Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
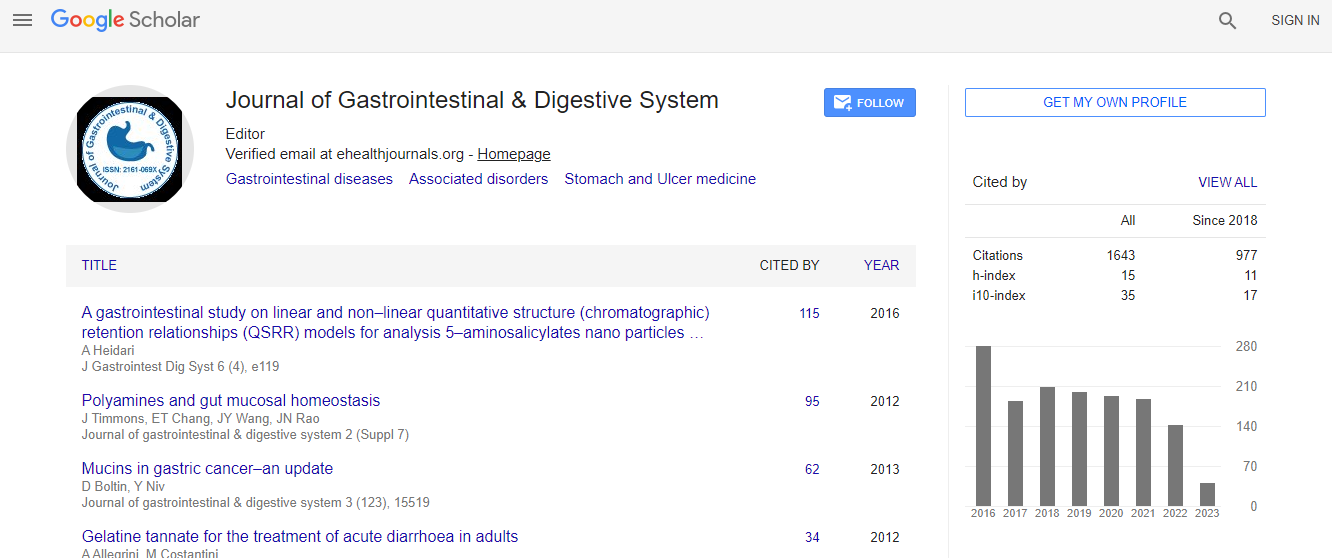
Google Scholar citation report
Citations : 2091
Journal of Gastrointestinal & Digestive System received 2091 citations as per Google Scholar report
Journal of Gastrointestinal & Digestive System peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Laparoscopic giant type IV hiatal hernia repair; my most difficult case: Video presentation
11th Global Gastroenterologists Meeting
Kece Can
Bahcesehir University, Turkey
Posters & Accepted Abstracts: J Gastrointest Dig Syst
Abstract
A 57-year-old man presented to the outpatient clinic with shortness of breath, dyspnea and vomiting. He noted that shortness of breath aggravated with exertion and after the ingestion of food. The patient did not describe an underlying chronic disease and did not use any medication within the previous six months. On the physical examination, vital signs were stable and no pathologic condition was observed. Blood analyses were found to be within the normal range. On the posteroanterior chest radiograph, there was an air-gas appearance that reflected the whole stomach on the chest. A thoracoabdominal CT scan including axial and coronal sections was performed in the patient because of the suspicion of a large hiatal hernia with available image. It was found that a large part of the stomach was herniated into mediastinum without any finding of incarceration. After three months of the operation, CT scan evaluation was performed again and no pathologic findings were observed (figure 1). Giant hiatal hernia is defined as greater than one third of the stomach in the thoracic cavity (chest) and representing 5 to 10% of all hiatal hernia. Although a uniform definition does not exist; most commonly with both the gastroesophageal junction and the fundus herniating through the hiatus. The fundus lies above the gastroesophageal junction. There are four types of HH. The current anatomic classification has evolved to include a categorization of hiatal hernias into Types I��?IV. Greater than 95% of hiatal hernias are Type I. Type IV hiatal hernias are characterized by the presence of a structure other than stomach, such as the omentum, colon or small bowel within the hernia sac. Although the cause for the development of hiatal hernia is unknown, its incidence increases by advancing age. Two potential mechanisms exist: Gastroesophageal reflux disease (GERD) leads to esophageal scarring and shortening with resulting traction on the gastroesophageal junction and gastric herniation; and chronic positive pressure on the diaphragmatic hiatus combined with a propensity to herniation leads to gastric displacement into the chest, resulting in GERD. Symptoms are often related to gastroesophageal reflux disease in the hiatal hernia which is usually asymptomatic. Asymptomatic hernia may not require any treatment, while multiple studies have supported the recommendation of early elective repair as a safer route in symptomatic patients. Repair of hiatal hernias has been performed traditionally via open laparotomy or thoracotomy. Since first laparoscopic hiatal hernia repair in 1992, this method has a growing popularity and today, it is the standard approach in experienced centers specialized for minimally invasive surgery. A successful repair of giant HH requires adherence to basic hernia repair principles i.e., hernia sac excision, tension-free repair, recognition and correction of a short esophagus, and a well-performed anti-reflux procedure. The laparoscopic approach for repair of large hiatal hernias is a relatively safe method with significant long-term efficacy in terms of symptom control and quality of life.Biography
Email: cankece@gmail.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi