Page 42
conferenceseries
.com
Volume 7, Issue 5 (Suppl)
J Psychol Psychother, an open access journal
ISSN: 2161-0487
Psychosomatic Medicine & Forensic Congress 2017
October 12-14, 2017
JOINT EVENT
24
th
International Conference on
PSYCHIATRY & PSYCHOSOMATIC MEDICINE
2
nd
International Congress on
FORENSIC SCIENCE AND PSYCHOLOGY
&
October 12-14, 2017 London, UK
Emotionally unstable personality disorder and psychosomatic problems
Matthew Rinaldi
King’s College London, London, UK
Bethlem Royal Hospital, UK
Statement of the Problem:
There are a specific sub-group of patients with emotionally unstable personality disorder (EUPD) who
tend to somatize overwhelming feelings rather than act them out via risky behaviors. They present to primary care services, receive
polypharmacy and are more likely to commit suicide. There are neuropsychiatric, psychodynamic and developmental explanations
for their tendency to somatize, but very little epidemiological data. We performed an audit of a tier-3 personality disorder unit to
determine the prevalence of psychosomatic disorders in this population and to determine any relationship between these diagnoses,
prescribing practices and attendance at therapy.
Methodology & Theoretical Orientation:
We conducted an audit of 63 waiting-list patients and performed a key-term search to
determine frequency of psychosomatic symptoms. We also performed a sub-group analysis of those patients in mentalization-based
therapy (i.e., with confirmed EUPD) and recorded the medications they were prescribed and their attendance at therapy.
Findings:
Psychosomatic conditions affected 57% of the waiting list population and 77% of the sub-group analysis. The most common
complaints were unexplained musculo-skeletal pain, unexplained chest pain and irritable bowel syndrome. Those with co-morbid
psychosomatic conditions were prescribed more medications, missed more therapy and cited medical reasons more often for missed
appointments.
Conclusion & Significance:
Psychosomatic disorders are more common in patients with EUPD than those without the diagnosis.
Psychosomatic disorders impact on attendance at therapy and increase the risk of polypharmacy. As such, psychosomatic conditions
should be routinely screened for at assessment and be positively diagnosed so that they can be addressed as a barrier to engaging in
treatment and understood within therapy as a coping mechanism. Psychosomatic disorders should be among the list of differentials
as the multi-disciplinary team investigate, interpret and manage physical symptoms sensibly.
Biography
Matthew Rinaldi is a core Trainee Psychiatrist on the Maudsley training programme. He has interests in psychosomatic conditions, the psychotherapeutic
understanding and multi-disciplinary management of them. A trainee who works for bottom-up service improvement, his work stems from under-researched
problems that he encounters in clinical practice.
matthew.rinaldi@slam.nhs.ukMatthew Rinaldi, J Psychol Psychother 2017, 7:5(Suppl)
DOI: 10.4172/2161-0487-C1-017
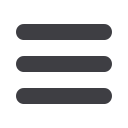
Graph 1:
Medications prescribed per-person in the sub-group analysis of
those with (blue) and without (red) psychosomatic disorders
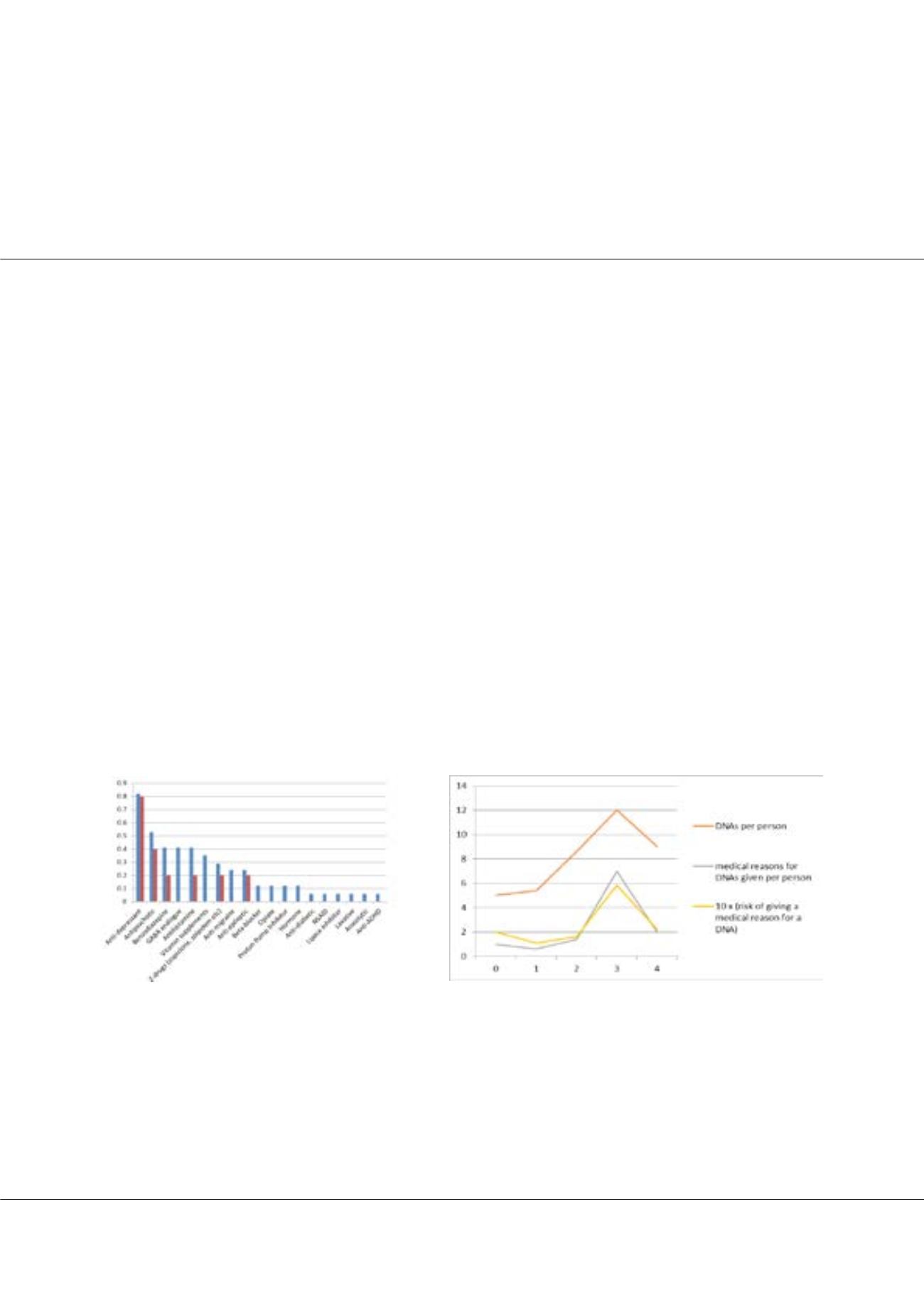
Graph 2:
Relationship between the number of psychosomatic disorders (x-axis);
DNA rates and the risk of giving a medical reason for a DNA (y-axis)
















