Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
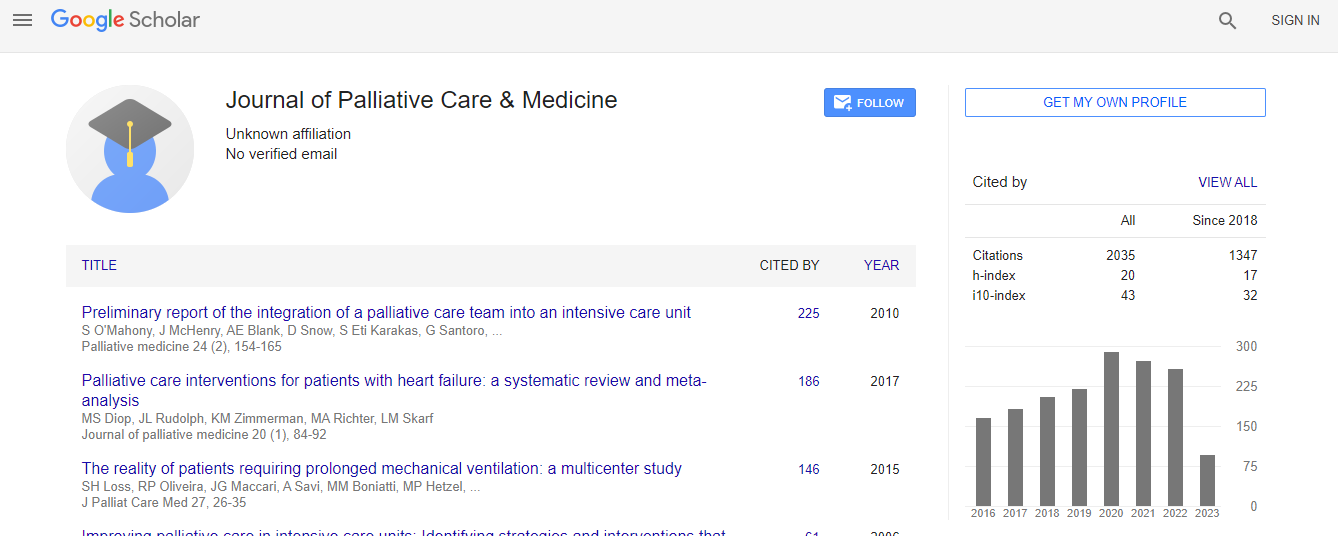
Google Scholar citation report
Citations : 1689
Journal of Palliative Care & Medicine received 1689 citations as per Google Scholar report
Journal of Palliative Care & Medicine peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Cytochrome p450: Why the same drugs used in palliative care do not work the same on everyone
International Conference on Hospice & Palliative Care
Stephen D Krau
Vanderbilt University Medical Center, USA
Posters-Accepted Abstracts: Posters-Accepted Abstracts
Abstract
Although the science related to variation in responses to medication has been developing for decades, the importance and practical application has not translated into clinical practice. The first step in improving outcomes related to individual medication response variation based on gender, and race, is in the examination of evidence that can result in strategies to provide effect medical care. For end of life care to be equitable, culturally congruent, and overall competent, this aspect of patient care demands consideration and illumination. Inter-individual variation in drug response poses a serious problem in the management of patients who are receiving medications to treat or prevent any disease or illness, or to provide comfort during end of life. Due to individual variations in response to drug therapy, this variability can result in toxicity and adverse drug reactions (ADRs). Major factors that account for differences in drug response include cultural practices, race (genetic composition), and gender. These factors merit consideration when determining which medication and dosage will provide appropriate treatment, or pain relief. Persons who are prescribing, administering, or taking medications can make the best decisions with regard to the most effective medication regimen, when they understand fundamental aspects of inter-individual variations and disparities in drug responses. One specific factor genetic factor that accounts for the variation in drug response is Cytochrome p450. Although knowledge about the impact of Cytochrome p450 on individual variations in drug response has been known for decades, the transition to clinical practice has not evolved. It is estimated that 90% of current prescribed medications are mediated by these enzymes that result in variations based on the individual├ó┬?┬?s phenotype. When considering cultural practices and racial differences, in many cases we are under medicating, overmedicating or using the wrong medication to achieve a specific outcome. For example, the mortality rate among African American women in the United States with breast cancer is unacceptable. This is in part due to the fact that clinical drug trials are done with primarily Caucasian females. Drug guidelines and doses established based on these data involving a predominant group. When medications that are effective in one racial group are given for same illnesses in another racial group, the medications can be not only ineffective, but detrimental. For competent and equitable palliative care, health care professionals have a responsibility to enhance knowledge of scientific data that supports variation based on race and gender. Only through recognizing the value of the evidence and it implications, can transcultural nursing related to medication prescription and administration truly be competent, skilled, and effective.Biography
Email: steve.krau@vanderbilt.edu

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi