Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
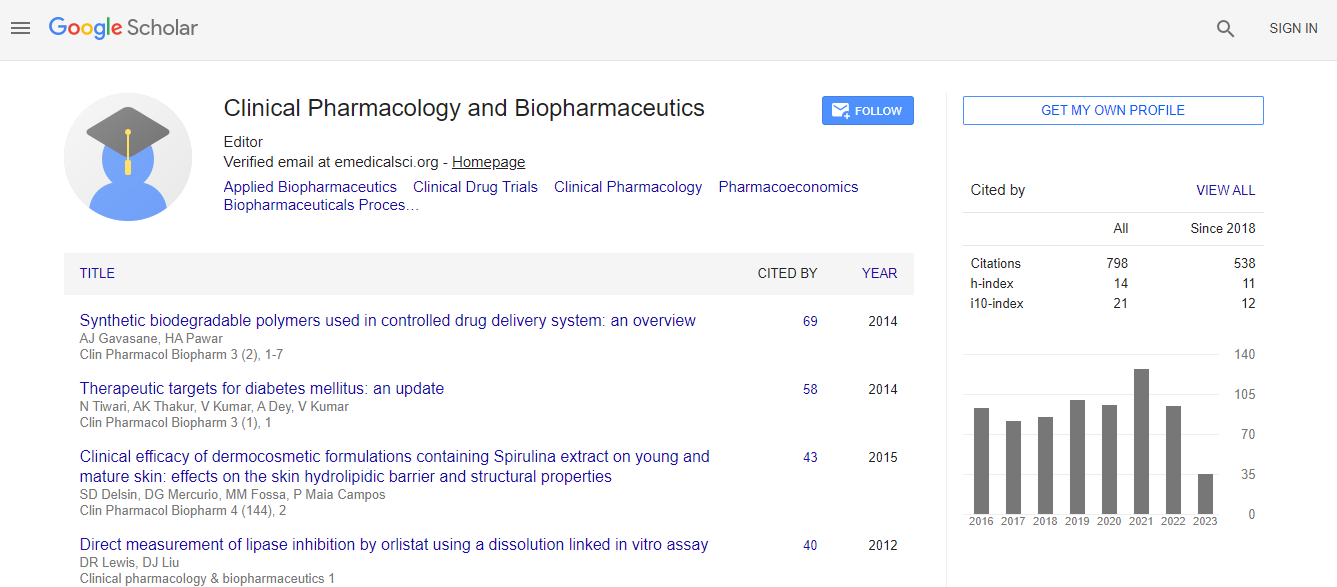
Google Scholar citation report
Citations : 1089
Clinical Pharmacology & Biopharmaceutics received 1089 citations as per Google Scholar report
Clinical Pharmacology & Biopharmaceutics peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Development Of Preeclampsia In A Pregnant Patient With FMF
International Conference and Expo on Biopharmaceutics
Oznur Kal1 and Emel Ozc├?┬▒men2
1Baskent University Medical Faculty Department of Nephrology, Turkey 2Baskent University Medical Faculty Department of Gynecology, Turkey
Posters-Accepted Abstracts: Clin Pharmacol Biopharm
Abstract
Introduction: Familial mediterrean fever (FMF) is an autosomal recessive disease characterized by recurrent self limiting attacks of fever, serositis ( like peritonitis, arthritis, pleuritis) and eryzipelas-like skin lesion. The disease is common among Turks, Armenians, Arabs and non askanazy Jews. FMF may cause amyloidosis which affects the kidneys but may also be accumulated in other organs such as the heart, gastrointestinal tract, and reproductive organs. Case: 30 years old female patient with a diagnosis of FMF is followed for ten years and using colchicine regularly and no nefropathy and amyloidosis history. Patients had an unknown cause infertility and became pregnant after the fourth in vitro fertilization (IVF). The patients blood pressure was increased at the 36th week of pregnancy and she had taken cesarian section. The patient was considered as preeclampsia and she had 300 mg/day proteinuria. After cesarean blood pressure and the proteinuria was back to normal within two months. Discussion: In the literature search we found only 1 case with FMF during pregnancy and complicated with preeclampsia. The course of disease in female FMF patients during pregnancy is variable. Some patients have an attack free period during pregnancy and still other women may experience attacks with high frequency. Apart from the inconcience and the pain during the attacks there is an additional risk, because peritonitis may lead to uterine contractions with eventual abortions, early labor and delivery. During the pregnancy the onset of hypertension and proteinuria after 20 weeks gestation characterizes preeclampsia, a leading cause of maternal mortality. Preeclampsia has been recognized as a potentially fatal complication of pregnancy for more than a century. It complicates between %3 and % 10 of pregnancies and is responsible for a large partion of maternal and perinatal morbidity and death. Despite extensive research into the causes and pathogenesis of this condition, delivery of the fetus and placenta is still the only effective treatment. Conclusion: FMF may trigger preeclampsia during pregnancy. For us to be cautious in terms of preeclampsia during pregnancy in patients with FMF. Pregnant FMF patients without nephropathy and amyloidosis, should be followed closely for preeclampsia.Biography
Email: drozkanonal@selcuk.edu.tr

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi