Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
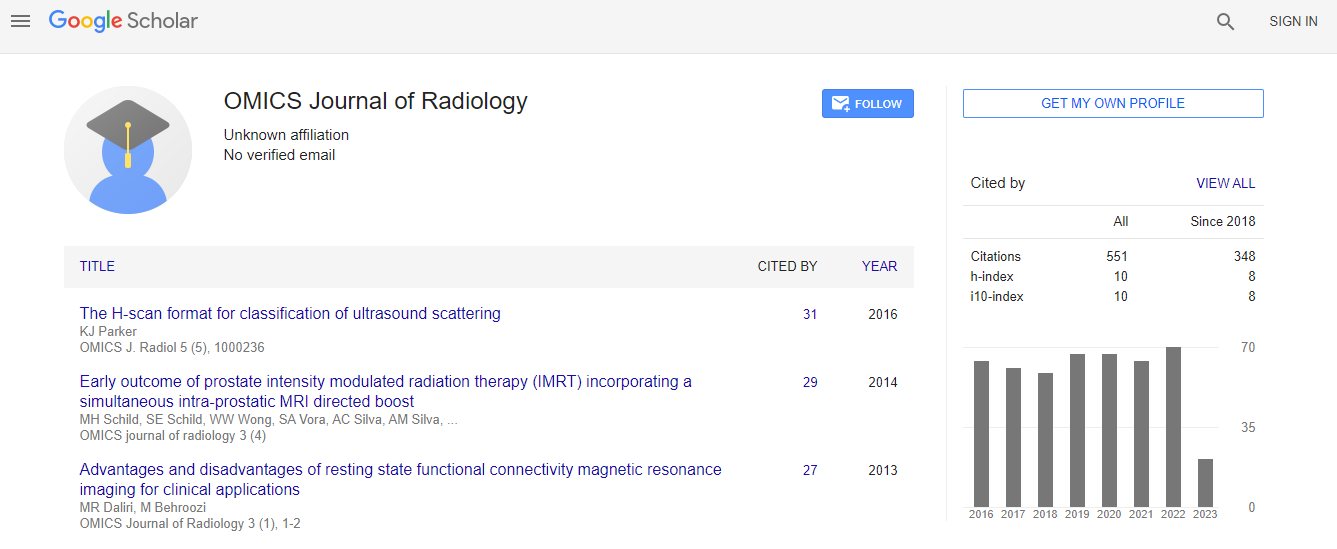
Google Scholar citation report
Citations : 551
Journal of Radiology received 551 citations as per Google Scholar report
Journal of Radiology peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Share This Page
Analytical fusion of different modality images based on prior knowledge
International Conference on Medical Imaging & Diagnosis
Michael L Goris, J Hongyun Zhu and Daniel Y Sze
Division of Nuclear Medicine Stanford University School of Medicine, California Division of Interventional Radiology
ScientificTracks Abstracts: OMICS J Radiol
Abstract
Background: Fusion is the simultaneous and combined analysis of two images mapping identically in the same object space, but recording a different attribute of the object. Most fusion has been performed as visual representation in which the attributes are represented independently into overlapping but independent color scales. In this work we explore fusion, in which the attributes are combined in a mathematical or logical manner, to address a specific goal. Methods: The first approach is mathematical, and concerns a particular combination of brain imaging: In patients treated for brain tumors, the usually clear delineation of pathology by MRI is compromised because the treatment itself may produce an ambiguous signal. Specifically, a FLAIR sequence will show post-treatment edema and recurrent tumor as a high signal intensity region. FDG PET on the other hand will show little or no density in the former, and (near normal) in the latter. A viable tumor would also show increased density in PET and post contrast T1 sequence, but not all post T1 high densities represent regions with high metabolic activity. The combination of these a-priori judgments (or prior knowledge) can be done in different manners: After normalization, the product MxP would favor viable tumor and the artangent of (P/M) would likely represent non-viable or non-malignant lesions. In the second approach, in preparation for a treatment of liver metastases with radioactive 90Y-labeled microspheres, the liver is infused intra-arterially with 99mTc macro aggregates, imaged, and reinjected with 99mTc colloid and imaged. The result is two in-line registered image volumes, defining MAA perfused tumor and liver, and functional liver (colloid) (Figure 2). The analysis of the fusion allows the computation of relative and absolute volumes, and relative doses to liver and tumor. We found that the relative dose to normal liver perfused by MAA is the best predictor of post therapy toxicity (as measured by the liver enzyme elevation). In cases of toxicity, the average relative volume was 66%, in the absence of toxicity, the relative volume was 33% (p<0.01), with only one case overlapping.Biography
Michael Goris has a Medical degree from the University of Leuven in Belgium and a PhD degree in Medical Physics from UC Berkeley. He has been a Professor in the Stanford Medical School and is Emeritus since 2012 and served as a Chairman for University panel on Radiation safety during 2003-2010. He has more than 120 publications in peer reviewed, journals. His research interests are Radio-immunotherapy, Medical Imaging Processing and Quantification for diagnosis Clinical validations.
Email: mlgoris@stanford.edu

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi