Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
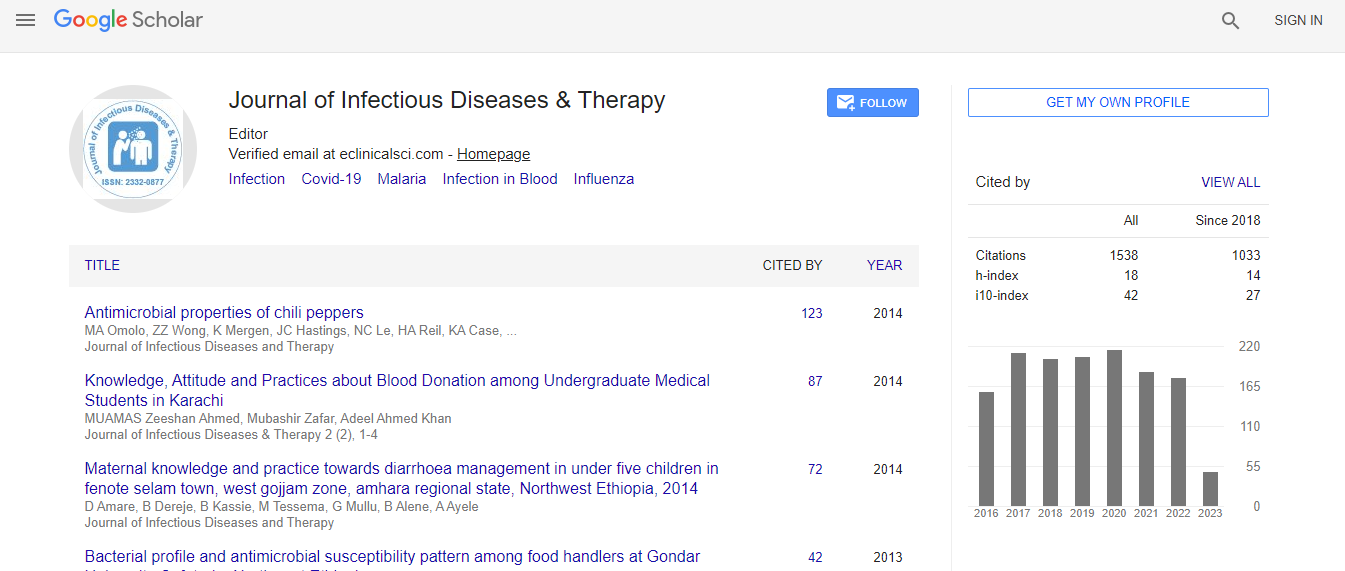
Google Scholar citation report
Citations : 1529
Journal of Infectious Diseases & Therapy received 1529 citations as per Google Scholar report
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Cytomegalovirus-Varicella Zoster Meningoencephalitis and Ischemic Stroke in an HIV-AIDS patient: A Case Report
4th International Congress on Infectious Diseases
Monica Pia P Reyes and Ryan M Llorin
St. Luke├ó┬?┬?s Medical Center Global City, Philippines
Posters & Accepted Abstracts: J Infect Dis Ther
Abstract
Along with the increasing number of newly diagnosed Human Immunodeficiency Virus (HIV) patients per day in the Philippines (26 new cases/day), an increasing number of HIV patients were diagnosed with Central Nervous System Infection (CNSI) and Stroke. A study shows that the risk of ischemic stroke was higher among those with HIV infection compared with uninfected people (hazard ratio 1.17). Mechanisms of ischemic stroke include HIV-associated vasculopathy, opportunistic infections or neoplasia, cardioembolism and coagulopathy. This case report aims to present a CNS co-infection of the three most documented viruses that causes stroke: Cytomegalovirus (CMV), Varicella Zoster Virus (VZV) and HIV. The inflammatory cascade in these infections promotes atherosclerosis, plaque rupture, and thrombosis, leading to ischaemic stroke. A 35-year-old male with HIV who was noncompliant with anti-retroviral therapy and who had recent untreated shingles was brought in with decreased sensorium, signs of meningeal irritation and right-sided neurologic deficit. Computed tomography scan revealed acute to sub-acute infarct, left middle cerebral artery territory (figure 1). Vancomycin, ampicillin, cefepime and ganciclovir were empirically started for central nervous system infection. HIV work-up revealed a CD4 of 11 cells/mm3 and HIV-1 RNA of 1,124,215 copies/mL. CMV IgG was positive at 65 U/mL. Lumbar tap done had an elevated opening pressure with elevated cerebrospinal fluid (CSF) protein, low-normal CSF glucose, and pleocytosis with lymphocytic predominance. Viral panel showed CMV viral load of 634,000 copies/mL and VZV IgG 44.4mIU/L clinching the diagnosis of concomitant CMV-VZV meningoencephalitis in an HIV patient. Magnetic resonance imaging and angiogram is compatible with viral vasculopathy (figure 2). The pathogenic mechanisms of VZV reactivation in the CNS include neuronal and glial direct infection and immune-mediated lesions including vasculitis and demyelinization while CMV infection of vascular smooth muscle cells induces production of powerful pro-inflammatory cytokines which accelerate atherosclerosis development. This seems to be the first reported case of co-infection of the CMV-VZV-HIV meningoencephalitis and ischemic stroke.Biography
Monica Pia P Reyes is a Diplomate of Philippine College of Physicians. She completed her Medical degree at University of the Philippines and; Internal Medicine Residency training at St. Luke’s Medical Center- Global City, Philippines where she was granted 2016 Excellence in Research Award. She is an incoming Infectious Disease Fellow at Philippine General Hospital. She has organized research forums and training workshops. Her research interest includes HIV/AIDS, Tuberculosis, and Critical Care Medicine.
Email: monicapiareyes@yahoo.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi