Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
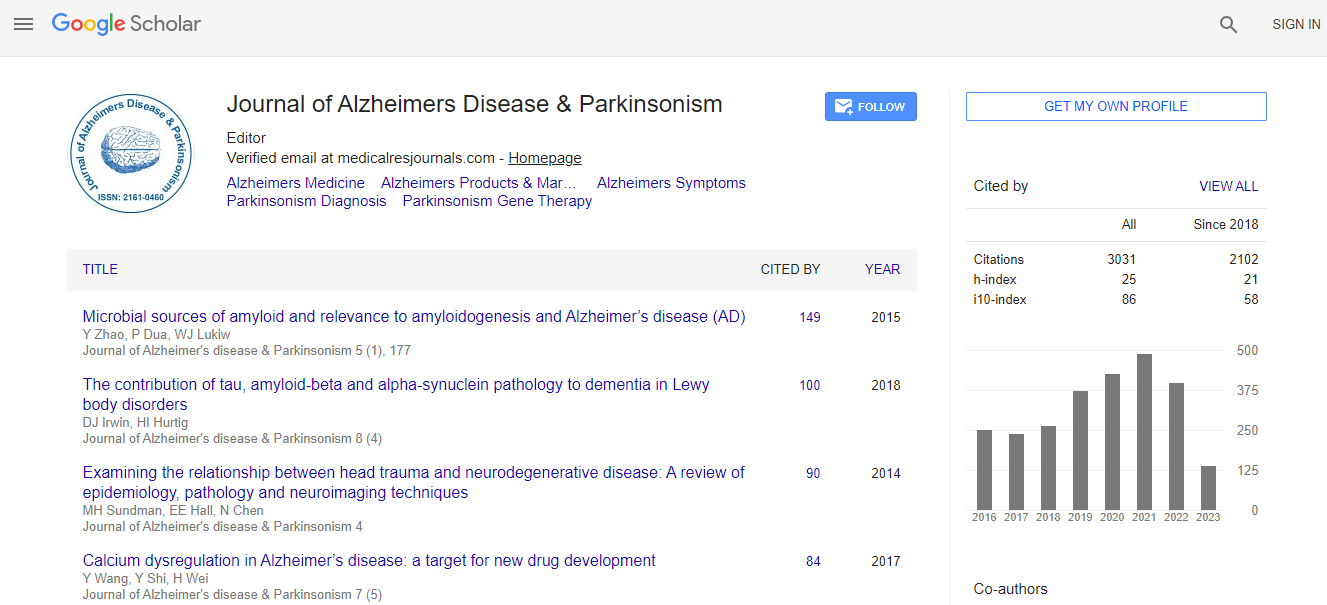
Google Scholar citation report
Citations : 4334
Journal of Alzheimers Disease & Parkinsonism received 4334 citations as per Google Scholar report
Journal of Alzheimers Disease & Parkinsonism peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Identifying neuropsychological profiles associated with white matter hyperintensities
3rd International Conference on Alzheimers Disease & Dementia
Jana Kynast, Leonie Lampe, Tobias Luck, Katrin Arelin, Dominik Fritzsch, Karl-Titus Hoffmann, Steffi G Riedel-Heller, Arno Villringer and Matthias L Schroeter
Max Planck Institute for Human Cognitive and Brain Sciences, Germany
Posters-Accepted Abstracts: J Alzheimers Dis Parkinsonism
Abstract
Background: White matter hyperintensities (WMH) feature as a marker of long-term white matter (WM) degeneration, caused by a broad range of pathologies. WMH can be detected on T2-weighted fluid attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) scans and progressively increase with age. Age-related WMH are strongly associated with vascular risk factors and are assumed to cause a global decline in cognitive performance. The progression of WMH majorly affects attention and executive functioning. However, a comprehensive, domain-specific characterization of the neuropsychological features associated with WMH is needed to validate recent findings and to further identify cognitive patterns associated with WMH. Aim: Here, we aim at the identification of neuropsychological characteristics associated with WMH in a large, non-clinical sample. Methods: We included 850 persons participating in the study of the Leipzig Research Centre for Civilization Diseases at the University of Leipzig, Germany (M = 60 years, SD = 13.1 years, range: 21-79 years). MRI was acquired for every participant with a 3 Tesla MRI-scanner. The amount of WMH on the individual FLAIR sequences was quantified on the 4-stage Fazekas scale (Fazekas, 1987) by experienced neuroradiologists. The sample was categorized in 4 Fazekas groups. Age, sex and education were identified as confounding factors. The neuropsychological test battery included the Trail Making Test (parts A and B), the Stroop Test, the Consortium to Establish a Registry of Alzheimerâ�?�?s Disease (CERAD) test battery and the 20-item Dysexecutive Questionnaire (DEX) of the Behavioral Assessment of the Dysexecutive Syndrome (BADS). Neuropsychological subtests were assigned to the cognitive domains attention, executive function, memory, learning, language, verbal fluency and perceptual-motor abilities, under wellestablished theoretical considerations and with respect to the clinical diagnostic criteria for mild and major neurocognitive disorder. Individual test results were age-standardized (M = 0, SD = 1) to the mean of the corresponding age group (<65 y, 66-69 y, 70-74 y, 75+ y). Age-standardized scores corresponding to the same cognitive domain were averaged to seven cognitive domain scores indicative of objective cognitive performance. A content based categorization of DEX items to five cognitive domains (attention, executive function, memory, language and social cognition) was applied. The sum score for every domain was age-standardized to the mean of the corresponding age group. Differences between the four Fazekas groups in (1) objective cognitive performance (7 measures) and (2) subjective cognitive complaint (5 measures) were analyzed with the nonparametric rank-sum test with data-alignment (critical alpha level: p < .05. Data was aligned for the effects of sex and education and their interaction with Fazekas score. Data was corrected for identical ranks. Group differences were examined using the single comparison algorithm proposed by Schaich&Hamerle. For single comparisons, the alpha level was adjusted due to multiple comparisons. Results: A general decline in cognitive performance is associated with a higher Fazekas score. The decline in cognition becomes evident with higher lesion load (starting at Fazekas score 2). Fazekas groups significantly differed in performance measures of attention (Ï�?�?²(3,846) = 13.77, p < .01) and executive functions (Ï�?�?²(3,846) = 12.84, p < .01). Analyses yielded marginally significant group differences in objective measures of memory (Ï�?�?²(3,438) = 7.74, p = .05) and visuo constructi veabilities (Ï�?�?²(3,434) = 7.73, p = .05). In all four cognitive domains, performance significantly declines with larger WM lesion load (Fazkasscore 2), while low lesion load (Fazekas score 1) was not associated with a decline in cognitive performance. Fazekas groups significantly differed in measures of memory complaint (Ï�?�?²(3,796) = 18.8, p < .001) and complaint on executive function (Ï�?�?²(3,796) = 39.88, p < .001). For both measures, persons with low lesion load (Fazekas score 1) worried significantly less than healthy persons (Fazekas 0) and persons with larger lesion load (Fazekas score 2, 3).Conclusion: Results show a substantial decline in cognitive performance with larger lesion load, which becomes evident at progressed stages of WMH (starting from Fazekas score 2). In line with recent literature, attention and executive function are assumed to be major dimension of cognitive decline. Furthermore, results suggest that small, punctual lesions (Fazekasscore 1) are less likely to be associated with impaired cognitive performance. A similar relation has also been found for subjective cognitive performance. Memory and executive functions are majorly affected by WMH and correspond to the results of objective cognitive performance. Surprisingly, persons with small WM lesions tend to be less worried about their cognitive performance than healthy persons. However, larger lesion load (Fazekas score 2 & 3) was associated with increased subjective complaint. This large cohort study contributes to the framework of age related WM changes and their association with domain specific cognitive performance and subjective cognitive complaints.Biography
Jana Kynast has completed her BA and MA in Psychology at the age of 25 years from the University Of Leipzig, Germany. In 2014 she became a fellow of the International Max Planck Research Network on Aging and started her PhD at the Max Planck Institute for Human Cognitive and Brain Sciences in Leipzig. Her research interests are the neuropsychology of mild cognitive impairment and dementia as well as its relation to neuroimaging and genetic biomarkers of dementia and dementia
Email: prestages. kynast@cbs.mpg.de

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi