Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
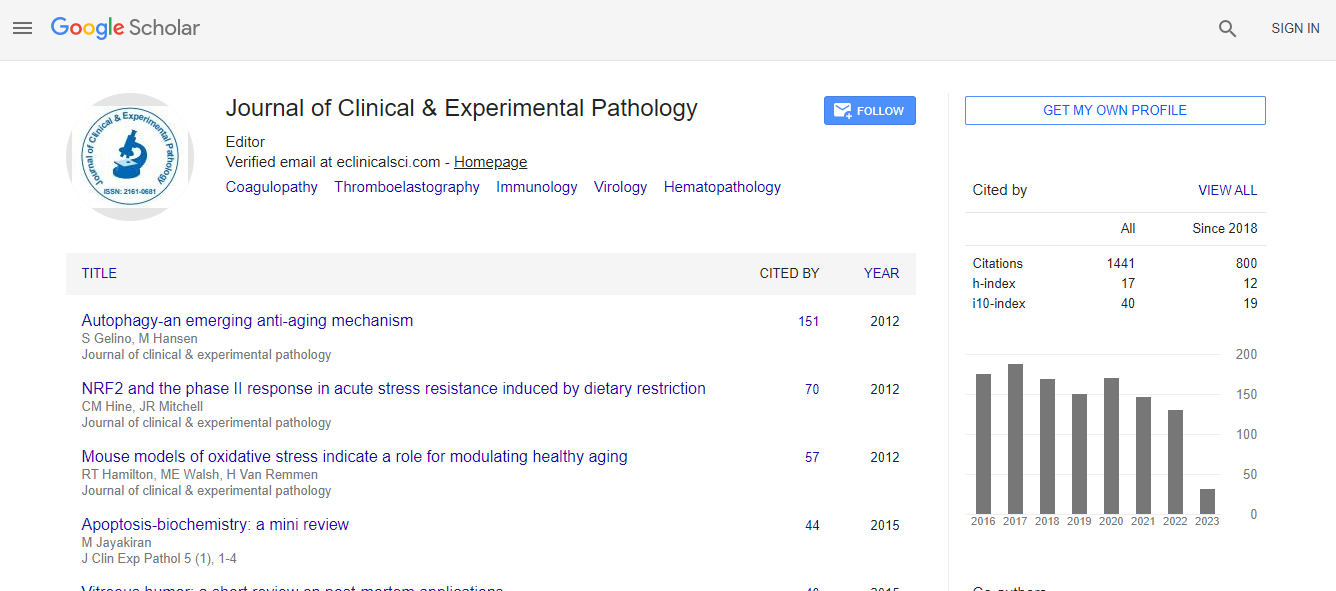
Google Scholar citation report
Citations : 2975
Journal of Clinical & Experimental Pathology received 2975 citations as per Google Scholar report
Journal of Clinical & Experimental Pathology peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Cosmos IF
- Ulrich's Periodicals Directory
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
- world cat
- journal seek genamics
- j-gate
- esji (eurasian scientific journal index)
Useful Links
Recommended Journals
Related Subjects
Share This Page
An analysis of ALK polysomy detected by fluorescence in situ hybridization analysis in non-small cell lung cancer patients at montefiore medical center
9th World Digital Pathology & Pathologists Congress
K H Ramesh, PhD, ABMGG, FACMGG
Montefiore Medical Center and Albert Einstein College of Medicine; Bronx, New York, USA
ScientificTracks Abstracts: J Clin Exp Pathol
Abstract
Non-small cell lung cancer (NSCLC) accounts for up to 80% of all lung cancers with an overall 5 year survival rate of about 10 to 15%. It is the leading cause of cancer-related mortality worldwide; and is responsible for 27% and 19.4% cancer deaths in the US and worldwide respectively. EGFR, KRAS, BRAF and ALK-EML4 anomalies are some of the driver mutations that have treatment and prognostic implications in NSCLC. The ALK-EML4 rearrangement has been identified in about 3 to 5% of NSCLC, with the large majority in adenocarcinoma and young patients who were light or nonsmokers. Recent studies have shown that lung cancers harboring the ALK-EML4 rearrangement are resistant to epidermal growth factor receptor tyrosine kinase inhibitors, but may be highly sensitive to ALK inhibitors, such as Crizotinib (Xalkori). Fluorescence In Situ Hybridization (FISH) analysis using the ALK DNA probe to determine if the tumor cells have the EML4-ALK rearrangement plays a vital role in establishing a rapid cytogenetic diagnosis. It is also helpful in monitoring the progression of the disease after treatment. However, a majority (>90%) of the patients with NSCLC show polysomy (multiple copies) of the ALK gene without the rearrangement. Little is known about the behavior of tumors showing polysomy, and the disease progression in patients with such tumors. At Montefiore we have been offering FISH testing (FDA approved) for ALK rearrangement since 2011. The aim of our study was to assess the survival difference in NSCLC patients without a history of tobacco use with ALK polysomy or the fusion oncogene. Using the Clinical Looking Glass database at Montefiore Medical Center in New York, we retrospectively identified four cases of ALK-EML4 gene rearrangement and 108 cases of ALK polysomy by FISH analysis from 2011-2014. Amongst the two groups, there were no significant differences in age (p=0.47) and there was a higher percentage of female patients in the rearrangement group than in the polysomy group (3/4 Vs.54/54). Using log-rank statistical analysis, there were no significant differences in survival from the date of NSCLC diagnosis between the polysomy and rearrangement groups (p=0.37). In conclusion, the lack of statistical significance in survival between the two groups may suggest that the oncogenicity of polysomy of ALK and the ALK-EML4 gene rearrangement in NSCLC patients works by similar mechanisms. However, the small sample size and single center study preclude any definitive conclusions in the survival differences. With clear knowledge of mortality in the two groups with a larger cohort of patients, molecular targets can be identified or the formulation of drugs that can prolong survival. As of 2016 we have added another 65 cases to the cohort of 112 cases, and are analyzing the extended data to determine if our conclusion will differ or remain the same.Biography
K H Ramesh a native of Bangalore, and an alumnus of Bangalore University & Kidwai Memorial Institute of Oncology, obtained his Doctoral Degree in Human Cancer Cytogenetics under the guidance of Professors M Krishna Bhargava, MD and B. N. Chowdaiah, Ph.D. He moved to the US in 1986 and completed his Clinical Cytogenetics training under the guidance of world renowned geneticist Avery Sandberg, MD at Roswell Park Cancer Institute, Buffalo, NY. At present he is the Director of Cancer CytoGenomics and Associate Professor of Pathology at Montefiore Medical Center & Albert Einstein College of Medicine, Bronx, NY. He is also Adjunct Associate Professor at The University of Texas MD Anderson Cancer Center. He is a Board Certified Clinical Cytogeneticist and a Diplomate of the American Board of Medical Genetics & Genomics, and Fellow of the American College of Medical Genetics & Genomics. His expertise is in genetic testing of leukemia, lymphoma, myeloma and soft and solid tumors. His interests include global education, football, and music.
Email: kramesh@montefiore.org

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi