Based Health Care and works as Knowledge Translation expert to the Ministry of Health of Ethiopia,Armauer Hansen Research Institute,Ministry of Health, Ethiopia.Evidence Based Health Care Centre: A JBI Center of Excellence, Public Health Faculty, Institute of Health, Jimma University, Ethiopia.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi