Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
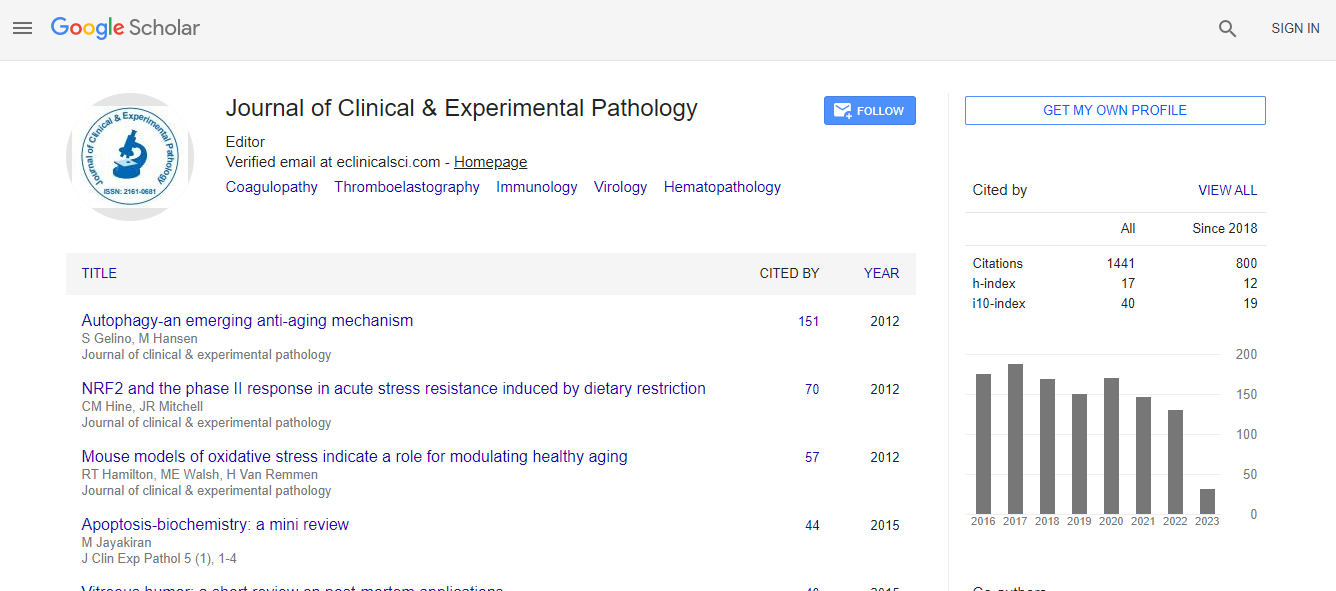
Google Scholar citation report
Citations : 2975
Journal of Clinical & Experimental Pathology received 2975 citations as per Google Scholar report
Journal of Clinical & Experimental Pathology peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Cosmos IF
- Ulrich's Periodicals Directory
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
- world cat
- journal seek genamics
- j-gate
- esji (eurasian scientific journal index)
Useful Links
Recommended Journals
Related Subjects
Share This Page
Histopathological findings in surgically resected treatment-resistant epilepsy cases
Joint Event on 15th International Congress on American Pathology and Oncology Research & International Conference on Microbial Genetics and Molecular Microbiology
M Ozge Tepe, Ozan Hasimoglu, Candan Gurses, Altay Sencer and Bilge Bilgic
Istanbul University, TurkeyMazhar Osman Bakirkoy Psychiatry and Neurological Diseases Research and Training Hospital, TurkeyKoc University, Turkey
Posters & Accepted Abstracts: J Clin Exp Pathol
Abstract
Statement of the Problem: In treatment-resistant epilepsy, different etiologies, histomorphological and immunohistochemical features, and diseases are included. Hippocampal sclerosis and focal cortical dysplasia are the most common histopathological diagnosis while tumor, vascular malformation, encephalitis, and glial scar are featured in decreasing frequency. Hippocampal sclerosis and focal cortical dysplasia are histopathologically classified according to the International League Against Epilepsy (ILAE) classifications. Molecular genetic studies in recent years have been effective in determining targeted therapies in patients who do not respond to antiepileptic drugs. mTOR pathway and immune system activation have been shown to play a role in epileptogenesis. To determine the incidence of different etiologies in the treatment-resistant epilepsy patients and find out histomorphological and immunohistochemical features and to demonstrate the relationship between the ILAE subtypes and the clinical features and try to predict the prognosis of the patients were main purposes in the neuropathological examination of our surgically resected treatment-resistant epilepsy cases. Methodology & Theoretical Orientation: In addition to immunohistochemistry (NeuN, Neurofilament-H, CD34, GFAP, IDH-1, and Olig-2) was performed in the diagnostic process, pS6 was used to demonstrate mTOR pathway activation in FCD cases and CD3, CD8, Iba-1 antibodies were applied to demonstrate neuroinflammation in HS cases. Findings: Statistical analysis of HS and FCD, were the most frequent histological findings, revealed a significant difference in age of seizure onset, epileptic seizure duration, surgical age, gender status, and Engel classification. pS6 expression was observed in dysmorphic neurons and balloon cells in the cases of FCD type II while lymphocyte infiltration was seen in all HS cases. Conclusion & Significance: Significant pS6 expression in FCD type II indicates that mTOR pathway inhibitors may be involved in the treatment of epilepsy. In HS cases, no statistical significant pathological feature to predict efficacy of immunomodulating therapy in a special subgroup has been identified.Biography
M Ozge Tepe graduated from Istanbul University, Istanbul Faculty of Medicine at the age of 24 years. She has trained in medical pathology during her residency since 2014.
E-mail: m.ozgetepe89@gmail.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi