Page 34
conferenceseries
.com
Volume 7, Issue 3 (Suppl)
J Obes Weight Loss Ther, an open access journal
ISSN: 2165-7904
Childhood Obesity & Bariatric Surgery 2017
June 12-13, 2017
June 12-13, 2017 Rome, Italy
&
Childhood Obesity and Nutrition
10
th
International Conference on
Metabolic and Bariatric Surgery
2
nd
International Conference on
JOINT EVENT
Eating and neurodevelopmental disorders in a clinical sample of children and adolescents with obesity
Elisabet Wentz, Anna Björk
and
Jovanna Dahlgren
University of Gothenburg, Sweden
Statement of the Problem:
Eating disorders are overrepresented in adults with obesity, but little is known about children with obesity.
Attention-deficit/hyperactivity disorder (ADHD) is more prevalent in children with obesity. Impulsive and disorganized behavior,
typically for ADHD, may contribute to an eating pattern that initiates weight gain and complicates the conventional treatment of
obesity. No studies on individuals with obesity have investigated the occurrence of autism spectrum disorder (ASD). Little is known
about the overlap between eating and neurodevelopmental disorders in children with obesity.
Aim:
The purpose of this study is to investigate the prevalence of eating disorders, ADHD, ASD and other neurodevelopmental
disorders in children and adolescents with obesity, and to explore a possible overlap between eating and neurodevelopmental
disorders.
Method:
76 children (37 girls, 39 boys) were recruited at referral to a university outpatient clinic. The parents were interviewed
regarding the child’s psychiatric morbidity and completed parental questionnaires pertaining to ADHD, ASD and other
neurodevelopmental disorders. The parents were screened for adult ADHD. The pro-bands completed instruments pertaining to
eating disorders. Anthropometric and metabolic data were collected.
Result:
Bodymass index ranged between SDS 1.92 and 5.90, and age between 5.1 and 16.5 years. ASDor ADHDwas diagnosed in 13.2%
and 18.4% of the children, respectively. 25% were screen-positive for motor problems, 31.6% had at least one neurodevelopmental
disorder. 18.4% had a parent who screened positive for adult ADHD. DSM-5 eating disorders were rare but so-called “loss-of-control
eating (LOC)” was present in 22% of the adolescents. One in three with LOC had also a neurodevelopmental disorder.
Conclusions & Significance:
ASD and ADHD are overrepresented in clinical populations of children and adolescents with obesity.
ADHD and LOC both reflect how impulsive traits can manifest in obese children.
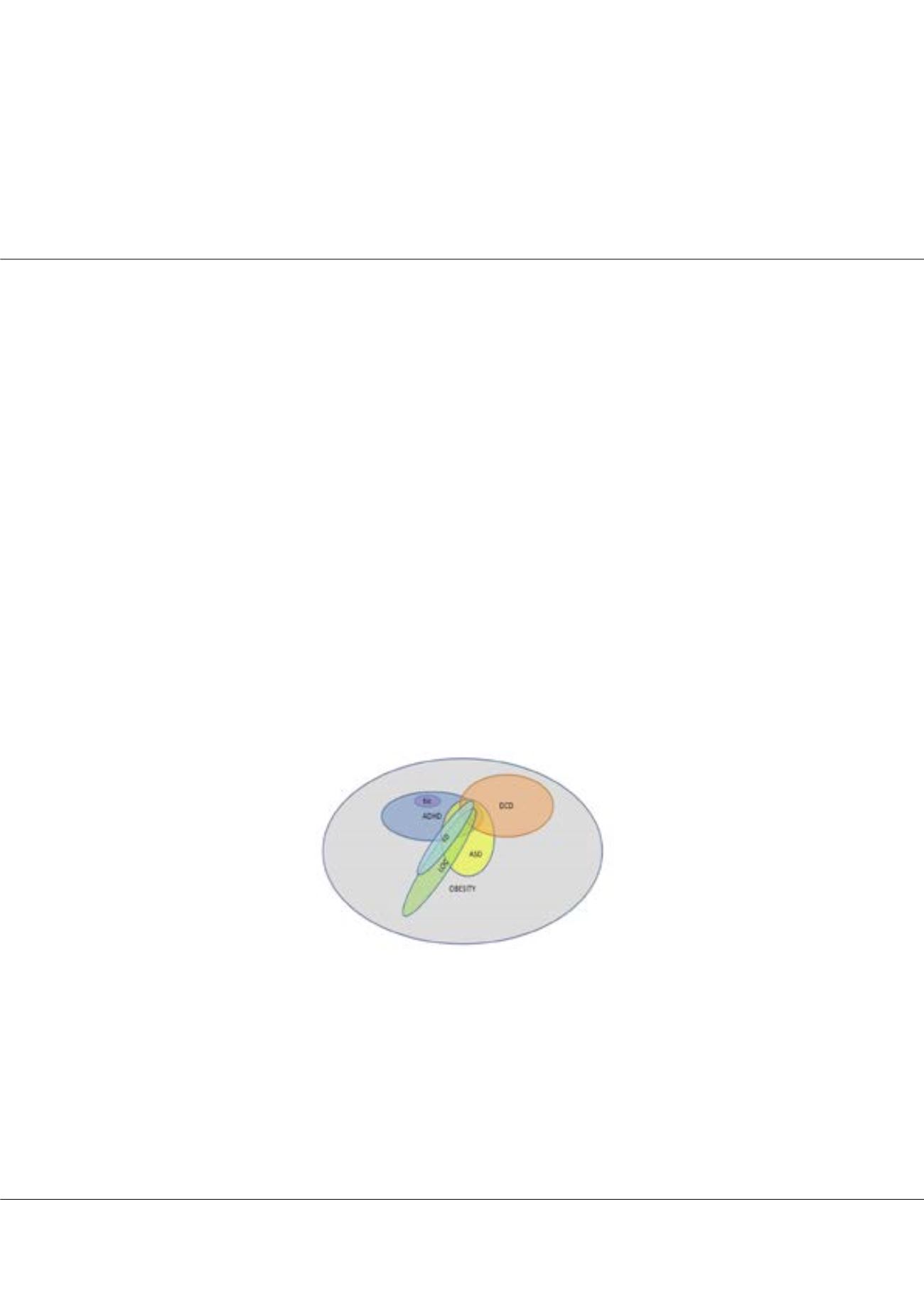
Figure:
Overlap between obesity, eating and neurodevelopmental disorders; ED: eating disorder; LOC: loss-of-control eating;
ASD: autism spectrum disorder; ADHD: attention-deficit/hyperactivity disorder; DCD: developmental coordination disorder;
tic: tic disorder.
Biography
Elisabet Wentz is the Manager of Gillberg Neuropsychiatry Centre, Associate Professor of Child and Adolescent Psychiatry, Senior Consultant at Child
Neuropsychiatry Clinic, Queen Silvia Children’s University Hospital and licensed as a Specialist in Child and Adolescent Psychiatry. Her PhD thesis entitled “Ten-
year outcome of anorexia nervosa with teenage onset”. Her current research includes, but is not limited to, “Longitudinal follow-up studies of anorexia nervosa,
the correlation between obesity, neuropsychiatry and eating disorders, eating disorders within the autism spectrum, non-pharmacological interventions (including
IT interventions) in cases of neuropsychiatric disabilities, as well as neuropsychiatric comorbidity in cases of various syndromes”. She has Post-doctorate position
at St. George’s Hospital Medical School, London. She has published around 50 peer-reviewed scientific papers as well as several book chapters. She supervises
PhD students at University of Gothenburg and at Lund University.
elisabet.wentz@gnc.gu.seElisabet Wentz et al., J Obes Weight Loss Ther 2017, 7:3 (Suppl)
DOI: 10.4172/2165-7904-C1-045