Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
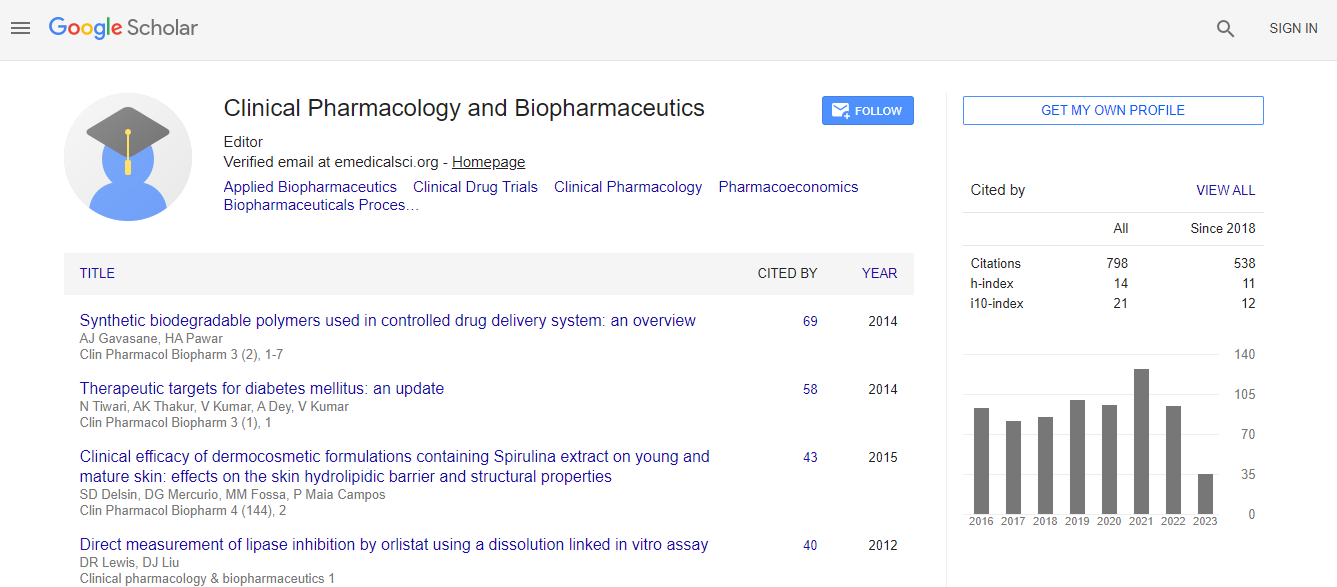
Google Scholar citation report
Citations : 1089
Clinical Pharmacology & Biopharmaceutics received 1089 citations as per Google Scholar report
Clinical Pharmacology & Biopharmaceutics peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Managing Drug Dosage in the ICU √¢¬?¬? is Augmented Renal Clearance what we really want to Know?
3rd International Conference on Clinical Pharmacy
Roger W Jelliffe
USC School of Medicine, USA
Keynote: Clin Pharmacol Biopharm
Abstract
Clearance (CL) is often felt to be the most physiologic parameter to describe elimination of substances from the body, and to be an independent parameter. However, there is an intimate relationship between CL, apparent volume of distribution (V) and the rate constant for elimination (K), in which CL = V times K, K = CL/V, and V = CL/K. Clearly none is independent. If one looks at general ways of describing similar systems, radioactive decay for example, there is no V, and K is the parameter giving accurate information about disappearance. In general, one can describe the behavior of a system as amount in a compartment, and the rate of movement from one compartment to another in terms of rate constants K. Observations of concentrations can be made as amount/V. CL is never needed. Further, since CL = KV, and since K has units of 1/time and V has units of volume, the units of CL are volume/time, and the actual information of rate of movement of drug becomes obscured when CL is used. However, V and K each give direct information about drug behavior. CL is not needed at all. CL is an unnecessary parameter. Further, since unstable ICU patients often have both rapidly changing renal function and unstable fluid balance at the same time, CL comingles and obscures the information of V and K, while V and K carry the needed information directly. This also facilitates separation of the two clinical issues of fluid balance and drug dosage for optimal management of these separate problems. Further, since ICU patients are so often unstable, conventional software for analyzing data of therapeutic drug monitoring (TDM) is no longer very useful, as it assumes that all the patent√¢¬?¬?s pharmacokinetic (PK) parameters are fixed and unchanging over the period of the data analysis. However, the interacting multiple model (IMM) algorithm developed in the aerospace community for tracking hostile targets most precisely has been developed [1] and implemented in the Bestdose clinical software [2] specifically to deal with this clinical situation. It tracks gentamicin and vancomycin in post-cardiac surgical ICU patients better than other methods [3]. It tracks changes in V and K as each new data point becomes available, resulting in the most recent Bayesian posterior parameter distributions. These then provide the foundation for dosage regimens to achieve desired target drug concentrations in the near future with maximum precision, using multiple model (MM) dosage design [4]. Illustrative clinical cases will be presented and discussed.Biography
Roger Jelliffe MD, FCP, FAAPS, developed the first computer software for individualizing drug dosage regimens in 1967. He was the first to relate renal drug elimination to creatinine clearance. He developed the first method for estimating creatinine clearance when serum creatinine is changing. He founded the USC Laboratory of Applied Pharmacokinetics in 1973, and the USC*PACK and more recent MM-USCPACK clinical software for individualizing drug dosage regimens most precisely. His laboratory developed the Resource for Population Modeling at the San Diego Supercomputer Center, the nonparametric adaptive grid (NPAG) population modeling approach, and Multiple Model (MM) design of maximally precise dosage regimens. This is now the Bestdose clinical and Pmetrics research software. We have developed three new methods of Bayesian analysis for individual patients. This adds great capability and safety in managing unusual patients. He is author or co-author of 132 peer reviewed publications, has mentored over 100 visiting scientific scholars, 1 sabbatical scholar, 2 Master’s Students, 3 Ph.D candidates, and 3 mini-sabbaticals.
Email: jelliffe@usc.edu

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi