Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
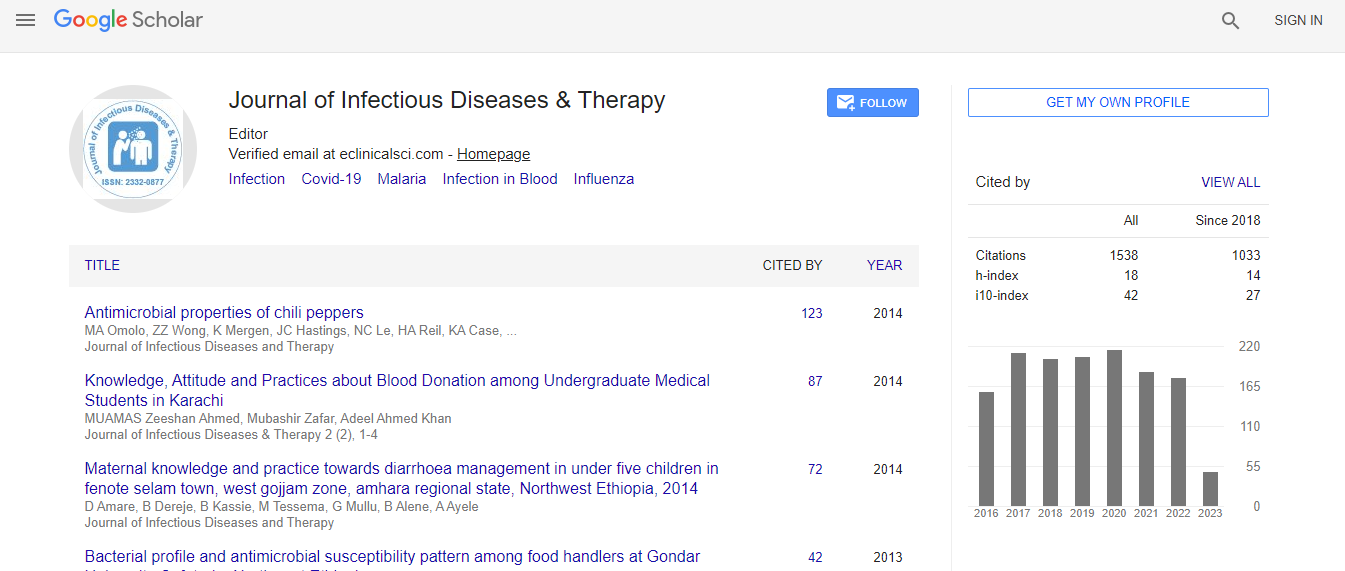
Google Scholar citation report
Citations : 1529
Journal of Infectious Diseases & Therapy received 1529 citations as per Google Scholar report
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Drug delivery by tattooing to treat cutaneous leishmaniasis
4th World Congress on Infection Prevention and Control
Stef Stienstra
Dutch Armed Forces/Royal Dutch Navy, Netherlands
Keynote: J Infect Dis Ther
Abstract
Background: Leishmaniasis is a vector borne disease that is caused by obligate intra macrophage protozoa of the Leishmania species. Leishmaniasis can cause different clinical syndromes including cutaneous leishmaniasis (CL), in which the patient generally presents with one or several ulcers or nodules on the skin, resulting from the infection of phagocytic cells located in the dermis. It often results into severe scar tissue in the skin. Most of the twelve million people infected with Leishmania worldwide are CL cases and 1.5 million new cases occur annually. Objective: WHO has a program to develop new treatments for cutaneous leishmaniasis. This study establishes a proof of concept that a tattoo device can target intra dermal drug delivery against cutaneous leishmaniasis (CL). Methods: The selected drug is oleylphosphocholine (OlPC) formulated as liposomes, particles known to be prone to macrophage ingestion. First it is shown that treatment of cultured Leishmania infected macrophages with OlPC liposomes results in a direct dose dependent killing of intracellular parasites. Based on this, in vivo efficacy is demonstrated using a 10 day tattooing mediated treatment in mice infected with L. major and L. mexicana. In both models this regimen results in rapid clinical recovery with complete regression of skin lesions by Day 28. Parasite counts and histopathology examination confirm high treatment efficacy at the parasitic level. Low amount of drug required for tattooing combined with fast clinical recovery may have a positive impact on CL patient management. Results: This first example of tattoo mediated drug delivery could open to new therapeutic interventions in the treatment of skin diseases. This study demonstrates that the use of a tattoo instrument for drug delivery is possible in the treatment of cutaneous leishmaniasis and that this method can successfully eliminate intracellular parasites at the site of infection. After showing that the selected drug oleylphosphocholine (OlPC) formulated as liposomes could efficiently reach intracellular parasites when in contact with infected macrophages, the activity of the drug was compared in vivo in mouse models of Old (L. major) and New World (L. mexicana) leishmaniasis. Three routes of administrations of the same drug formulation were investigated: Systemic (IP) administration, topical administration as a drop and administration via the tattoo instrument. Evaluation parameters included clinical (lesion sizes) and parasitological parameters (burdens) using quantitative and qualitative methods. In all experiments, the tattooing delivery procedure was the most efficacious at both the clinical and parasitological levels. Limitations: The used tattoo device, used routinely for permanent makeup procedures is not yet optimal for quantitative drug delivery.Biography
Stef Stienstra is a strategic and creative Consultant in Biomedical Science with a parallel career as a Commander of the Reserve of the Royal Dutch Navy. For the Dutch Armed Forces he has responsibility for the counter measures in CBNRe threats and (medical) consequence management both in a military and a civilian (terrorism) setting. In his civil career he works internationally as a Consultant or as Scientific Supervisory Board Member for several medical and biotech companies, merely involved in biodefense. He is also a Visiting Professor for Punjab University in Pakistan and Rhein-Waal University in Germany. He has completed his studies in Medicine and in Biochemistry at the University of Groningen in Netherlands and has extensive practical experience in cell biology, immuno-hematology, biodefense and transfusion medicine.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi