Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
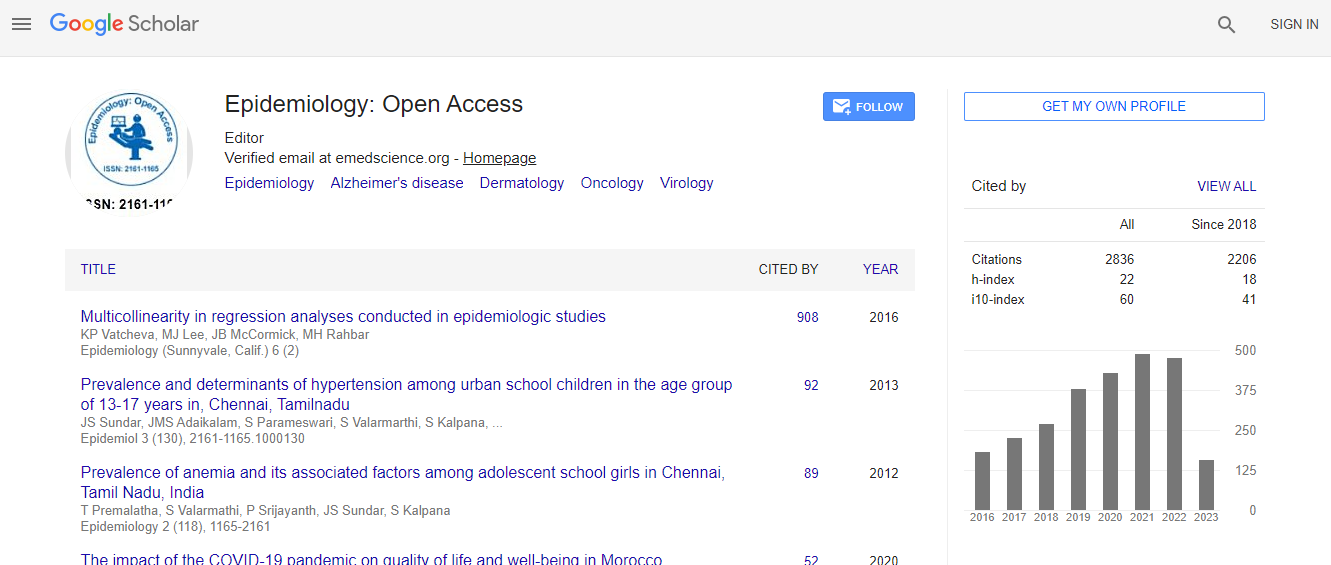
Google Scholar citation report
Citations : 3864
Epidemiology: Open Access received 3864 citations as per Google Scholar report
Epidemiology: Open Access peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- SafetyLit
- Access to Global Online Research in Agriculture (AGORA)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Cab direct
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
EXTENDED MOLECULAR EPIDEMIOLOGY OF ACUTE GASTROENTERITIS IN HOSPITALIZED CHILDREN AFTER ROTAVIRUS VACCINE IMPLEMENTATION IN TAIWAN
4th International Conference on Epidemiology & Public Health
Shih-Yen Chen
Chang Gung University College of Medicine, Taiwan
Posters & Accepted Abstracts: Epidemiology (Sunnyvale)
Abstract
Background: Rotavirus vaccine implementation has changed enteric virus infections in children. Objective: To investigate the change in viral acute gastroenteritis (AGE) and associated infections in hospitalized children in a longer time after rotavirus vaccine implementation. Design: During the period from January 2006 to December 2015, fecal samples from hospitalized children in Chang Gung Children√ʬ?¬?s Hospital with AGE were examined for enteric pathogens. Study period was divided into early post-vaccine (2006 Jan.-2010 Dec.) (EPV) and late post-vaccine (2011 Jan. -2015 Dec.) (LPV) periods. Setting: A tertiary children√ʬ?¬?s medical center in northern Taiwan. Results: A total of 905 stool samples were collected from hospitalized patients with AGE including 441 in EPV and 464 in LPV. In EPV period, enteric pathogens were identified in 318 (72.1%) including 113 (25.6%) rotavirus, 107 (24.3%) norovirus as major pathogens; In LPV periods, detection ratio of 315 (67.9%) with major infections of 88 (19 %) rotavirus and 107 (23.1%) norovirus. Statistical analysis showed a significantly decreased prevalence of rotavirus infection (P = 0.016) and a significantly increased prevalence of enteric bacteria infections (P < 0.001). Norovirus has outnumbered rotavirus (23.1% vs 19%) as the most common viral pathogen acute gastroenteritis. Rotavirus genotyping demonstrated a significant decrease of G1 (P=0.0002) in LPV compared to that of EPV. Norovirus GII.4 were the most predominant genotype in both periods with the commonest of GII.4 2006 b strain (35 of 59, 59.3%) in EPV and GII.4 2012a Sydney strain (29 of 65, 44.6%) in LPV period. Among vaccinated patients with AGE, norovirus is the most common etiology and there was relatively lower prevalence rotavirus infection in LPV with common genotypes of G1, G2, and G3. Conclusions: In Taiwan, under a suboptimal rotavirus vaccination policy, rotavirus infection caused hospitalization AGE is definitely decreased and norovirus has replaced rotavirus as the leading cause for hospitalized children with AGE. Enrichment of rotavirus vaccine coverage, development of norovirus vaccination, and sustained bacterial infections control important for infection containment and hospital care in Taiwan.Biography
Shih-Yen Chen is currently an attending physician in the Department of Pediatrics, Chang Gung Children’s Hospital and Chang Gung University, Taoyuan, Taiwan. He received his Doctor of Medicine degree from Taipei Medical College, and Doctor of Philosophy degree from Chang Gung University College of Medicine. He obtained his postdoctoral fellowship training from the Division of Pediatric Gastroenterology and Hepatology, Chang Gung Children’s Hospital. His research interests include pediatric gastrointestinal infection and molecular epidemiology of viral gastroenteritis.
Email: csy001@adm.cgmh

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi