Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
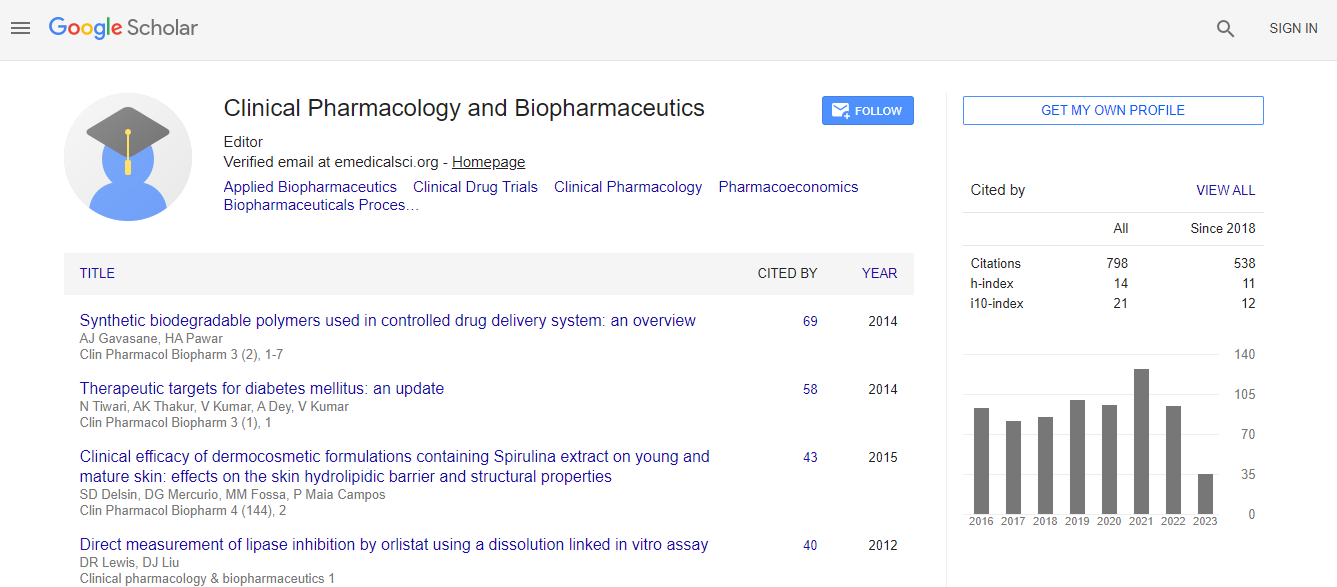
Google Scholar citation report
Citations : 1089
Clinical Pharmacology & Biopharmaceutics received 1089 citations as per Google Scholar report
Clinical Pharmacology & Biopharmaceutics peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Apoptotic-derived microparticles to endothelial-derived progenitor cells ratio as a novel biomarker in advanced heart failure patients
3rd International Conference on Clinical Pharmacy
Alexander E Berezin
Zaporozhye Medical University, Ukraine
ScientificTracks Abstracts: Clin Pharmacol Biopharm
Abstract
Background: Acutely Decompensated Chronic Heart Failure (ADHF) is considered a life-threatening event. Despite contemporary treatment strategies of ADHF, frequent recurrent hospitalizations due to other cardiovascular reasons after discharge of patients from the hospital are occurred. The objective of the study was to examine prognostic value of circulating Endothelial-Derived Apoptotic Microparticles (EMPs) to endothelial origin Mononuclear Progenitor Cells (MPCs) ratio for post-discharged patients with clinical stabilization after ischemic ADHF. Methods: We have consecutively enrolled 136 patients (62 male) with CAD admitted with a primary diagnosis of ADHF. All the patients have given their written informed consent for participation in the study. At baseline, all enrolled patients were hemodynamically stable and they had NYHA III/IV classes of ischemic CHF. Observation period started at discharge from the hospital and was up to 3 years. Flow cytometry analysis for quantifying the number of EMPs and angiogenic MPCs was used. Results: Calculated EMPs to MPCs ratios in survived and died patient cohort were 8.4 (95% CI=7.6ΓΆΒ?Β?9.2) and 78.9 (95% CI=53.0ΓΆΒ?Β? 116.6), respectively (p=0.001). MPCs, EMPs, NYHA class, NT-proBNP and increased NT-proBNP >30% within 24-48 hours of admission period remained statistically significant for all-cause mortality, CHF-related death, and CHF-related rehospitalisation, whereas LVEF and hs-CRP for all variables did not. We found that the addition of EPMs to MPCs ratio to the ABC model (NT-pro- BNP, increased NT-pro-BNP>30%) improved the relative IDI by 19.6% for all-cause mortality, by 21.7% for CHF-related death, and by 19.5% for CHF-related rehospitalisation. Conclusion: We demonstrated that EMPs to MPCs ratio is considered more tremendous indicator of an imbalance between angiogenic and apoptotic responses with possible relation to cardiovascular outcomes in post-discharged patients with clinical stabilization after ischemic ADHF.Biography
Email: dr_berezin@mail.ru

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi