Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
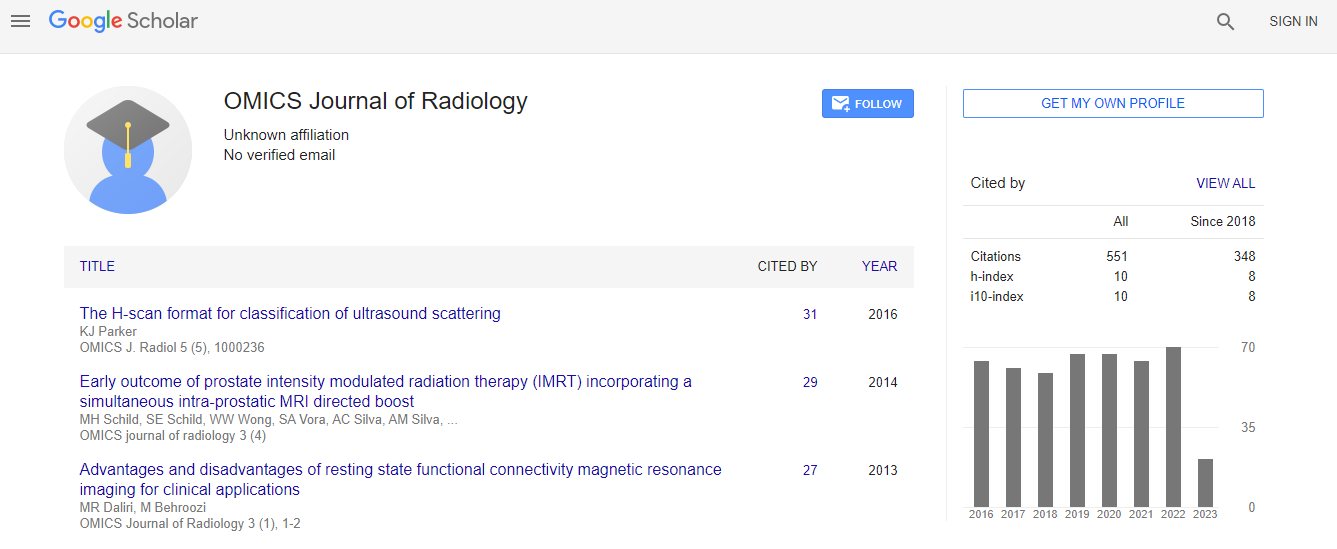
Google Scholar citation report
Citations : 551
Journal of Radiology received 551 citations as per Google Scholar report
Journal of Radiology peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Share This Page
Breast intervention from basic to advanced
2nd World Congress on Radiology and Oncology
Naglaa Mohamed Abdel Razek
Cairo University, Egypt
ScientificTracks Abstracts: OMICS J Radiol
Abstract
A biopsy remains the standard technique for diagnosing both palpable and non palpable breast abnormalities and is the preferred initial method of evaluating almost all breast masses (Burstein, 2011). Studies have shown that the combination of a physical examination, radiographic imaging and histopathological confirmation, also referred to as “the triple-test”, can produce accuracy levels of over 90% when all three components are concordant for benign or malignant disease (Singhal, 2008).Under certain circumstances when a mass or radiographic abnormality is categorized as probably benign in the presence of high patient anxiety, family history of breast cancer, or poor likelihood of compliance with recommended six-month follow-up imaging, a breast biopsy may be recommended for category three lesions (American Cancer Society, [ACS], 2011; National Comprehensive Cancer Network. A number of well-designed studies have demonstrated the safety and clinical utility of minimally invasive breast biopsy methods relative to open surgical biopsy. Advantages include less discomfort for the patient, a reduction in scarring and cosmetic defect, less invasive procedure, and quicker patient recovery. Percutaneous methods: Small needles: • Fine-Needle Aspiration Biopsy (FNAB) • Core Needle Biopsy (CNB): Automated spring-loaded core needle. Large needles: • Vacuum Assisted core needles. • Breast lesion excision system (Intact™) • Virtual needle: HIFU, high intensity focused ultrasound The following ultrasound guided procedures: 1. FNB of solid lesions 2. Core biopsy of solid lesions 3. Open surgical biopsy after Wire localization of non palpable lesions. 4. Vacuum assisted biopsy & closed excision of benign breast masses. 5. Percutaneous Cyst aspiration or abscess & seroma drainage. 6. Metallic clip placement to follow the effect of chemotherapy. Large needle procedures: BLES & VAB are two advanced automated large needle breast biopsy methods .To date , there is no clear international guide lines regarding the indications however we will try to put preferential indications of each technique based on the available international publications , NICE guideline (UK) as well as our experience in the two techniques ( 2000 VAB in 9 years and 300 BLES in 2yrs). What is VAB ? It is done using a percutaneous device developed specifically for breast biopsy. It is a sort of advanced large core needle biopsy. It utilizes vacuum assistance coupled with a high speed rotating cutter to acquire tissue samples. What is BLES? The BLES consists of a biopsy “wand” and 5 metallic prongs (wand size depending) with their tips connected by an Extensible cutting radiofrequency ring wire then pass from the wand and envelop an area of tissue ranging from 10 to 20 mm in diameter (depending on wand size) in only 8 s. The Prongs pass RF waves into surrounding tissue in order to excise and allow haemostasis, but not to the extent of damaging the sample. Allows excision of the entire breast mass or suspicious area as an intact complete mass may be with safety margin. Indications of Large needle procedures : Therapeutic = Resection of Image evidence of Benign Lesions (if surgery is not preferred) Fibroadenoms or Lipomas, Complex Cysts , Intraductal Vegetations, Papilloma, Hematomas , Scars Advantages: No hospitalization, Local anesthesia, Better targeting ,Small Incision ,No sutures ,No scar, Short duration of procedure, Can resume normal activity in 30 minutes & Poor side effects. Diagnostic 1. Suspicious lesions (BIRADS IV) with a size of less than 5mm 2. Mismatching radiography& pathology = Suspicious lesion & negative FNB or CNB 3. Mastopathic areas : for exclusion of suspected high risk lesions : ADH, radial scar, DCIS, lobular breast cancer 4. Unclassified/ suspicious microcalcification . 5. Focal architecture distortion . 6. Containdications to anasthesia and operations Conclusion: BLES & VAB are used as the primary method for histopathology diagnosis of suspicious small & borderline lesions as well as the unclassified microcalcfications. There are some limitations to BLES including; lactating females, patients with breast implants and patients presenting with a lesion close to the skin or in the axillary tail. BLES is favored in high risk lesions & DCIS considering the relative high underestimation rate associated with VAB and not found with the BLES . Moreover BLES offers complete lesion removal with available margin evaluation.Biography
Naglaa Abdel Razek is a graduate of Cairo University faculty of medicine the year 1993 and completed her studies for the MD in Radiology from the Cairo University in the year 2003. And she completed her training in breast imaging and intervention in Germany, Italy and France. Since 1995, she is working as a staff member in the radiology department and she was nominated as a professor of radiology since May 2013. She is one of the most recognized radiologists in Egypt working in the field of breast cancer screening, diagnosis and intervention. She introduced to Egypt the technique of non-invasive removal of benign tumors of the breast using the vacuum assisted biopsy and also she introduced a very new technique to Egypt , the breast lesion excision biopsy (BLES) and she is working with international group to set guidelines for the use of such a new technique. Dr Naglaa is an active member in the Women’s Health Outreach Program at the Ministry of Health since 2007 and in October 2014 till May 2016 ,she was nominated as the General manager of Egypt breast cancer screening program and women health in Egypt and she occupied the post of being the Minister Advisor in radiology for one year from January 2015 to January 2016. She is an active member and Board member of many National & International societies, She is president and founder of the Pink foundation and Detect Breast course & she is an international Board member of the American Association of Women Radiologists, European society of Radiology ,European Society of Breast Imaging & the Radiology Society of North America. Prof. Naglaa also is the principle breast radiologist and interventionist in Alfa scan Radiology Center and she is the head of the breast unit since 2003 till present . Naglaa has many national and international publications and has presented many presentations in national and international conferences especially concerned with breast cancer. Dr. Naglaa’s favorite mission is to fight breast cancer.
E-mail: naglaaabdelrazek@yahoo.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi