Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
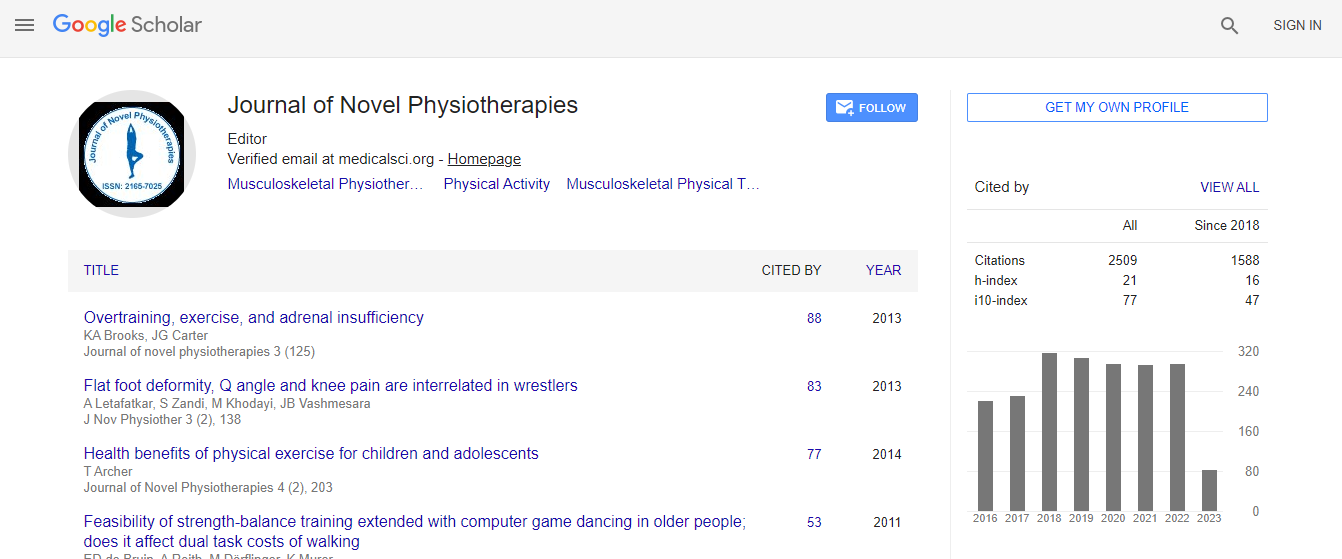
Google Scholar citation report
Citations : 3145
Journal of Novel Physiotherapies received 3145 citations as per Google Scholar report
Journal of Novel Physiotherapies peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Comparing low upper trapezius to lower trapezius ratio exercises, with cued electrical stimulation to exercises and sham stimulation, for a motor learning effect in scapular dyskinesis
2nd International Conference and Expo on Novel Physiotherapies
Walker DL, Hickey CJ and Tregoning MB
California State University, USA
Posters & Accepted Abstracts: J Nov Physiother
Abstract
Purpose/Hypothesis: Altered scapular motion and position, termed scapular dyskinesis, is commonly treated in physical therapy clinics and is often a component of shoulder pain. Conventional therapeutic exercise programs to treat dyskinesis address impaired muscle recruitment in an effort to normalize scapular-humoral rhythm. Treatment durations can range up to 12 visits with varying success. There are no studies that examine traditional therapeutic exercise programs with the addition of triggered electrical stimulation (ES) as a motor cue to relearn appropriate patterns of scapular movement. The purpose of this pilot study was to compare therapeutic exercise with an ES cue, to therapeutic exercise with a sham cue, to examine a motor learning effect in subjects with scapular dyskinesis. The hypothesis was that the ES group would be different in manual measures and in video inspection compared to the sham (non-stimulation) group. Subjects: 12 subjects (representing 15 scapulae) from a university campus sample of convenience, who met the inclusion criteria, were randomized into the ES or sham groups. Materials/Methods: Pre-data collection, intra-rater reliability for the manual measures was established (r=0.60). An expert clinician assessed for visual winging of the scapula at rest and during active flexion and abduction following an intake questionnaire. Subjects were video-taped and distance measurements were taken at (0�°, 45�°, 90�° and 120�° abduction) prior to treatment, referencing the ipsilateral-side of the thoracic spinous process and the medial aspect of the scapular inferior angle. Both ES and sham groups were given three exercises cited as having low upper trapezius/lower trapezius (UT/LT) ratios. Exercises were performed 4 times a week, 2 times independently and 2 times with the researchers using ES cueing or sham cueing. Electrical cueing was provided via a handheld switch. A biphasic-pulsatile current was used. The frequency and pulsewidth were 25 pps and 250 usec, respectively. The intensity was comfortable and produced scapular retraction. Results: Results indicated manual measurements of the scapular distance were consistent and not significantly different across the ES and sham groups at 0�° and 45�° degrees. No significant change was found across the control group for 90�° or 120�°. However, at 120�° the intervention group showed a significant difference in measurements (p=0.003). Mean results also showed that although the sham group started in better scapular positioning with 1.73 cm less excursion than the ES group (sham 8.44 cm and ES 10.17 cm), the ES groupâ��s post treatment end with a 2.76 cm change, and surpassed the control by a large margin. On-going preliminary video reviewing visually confirms this analysis. Conclusions: This quick, simple intervention (ES cue with three exercises) on subjects who started with poorer scapular positioning (at 120�°), yielded significant mean changes compared to subjects who were not electrically cued. In addition, consistency was noted on pre and post-test measures at 0�° and 45�° between treatment groups with the manual spinous process to inferior angle measurements. Clinical Merit: Greater change in scapular distance pre-to-post-test, at 120 degrees, following six, 20 minute treatments with ES cueing, can provide the busy clinician with a valuable means to facilitate improved motor learning in patients with scapular dyskinesis.Biography
Walker DL, PT, DPT, OCS, GCS has been a practicing Physical Therapist for 24 years. She is a faculty member at the Department of Physical Therapy and holds two clinical specialty certifications, one in orthopedics and one in geriatrics. One of her clinical areas of expertise is the upper quadrant and shoulder.
Email: dewalker@csufresno.edu

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi