Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
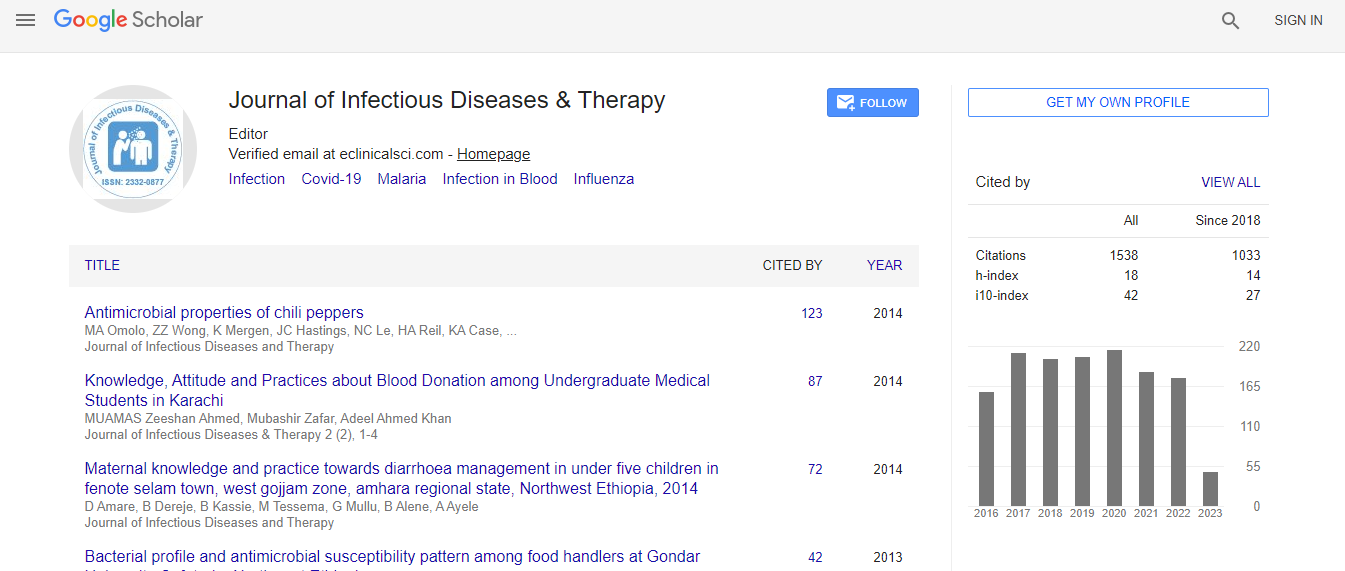
Google Scholar citation report
Citations : 1529
Journal of Infectious Diseases & Therapy received 1529 citations as per Google Scholar report
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Biochemical and microbiological profile of patients admitted with sepsis in an intensive care unit
4th International Congress on Infectious Diseases
Linda Bridina and Angelika Krumina
Riga Stradins University, Latvia
Posters & Accepted Abstracts: J Infect Dis Ther
Abstract
Background: Beyond issues related to measurement, the incidence of sepsis depends on host, pathogen and system factors, for example, lifestyle, sex, race, immune response, chronic health disorders, distribution of pathogens, and access to intensive care. Although these factors are articulated as separate entities, their complex interplay is crucial to consider. Materials & Methods: The retrospective analysis of 72 patients├ó┬?┬? medical records was carried out. The research included both sexes and all ages├ó┬?┬? patients who were hospitalized at Riga Eastern Clinical University Hospital inpatient "Gai├?┬╝ezers" from 2011 to 2014 years. Blood test on the sterility and identification of blood culture were performed for all the patients. Data was described using means with standard deviations (SD), median with interquartile range (IQR), Mann-Whitney U method, chi-square tests. Data statistical analysis was done in SPSS. Results: From all 72 (100%) patients included in the study, 67 (93.05%) patients had immuno compromised background- tumors, intra-abdominal infections, complicated soft tissue infections, cardiovascular, endocrine, lung, liver, kidney diseases, HIV, viral hepatitis and alcohol addiction. Five (6.9%) patients were not diagnosed with related diseases. Our data showed that most of the patients were in the age group of 60 to 79 (n=32.44%) and 20 of them (62.5%) died. Summarizing the results, all patients at the time of hospitalization had elevated C reactive protein (CRP). More than the half of patients 56 (77.7%) CRP was above 259 mg/L. Leukocytosis was diagnosed with 59 (81.9%) patients. Leukopenia was diagnosed with six (8.3%) patients. 32 (44.4%) patients had elevated liver indicators (ALT, AST). 39 (54.1%) patients had elevated kidney indicators. But the renal replacement therapy during hospitalization was received by 13 (18.1%) of patients. For the dead patients (n=36.50%) the renal replacement therapy was received by 25% (p = 0.12). Plating of blood was positive in 32 (44.4%) of all the patients. Blood agent in culture grows-Streptococcus betahemolytic group B was 1 (3.1%), Escherichia coli 3 (9.37%), Staphylococcus epidermidis 5 (15.6%), Staphylococcus hominis 1 (3.1%), Staphylococcus aureus 7 (21.9%), Staphylococcus haemolyticus 1 (3.1%), Prevotella oralis 1 (3.1%), Streptococcus pneumonia 10 (31.3%), Klebsiella pneumonia 1 (3.1%), Clostridium difficile 1 (3.1%), Streptococcus beta-hemolytic group A 1 (3.1%). Microbiological plating of urine was positive in 11 (15.3%) patients; the most common agents in plating were E. coli and Staphylococci. Conclusion: In our study, blood culture was mostly positive for less than a half of patients (44.4%). In most instances, bloodstream infections are intermittent and the circulating microbial loads are low; it makes the diagnosis and treatment of sepsis even harder.Biography
Linda Br├?┬źdi├?┬?a is currently studying at Riga Stradins University, Latvia. Her study mainly focuses on “Infection and immune system, biochemical and microbiological research on patients with sepsis”.
Email: linda.bridina@gmail.com

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi