Research Article Open Access
Virulence Factors Involved in Passage of Francisella tularensis subsp. novicida Through an Air-Blood Barrier Model
Sandra S. Ojeda1, Chris A. Mares2, Jorge I. Alvarez3, Qun Li4, Carlos J. Orihuela2 and Judy M. Teale2,4*
1Department of Immunology UT MD Anderson Cancer Center 7455 Fannin Houston, TX, 77030, USA
2Department of Microbiology and Immunology, University of Texas Health Science Center at San Antonio 7703 Floyd Curl Dr. San Antonio, TX, 78229, USA
3Neuroimmunology unit, Neurosciences Centre Hospitalier De L’Université de Montréal - Hôpital Notre Dame 2099 Alexandre de Seve, Y3608 Montreal, QC H2L 2W5
4Department of Biology, University of Texas at San Antonio One UTSA Circle San Antonio, TX, 78249, USA
- *Corresponding Author:
- Judy M. Teale Ph.D
Department of Biology-MBT
University of Texas at San Antonio
One UTSA Circle, San Antonio, TX 78249
Tel: 210-458-7024
Fax: 210-458-7025
E-mail: judy.teale@utsa.edu
Received Date: June 24, 2011; Accepted Date: November 08, 2011; Published Date: November 17, 2011
Citation: Ojeda SS, Mares CA, Alvarez JI, Li Q, Orihuela CJ, et al. (2011) Virulence Factors Involved in Passage of Francisella tularensis subsp. novicida Through an Air-Blood Barrier Model. J Bioterr Biodef S3:003. doi: 10.4172/2157-2526.S3-003
Copyright: © 2011 Ojeda SS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Francisella tularensis subsp. novicida ( F. novicida ) is a facultative intracellular pathogen that when inhaled causes respiratory infection in mice; it is widely used as a model to study tularemia caused by F. tularensis. F. novicida is able to infect different cell types including macrophages and dendritic cells. In the present study we examined F. novicida interactions with human lung epithelial cells and determined the role of established virulence determinants in these processes. A549 type II lung epithelial cells and murine LA-4 bronchial epithelial cells were used to examine the ability of wild type F. novicida and the mutant F. novicida strains deficient in IglC, Tul4, MglA, 58kDa membrane lipoprotein, and RipA to adhere, invade, replicate within, and translocate through an in vitro transwell system. Using this systematic approach, we determined that different virulence factors play cell-site specific roles during infection: Tul4 is important for adhesion to lung cells; MglA, 58kDa protein, and Tul4 are important for cell invasion; IglC and its transcriptional regulator MglA are important for intracellular replication; and the function of MglA is required for migration across cell barriers. In addition we also determined that F. novicida infection results in upregulation of matrix metalloprotease 9 (MMP-9) by lung epithelial cells and the subsequent disruption of cell adherens junctions as characterized by loss of cadherin, alpha and beta catenin, and the basal membrane protein laminin.
We conclude that F. novicida is able to attach, invade, and cross through lung epithelial cells and that these properties are determined by individual virulence determinants.
Keywords
Francisella; Air-blood barrier; Lung; Epithelium; Adhesion; Invasion.
Introduction
Francisella tularensis is a facultative intracellular pathogen that is the causative agent of tularemia. Francisella has a broad host range as it is able to infect amoeba, arthropods, rodents and higher mammalian species [1-4]. In humans the primary replication site appears to be the macrophage although other cell types have been implicated [5-7]. Infection is established through contact with infected tissues, arthropod bites, inhalation and ingestion, leading to various clinical manifestations [2,8]. The route of infection is a key factor in determining disease severity with inhalation being the most dangerous route [2,9,10]. Two subspecies of F.tularensis are capable of causing disease in humans [9,10]. F.tularensis (type A) is the most virulent subspecies and is primarily found in North America. It is capable of causing respiratory disease with as few as 10 organisms. The highly virulent nature of type A bacteria combined with its ability to be aerosolized has led the Centers for Disease Control and prevention (CDC) to designate it as a category A biological warfare agent [2,11]. F.tularensis subsp. holarctica (type B) is less virulent but more widespread. It is found across the Northern hemisphere, as well as Europe, and Asia. The attenuated F.tularensis live vaccine strain (LVS) was derived from a Type B strain [12]. F.tularensis subsp. novicida (F. novicida) is an important laboratory strain, as it remains highly virulent in mice causing respiratory disease with severe lung pathology and death within 3-5 days after infection; it is principally used to model Type A infections outside of a Biosafety level 3 (BSL-3) facility [13].
The airway epithelium constitutes the primary barrier that microorganisms encounter when they enter the body through the aerosol route. The close proximity of alveolar epithelial cells to the bloodstream make them a critical cell barrier that prevents microorganisms from entering the bloodstream and disseminating throughout the body. In addition to the barrier function, the airway epithelium produces pro-inflammatory molecules, immune regulators, as well as a variety of antimicrobial factors such as lysozyme, defensins and reactive nitrogen species [14,15]. Therefore, the interaction of pathogenic microorganisms with the airway epithelial cells and the resulting response determines whether bacteria disseminate and cause disease in the host.
Recent studies have reported the ability of F.tularensis LVS to invade and replicate within alveolar type II epithelial cells [5,16,17]. In this study we show that F. novicida is also able to adhere, invade and replicate within lung epithelial cells enabling it to cross the air-blood barrier. Importantly, we observed that several known virulence factors play distinct roles in F. novicida adhesion, invasion, replication and migration through the air-blood barrier. Together, these observations provide new insights into the pathogenic mechanisms of Francisella.
Materials and Methods
Bacterial strains and cell lines
Wild type F. novicida (U112) strain was obtained from Dr. Bernard Arulanandam (University of Texas at San Antonio, San Antonio TX) through Dr. Fran Nano (University of Victoria, Victoria, British Columbia, Canada) [18,19]. F. novicida mutant strains ΔiglC, ΔmglA, Δtul4 and ΔripA protein mutant strain (ΔripA, locus tag FTN_0157) were obtained from Dr. Karl Klose (University of Texas at San Antonio, San Antonio, TX) [20,21]. F. novicida 58kDa protein mutant strain (Δ58kDa, locus tag FTN_0444) was kindly provided by Dr. L. Gallagher (University of Washington, Seattle, WA) [20]. All F. novicida strains were grown at 37°C on trypticase soy agar plates supplemented with 0.1% cysteine (TSAcys). Mutant strains ΔiglC, ΔmglA, and Δtul4 were grown in the presence of 100 mg/mL of erythromycin. The Δ58kDa mutant was grown on trypticase soy agar plates supplemented with 0.1% cysteine (TSAcys). The mutant strain ΔripA was grown on TSAcys in the presence of 50 mg/mL of kanamycin. INV110 is a laboratory strain of Escherichia coli that is normally used for cloning [22]. INV110 was cultured on Luria Bertani (LB) broth and agar at 37° C; broth cultures were grown in an orbital shaker. A549 cells (ATCC CCL-185) are a type II pneumocyte cell line derived from a human lung adenocarcinoma [23]. LA-4 cells (ATCC CCL-196) are a bronchial epithelial cell line derived from a murine lung adenoma [24]. Both cell lines were low passage derivatives. Cell lines were cultured in F-12 media supplemented with 10% fetal bovine serum and an antibioticantimycotic (1 unit of penicillin, 100 mg of streptomycin and 0.25 mg/ml of amphotericin B) (Gibco, Carlsbad, CA) in a humidified atmosphere containing 5% CO2 at 37°C. Human umbilical vein endothelial cells (HUVECs) were acquired from Lifeline Technology, Part# FC-0003, lot # 00213, manufactured 09/19/07 and cultured in Endothelial Basal Media (EBM) supplemented with 2% fetal bovine serum, 0.4% bovine brain extract, 0.1% human epidermal growth factor, 0.1% hydrocortisone and 0.1% gentamicin sulphate amphotericin B.
Adhesion, Invasion and Replication Assays
Cells were grown in 24-well tissue culture treated polystyrene plates; all assays were performed using confluent monolayers of cells (106 cells per well). Prior to each experiment, bacteria were streaked onto fresh agar plates and grown overnight. The next day bacteria were scraped from the plates and used to create a bacterial suspension corresponding to approximately 1 x 106 colony forming units (CFU)/ ml in F-12 media. For adhesion assays, cell monolayers were washed to remove antimicrobials and 250 μl of the bacteria suspensions added to the wells at a Multiplicity of infection (MOI) of 1. Plates were centrifuged at 1000 cfg for 15 min and then transferred to a 37°C, 5% CO2 incubator for 1 hour. After the incubation, unattached bacteria were removed by washing the cells 3 times for 5 minutes with phosphate buffer saline (PBS; pH 7.4). Cells were lysed using 100 μl of 0.1% Triton X-100. The lysate was serially diluted, spread on agar plates, and the plates incubated overnight. Adhered bacteria were extrapolated from the number of colonies counted the next day on the plates. For invasion assays, following the 1 hr incubation, bacteria infected cells were washed and then incubated for 2 hrs with F-12 culture media containing 50 μg/mL of gentamicin. The invasion rate was calculated dividing the number of bacterial cells invading by the number of bacterial cells attaching. Subsequently, the numbers of intracellular bacteria were determined by washing with PBS, lysing the cells with Triton X-100, plating and bacterial colony counting the next day. To assess intracellular replication, after treatment with 50 μg/ mL gentamicin for 2 hours, cells were washed and incubated with F-12 media containing 2 μg/mL of gentamicin. After 2, 6 and 24 hrs, the cells were washed and lysed with Triton X-100. The number of intracellular bacteria was determined as previously described.
Immunofluorescence staining
A549 cells were grown on poly-L-lysine-coated coverslips. Cells were infected with F. novicida as indicated above. At the designated time points, single immunofluorescence staining was performed. Cells were washed 3 times with PBS. The cells were fixed using 70% ethanol for 5 min at room temperature (RT), washed twice again with PBS and then washed with TNT buffer (Tris 0.1M, NaCl 0.15M and Tween 20 0.05%). To block unspecific antibody binding the cells were incubated 30 min at RT with 10% serum from a naïve mouse, followed by a 40 min RT incubation with an antibody specific for F. novicida lipopolysaccharide (LPS) conjugated with Alexa 488 (1:300). After that, the cells were washed three times with TNT, one wash with 1% Triton X-100 and 3 more washes with TNT. The slides were mounted with Cytoseal (Calbiochem) containing nuclear staining 4’,6-diamidino-2- phenylindole (DAPI, 0.3 μM). Double immunofluorescence staining was performed as described above but using first a set of primary antibodies specific for pan-cadherin, α-catenin and β-catenin (R&D Systems, Minneapolis, MN), basal membrane protein laminin (Sigma- Aldrich, St. Louis, MO), and the pro and active form of matrix metalloproteinase 9 (MMP-9) (Sigma-Aldrich, St. Louis, MO) which were purified rabbit anti-mouse and as secondary antibody rhodamine red X (RRX)-conjugated AffiniPure anti rabbit IgG (Jackson Immuno Research Laboratories, Inc., West Grove, PA). This procedure was then followed by incubation with a specific antibody for F. novicida as described above.
Generation and infection of an in vitro air-blood barrier
The air-blood barrier was constructed on 0.4 μm pore snapwell membranes (CORNING, Corning, NY 14831 USA) first seeded on the bottom (membrane) upside down with 2.5 X 105 cells/ mL of HUVECs in EBM media supplemented as described above. HUVECs were allowed to grow for 48 hrs at 37°C and 5% CO2. Then, the snapwell membranes were inverted and the A549 cells were seeded on the top side of the membrane at a concentration of 2.5 X 105 cells/ mL in F-12 media supplemented with 10% FBS and antibiotic-antimycotic as described above. The media was changed in the top and lower chamber the next day. The confluence of the bilayer was monitored by changing the media present in both chambers for fresh media and by measuring the volume present in the top chamber 5 minutes after fresh media had been added; if 10% or less volume of fresh media was lost from the top chamber the bilayer was considered to be ready for infection. Once the air-blood barrier was ready for infection, cells were washed three times with F-12 media, and each well was infected with approximately 1 X 106 CFU/ml of bacteria in 250 μl of media. Immediately after infection, the content of the lower chamber in each well was collected, spun down, suspended in 120 μl of F-12, and then plated to determine the number of bacteria crossing the air-blood barrier (bilayer). Following this procedure, plates of bilayers were incubated at 37°C and 5% CO2. Collection of the lower chamber contents was performed at 2, 6 and 24 hrs after infection following the procedure described above. 2.5 ml of media contained in the lower chamber were refilled after the collection at each time point.
Statistical Analysis
Results were expressed as means and the error bars indicate the standard error of the mean. In all the figures, data were pooled from at least three independent experiments with each experiment having 3 or more replicates. Data obtained for U112 was compared to E. coli and F. novicida mutant strains ΔiglC, Δtul4, ΔmglA, Δ58kDa and ΔripA by using a homoscedastic two-tailed Student’s t-test. Statistical significance was established at P < 0.05. Invasion data were analyzed statistically comparing F. novicida against E. coli infected cells for each cell type separately. Replication data were analyzed statistically comparing F. novicida against each mutant strain for each time point, 2 hrs, 6 hrs and 24 hrs of replication. A one-way ANOVA and a Dunn’s mutiple comparison post-test were used to analyze the infection of the air-blood barrier.
Results
F. novicida adheres and invades lung epithelial cells in vitro
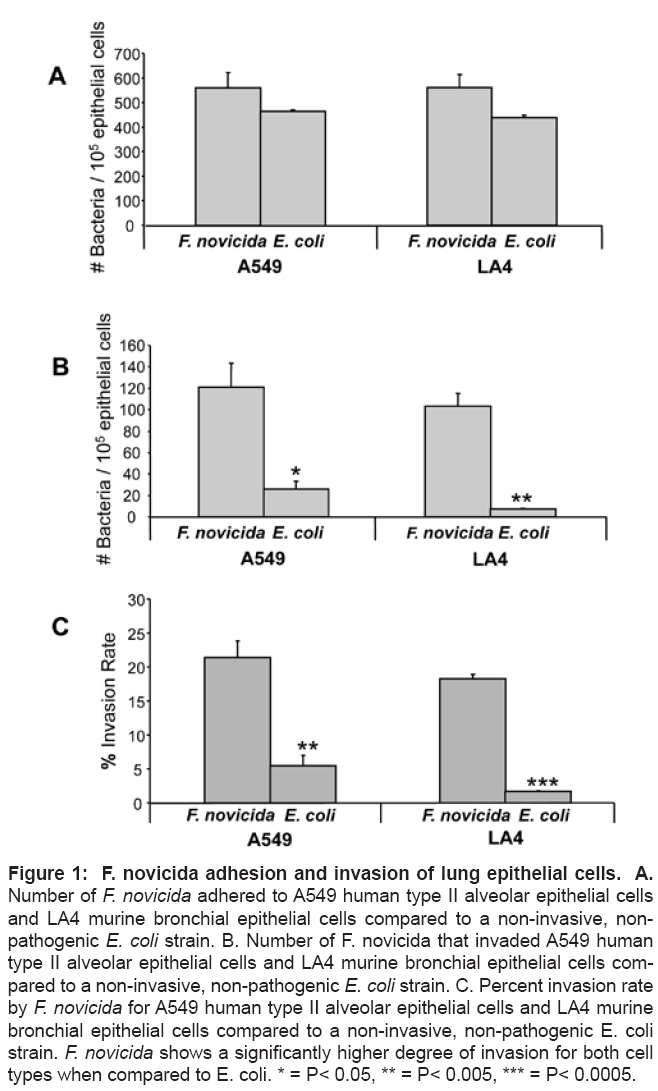
It has been previously reported that F.tularensis LVS invades and replicates within TC-1, MLE 12, A549, HEp-2 and HBE rodent and human lung epithelial cells [5,17,25]. In contrast it remains unknown if F. novicida is able to replicate within lung epithelial cells. To determine whether F. novicida could adhere and invade lung epithelial cells we performed adhesion and invasion assays in vitro using A549 lung cells and LA-4 bronchial epithelial cells. For comparison purposes we included a non-invasive, non-pathogenic E. coli strain, INV100. Wild type (WT) F. novicida (U112) adhered to both cell lines at levels equivalent to INV100 (Figure 1A). In contrast, U112 invaded A549 and LA-4 cells at levels 5-fold (p=0.016) and 14-fold (p=0.0013) greater than INV100, respectively (Figure 1B). Extrapolation of the invasion rate (invasion/adherence) indicated that approximately 20% of U112 that attached to a cell were able to invade; in contrast only 2-5% of INV100 were detected as intracellular (Figure 1C). Importantly, no cell line specific differences were observed between A549 or LA-4 cells for U112 adhesion or invasion, suggesting that bronchial and alveolar epithelial cells are equally susceptible to these processes. Overall, similar levels of adhesion by U112 and INV100 indicate a passive binding to lung cells. However, F. novicida seems to have the ability to invade these cells, whereas this property is absent in non-pathogenic E. coli.
Figure 1: novicida adhesion and invasion of lung epithelial cells. A. Number of F. novicida adhered to A549 human type II alveolar epithelial cells and LA4 murine bronchial epithelial cells compared to a non-invasive, nonpathogenic E. coli strain. B. Number of F. novicida that invaded A549 human type II alveolar epithelial cells and LA4 murine bronchial epithelial cells compared to a non-invasive, non-pathogenic E. coli strain. C. Percent invasion rate by F. novicida for A549 human type II alveolar epithelial cells and LA4 murine bronchial epithelial cells compared to a non-invasive, non-pathogenic E. coli strain. F. novicida shows a significantly higher degree of invasion for both cell types when compared to E. coli. * = P< 0.05, ** = P< 0.005, *** = P< 0.0005.
Differential adhesion and invasion of F. novicida and mutant strains to lung epithelial cells
We next sought to determine the role of established Francisella virulence genes in the adhesion and invasion process of epithelial cells. Five different mutant derivatives of U112 were used: 1) ΔiglC (ΔiglC: :ermC) which lacks the iglC gene that is present in the Francisella pathogenicity Island (FPI) and is necessary for intramacrophage survival and growth [21,26]; 2) ΔmglA (ΔmglA: :ermC) that lacks the mglA gene which is the transcriptional regulator of the FPI genes [21,26]; 3) Δtul4 (Δtul4: :ermC) that lacks a 17-kDa membrane lipoprotein that is known to be recognized by T cells from a majority of F.tularensis primed individuals and has been described as a ligand for the human TLR2/TLR1 heterodimer [21,27,28]; ΔiglC, ΔmglA and Δtul4 mutants were generated by utilizing universal priming of optimized antibiotic resistance cassettes and splicing by overlap extension (SOE) [21], mutations generated through this method have characteristics of non-polar mutations [29] 4) Δ58kDa that lacks a 58kDa membrane lipoprotein reported to contribute to virulence in vitro and in vivo [30,31]; this mutant has shown non-polar effects [30] finally, 5) ΔripA that lacks a cytoplasmic membrane protein required for intracellular replication of F.tularensis LVS within macrophages and lung epithelial cells [32]; this is a transposon mutant with disruption of the ripA gene [20].
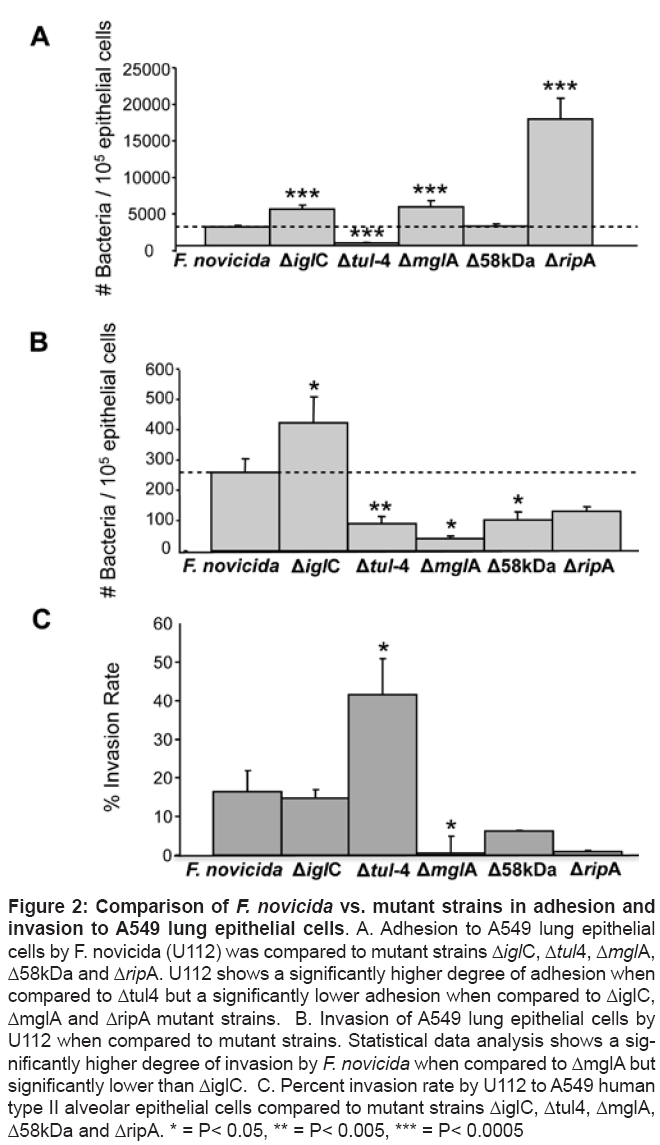
Following adherence and invasion assays we determined that mutant strain ΔiglC adhered and invaded lung cells at levels greater than U112 (Figures 2A and 2B), however analysis of the invasion rate suggested that cell surface attached ΔiglC mutants had an equal propensity to invade lung cells as U112 (U112 invasion rate = 16%; ΔiglC = 15%) suggesting that mutation of iglC only affected adhesion (Figure 2C). In contrast Δtul4 adhered and invaded lung cells at significantly lower levels than U112 (Figures 2A and 2B). Despite this, invasion rate analyses suggest that adhered Δtul4 mutants had a greater capacity to invade cells than U112 (invasion rate = 46%) (Figure 2C). The ΔmglA mutant adhered to A549 cells at a significantly higher level than U112 (p< 0.0005) (Figure 2A). However, a significant decrease in the number of intracellular ΔmglA was observed versus U112 (Figure 2B). Of note the invasion rate of ΔmglA was 10-fold lower than U112 (ΔmglA invasion rate < 1%) (Figure 2C). This finding suggests that ΔmglA mutant strain improperly regulates the expression of protein(s) involved in both adhesion and invasion. The mutant strain Δ58kDa showed similar levels of adhesion when compared to U112; however, it too had significantly diminished invasion levels (p<0.05) (Figure 2B) with an invasion rate of 6% (Figure 2C). Finally, strain ΔripA showed significantly higher levels of adhesion to lung cells than WT strain (Figure 2A). However, it appeared to have decreased levels of invasion of lung cells although the final value was not statistically significant p=0.1466 (Figure 2B) and its invasion rate was only 1% (Figure 2C). Collectively, these findings suggest that the F. novicida adherence and invasion are distinct pathogenic processes and that deletion of established virulence determinants may have unexpected outcomes on these complex processes.
Figure 2: Comparison of F. novicida vs. mutant strains in adhesion and invasion to A549 lung epithelial cells. A. Adhesion to A549 lung epithelial cells by F. novicida (U112) was compared to mutant strains ΔiglC, Δtul4, ΔmglA, Δ58kDa and ΔripA. U112 shows a significantly higher degree of adhesion when compared to Δtul4 but a significantly lower adhesion when compared to ΔiglC, ΔmglA and ΔripA mutant strains. B. Invasion of A549 lung epithelial cells by U112 when compared to mutant strains. Statistical data analysis shows a significantly higher degree of invasion by F. novicida when compared to ΔmglA but significantly lower than ΔiglC. C. Percent invasion rate by U112 to A549 human type II alveolar epithelial cells compared to mutant strains ΔiglC, Δtul4, ΔmglA, Δ58kDa and ΔripA. * = P< 0.05, ** = P< 0.005, *** = P< 0.0005
F. novicida and mutant strains replicate in lung epithelial cells
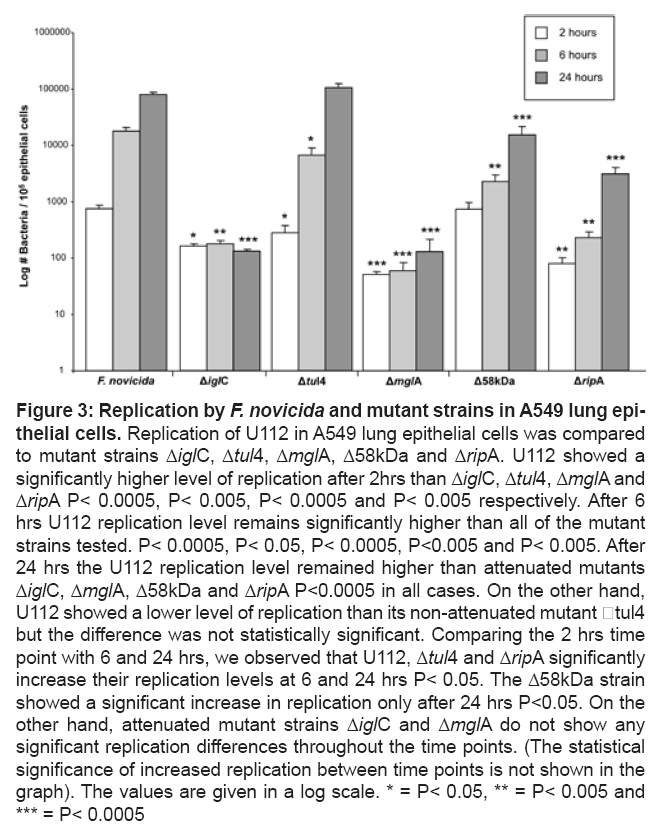
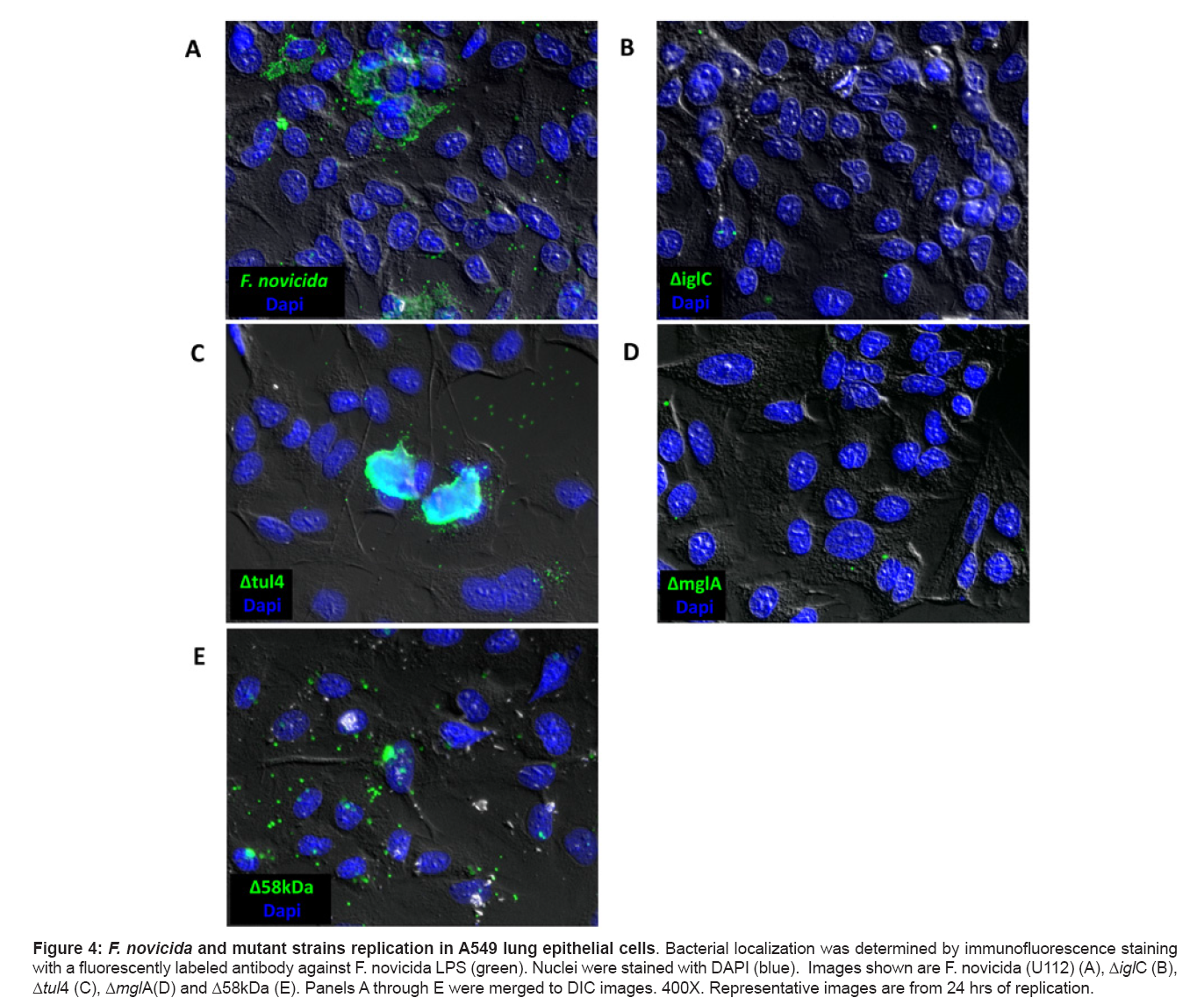
One major aspect of F.tularensis pathogenesis is its ability to replicate within cells [5,6,33,34]. To determine the replicative capacity of F. novicida, A549 lung epithelial cells were infected with U112 for 2, 6 and 24 hrs (Figure 3). We observed that U112 was able to replicate exponentially and in a time dependent fashion. Thus intracellular replication in lung epithelial cells may also be a virulence determinant for F. novicida. We subsequently examined the role of IglC, MglA, Tul4, 58kDa (Figure 3 and 4) and RipA (Figure 3) in intracellular replication. ΔiglC and ΔmglA failed to multiply, and the levels of these mutants remained constant through 24 hours. It is important to highlight that neither displayed a net loss of intracellular bacteria over time suggesting that they were not killed within the cell. Interestingly the inability of ΔiglC to replicate contrasted with its increased ability to adhere and invade cells, whereas the inability of ΔmglA to replicate was consistent with more global defects including those observed for invasion. These findings were confirmed by immunofluorescent microscopy where very few bacteria were observed in A549 cells after 24 hrs for ΔiglC and ΔmglA (Figures 4B and 4D respectively). Importantly no defects were found for intracellular replication for Δtul4, Δ58kDa or ΔripA mutants, thus indicating that these genes did not impact intracellular survival and/or replication.
Figure 3: Replication by F. novicida and mutant strains in A549 lung epithelial cells. Replication of U112 in A549 lung epithelial cells was compared to mutant strains ΔiglC, Δtul4, ΔmglA, Δ58kDa and ΔripA. U112 showed a significantly higher level of replication after 2hrs than ΔiglC, Δtul4, ΔmglA and ΔripA P< 0.0005, P< 0.005, P< 0.0005 and P< 0.005 respectively. After 6 hrs U112 replication level remains significantly higher than all of the mutant strains tested. P< 0.0005, P< 0.05, P< 0.0005, P<0.005 and P< 0.005. After 24 hrs the U112 replication level remained higher than attenuated mutants ΔiglC, ΔmglA, Δ58kDa and ΔripA P<0.0005 in all cases. On the other hand, U112 showed a lower level of replication than its non-attenuated mutant tul4 but the difference was not statistically significant. Comparing the 2 hrs time point with 6 and 24 hrs, we observed that U112, Δtul4 and ΔripA significantly increase their replication levels at 6 and 24 hrs P< 0.05. The Δ58kDa strain showed a significant increase in replication only after 24 hrs P<0.05. On the other hand, attenuated mutant strains ΔiglC and ΔmglA do not show any significant replication differences throughout the time points. (The statistical significance of increased replication between time points is not shown in the graph). The values are given in a log scale. * = P< 0.05, ** = P< 0.005 and *** = P< 0.0005
Figure 4: F. novicida and mutant strains replication in A549 lung epithelial cells. Bacterial localization was determined by immunofluorescence staining with a fluorescently labeled antibody against F. novicida LPS (green). Nuclei were stained with DAPI (blue). Images shown are F. novicida (U112) (A), ΔiglC (B), Δtul4 (C), ΔmglA(D) and Δ58kDa (E). Panels A through E were merged to DIC images. 400X. Representative images are from 24 hrs of replication.
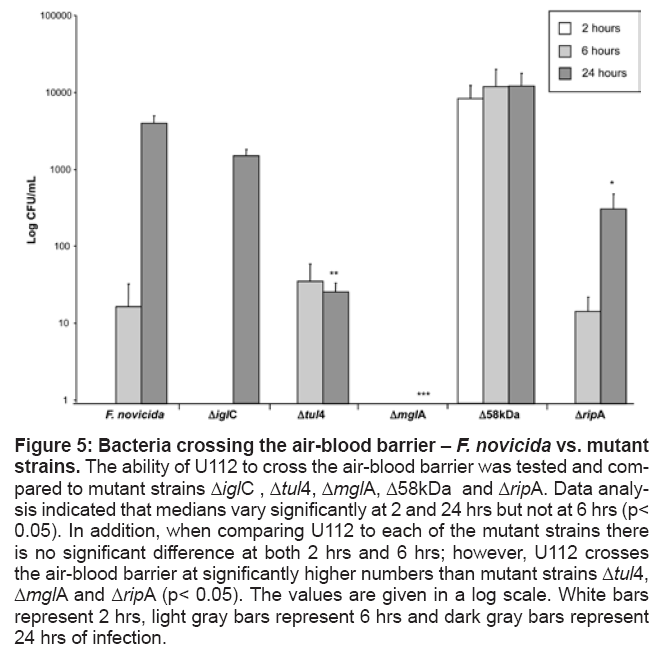
Ability of F. novicida and mutants to cross in vitro model of air-blood barrier
One of the key aspects of F.tularensis lethality is its ability to interact with the airway epithelium, enter the bloodstream and rapidly disseminate to distant organs such as liver and spleen [30]. To asses the ability of F. novicida to cross the air-blood barrier, we established an in-vitro cell co-culture composed of a top layer of A549 human airway epithelial cells grown on a transwell membrane and a bottom layer of HUVEC human endothelial cells grown on the opposite side of the membrane. This air-blood barrier model was infected through the apical side with F. novicida at an MOI of 1. The ability of F. novicida to cross the air-blood barrier was assessed by collecting all the volume present in the lower chamber of the transwell system, refilling with fresh media for the next time point, and by plating immediately after (0 hrs), 2 hrs, 6 hrs and 24 hrs of infection. Experimental results obtained at time 0 and 2 hrs revealed that the barrier was tight, as no bacteria were isolated from the lower chamber despite intracellular bacteria (Figure 5). By 6 hrs of infection, 101 CFU/ml of bacteria had crossed the air-blood barrier and by 24 hrs of infection the amount of bacteria present in the lower chamber had increased to 103 CFU/ml (Figure 5).
Figure 5: Bacteria crossing the air-blood barrier – F. novicida vs. mutant strains. The ability of U112 to cross the air-blood barrier was tested and compared to mutant strains ΔiglC , Δtul4, ΔmglA, Δ58kDa and ΔripA. Data analysis indicated that medians vary significantly at 2 and 24 hrs but not at 6 hrs (p< 0.05). In addition, when comparing U112 to each of the mutant strains there is no significant difference at both 2 hrs and 6 hrs; however, U112 crosses the air-blood barrier at significantly higher numbers than mutant strains Δtul4, ΔmglA and ΔripA (p< 0.05). The values are given in a log scale. White bars represent 2 hrs, light gray bars represent 6 hrs and dark gray bars represent 24 hrs of infection.
We also studied the role of the proteins IglC, MglA, Tul4, 58kDa and RipA in the capacity of F. novicida to cross this modeled air-blood barrier. By 2 hrs of infection, in contrast to the WT strain, the Δ58kDa mutant was the only strain capable of crossing the air-blood barrier, although the number of bacteria did not show a significant increase over time (Figure 5). On the other hand, by 6 hrs of infection, in addition to the WT strain, mutant strains Δ58kDa, Δtul4 and ΔripA were able to cross the air-blood barrier. Mutant strain Δ58kDa was isolated from the lower chamber at higher levels than the rest of the strains used (Figure 5) but statistical significance was not achieved. By 24 hrs of infection, mutant strains Δ58kDa, ΔiglC, ΔripA and Δtul4 crossed air-blood barrier, but statistical analyses revealed that the WT strain crossed the bilayer at significantly higher levels than the mutant strains ΔmglA, Δtul4 and ΔripA (p< 0.0005, p< 0.005 and p< 0.05 respectively) (Figure 5). These data suggests that 1) mglA is necessary for F. novicida in order to cross the air-blood barrier; 2) the absence of the 58kDa protein increases the ability of F. novicida to cross the bilayer; 3) the absence of IglC, Tul4 and RipA does not seem to have a major effect in Francisella’s ability to cross the air-blood barrier.
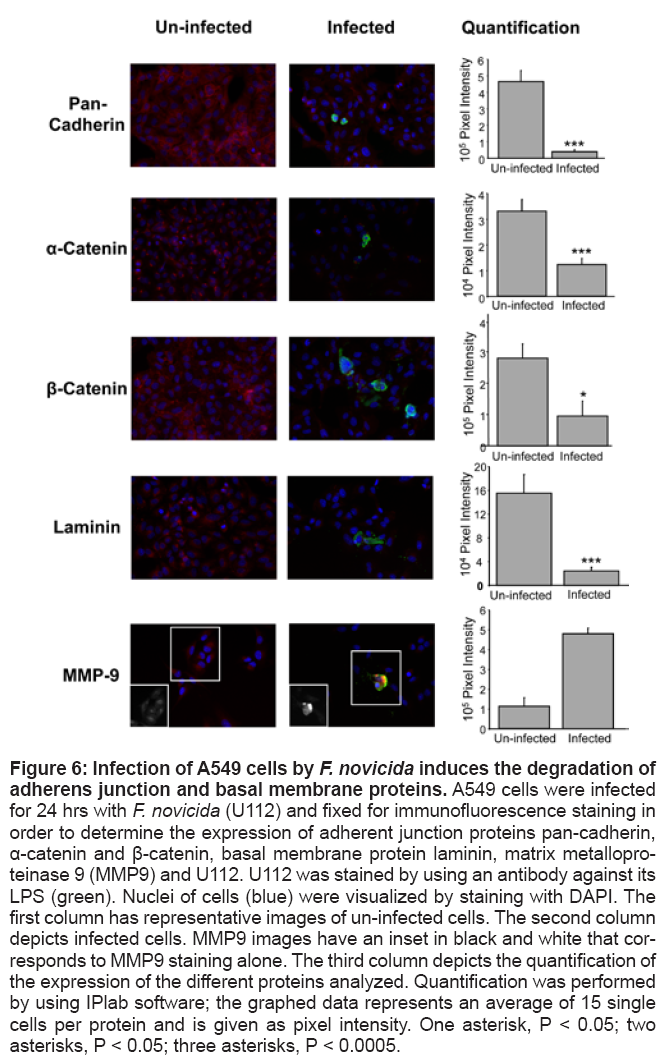
F. novicida infection of lung epithelial cells disrupts intraepithelial junction proteins
In an attempt to fully examine the mechanisms by which Francisella may cross the lung epithelial cell barrier, we also tested the effects of F. novicida infection on intraepithelial junction proteins. Adherens are members of junction protein complexes on the lateral membrane that occur at points of cell-to-cell contact [35]. A confluent monolayer of A549 cells on poly-L-lysine coated coverslips was infected with F. novicida for 24 hrs. Subsequently coverslips were fixed and stained for adherens junction proteins pan-cadherin, a-catenin and b-catenin and the basement membrane protein lamin. Our results showed that infected cells had a significant decrease in the expression of adherens junction proteins as well as laminin when compared with uninfected cells (Figure 6), suggesting a disruption of the cell-to cell contacts. Recent studies report that MMP-9 activity enhances host susceptibility to pulmonary infection with Francisella [36]. In addition, in vivo assays have shown that MMP-9 is one of the few proteins that are expressed early during respiratory tularemia [30]. Furthermore, recent studies show the ability of MMP9 to modulate tight junction integrity and cell viability in the human airway epithelia [37]. For these reasons, we decided to determine the presence of MMP-9 in infected cells. Our data showed that in fact MMP-9 expression is significantly increased in cells that contain intracellular F. novicida (Figure 6); however, cells that apparently do not have intracellular bacteria showed a decrease in the expression of MMP-9 when compared to uninfected cells. These data suggest that intracellular F. novicida could induce the expression of MMP-9.
Figure 6: Infection of A549 cells by F. novicida induces the degradation of adherens junction and basal membrane proteins. A549 cells were infected for 24 hrs with F. novicida (U112) and fixed for immunofluorescence staining in order to determine the expression of adherent junction proteins pan-cadherin, α-catenin and β-catenin, basal membrane protein laminin, matrix metalloproteinase 9 (MMP9) and U112. U112 was stained by using an antibody against its LPS (green). Nuclei of cells (blue) were visualized by staining with DAPI. The first column has representative images of un-infected cells. The second column depicts infected cells. MMP9 images have an inset in black and white that corresponds to MMP9 staining alone. The third column depicts the quantification of the expression of the different proteins analyzed. Quantification was performed by using IPlab software; the graphed data represents an average of 15 single cells per protein and is given as pixel intensity. One asterisk, P < 0.05; two asterisks, P < 0.05; three asterisks, P < 0.0005.
Discussion
This study used and in vitro model to understand the interaction between the respiratory pathogen F. novicida and the pulmonary epithelium. Our goal was to systematically examine the epithelial cell interaction with F. novicida in a stepwise manner. To characterize these interactions, we first investigated the ability of organisms to adhere and invade lung epithelial cells. We determined that U112 adheres to both cell types at similar levels than the non-pathogenic E. coli INV110, suggesting a passive adhesion to lung epithelial cells during infection. In contrast, we observed that U112 showed a higher invasion level to both cells lines suggesting that despite the passive mechanism it uses to attach to lung epithelial cells it is able to invade this cell type at relatively high rates. The results also showed that F. novicida is capable of replicating within A549 cells at an exponential rate. This is consistent with previous studies indicating that F.tularensis LVS has the ability to invade and replicate within alveolar epithelial cells [5,25]. In addition, recently Hall et al. [38], described the presence of F. novicida in lung epithelial cells as well as its replication within A549 cells.
The present study expanded on these findings by determining the role of known Francisella virulence factors including iglC, mglA, tul4, 58kDa and ripA in adhesion, invasion and intracellular replication. Our results showed that the F. novicida mutant strain Δtul4 adhered to A549 cells at significantly lower levels than the WT strain; since Tul4 is a membrane lipoprotein it could be serving not only as an antigen that can be recognized by T cells [27], but also as a ligand that facilitates the binding of F. novicida to lung epithelial cells. This proposed role is consistent with the finding that Tul4 stimulates the TLR2/TLR1 heterodimer [28]. In contrast, mutant strains ΔiglC, ΔmglA and ΔripA adhered to A549 cells at higher levels than the U112 strain suggesting that none of these proteins are required for F. novicida adhesion to A549 cells. These findings also suggests that adhesion to lung cells is a process tightly regulated by F. novicida, that the bacteria must gain an advantage by limiting its contact with epithelial cells, and that adhesion is a pathogenic mechanism that is distinct from invasion.
Despite the increased ability to adhere to A549 cells, mutant strain ΔmglA showed significantly lower levels of invasion. As MglA is the transcriptional regulator of most of the genes included in the FPI [26] and also regulates the transcription of other genes outside FPI (FTT0989, oppb and FTT1209c) [39], it is likely that MglA is regulating the expression of other virulence factors necessary for the invasion of lung epithelial cells. In addition, mutant strains Δ58kDa and Δtul4 showed significantly lower levels of invasion to A549 cells when compared to U112 strain. This is of interest as both Tul4 and the 58 kDa proteins are membrane lipoproteins and could potentially play synergistic roles for invasion of this cell type. In contrast, consistent with an increased adhesion to A549 cells, mutant strain ΔiglC showed significantly increased levels of invasion suggesting that this gene does not play a role in invasion.
One of the major aspects of F. novicida virulence is its ability to replicate within different cell types [5,6,33,34]. The results obtained in our experimental assays, showed an increased replication by U112 strain in A549 cells and that this replication increased in a time dependent manner. These data suggest that the capability of replicating within a non-phagocytic cell type, gives F. novicida an advantage to disseminate via the blood to other tissues in the host. It has been demonstrated that Francisella has a significant extracellular phase in blood [40]; therefore, it could disseminate to other tissues not only intracellularly in macrophages or dendritic cells but also extracellularly.
Subsequently, we examined the role of IglC, MglA, Tul4, 58kDa and RipA in intracellular replication. Our data showed that mutant strains ΔiglC and ΔmglA showed significantly lower levels of replication within A549 cells when compared to the WT strain. Moreover, replication levels did not show a significant change from one time point to the next time point tested. This suggests that IglC and its transcriptional regulator MglA are important for intracellular replication within A549 lung epithelial cells, similar to that observed in replication within phagocytic cells [21]. The deletion of RipA protein affected replication slightly (not adherence or invasion). Interestingly, similar results have been previously shown for the replication of the Francisella LVS mutant strain ΔripA in macrophages and murine lung epithelial cell line TC-1 [32].
Several studies have shown that Francisella disseminates to distant organs such as liver and spleen following an aerosol infection [11,30,41]. Other studies have shown that Francisella survives and replicates, among others, within macrophages and dendritic cells [6,33] and others point out the possibility that Francisella could use dendritic cells as a mean to disseminate inside the host [42]. In the present study we tested for the possibility that Francisella could enter the blood stream directly from the lungs and further disseminate. Our results showed that F. novicida is able to cross a two cell layer modeling the air-blood barrier as early as 6 hrs after infection, and the number of bacteria crossing the barrier increased with time. The increase in number of bacteria present on the lower chamber after 24 hrs of infection could be explained by the fact that F. novicida replicates within alveolar epithelial cells, and that bacteria cells could disrupt this monolayer facilitating the route to possibly continue infecting the endothelial cells and reaching the blood stream.
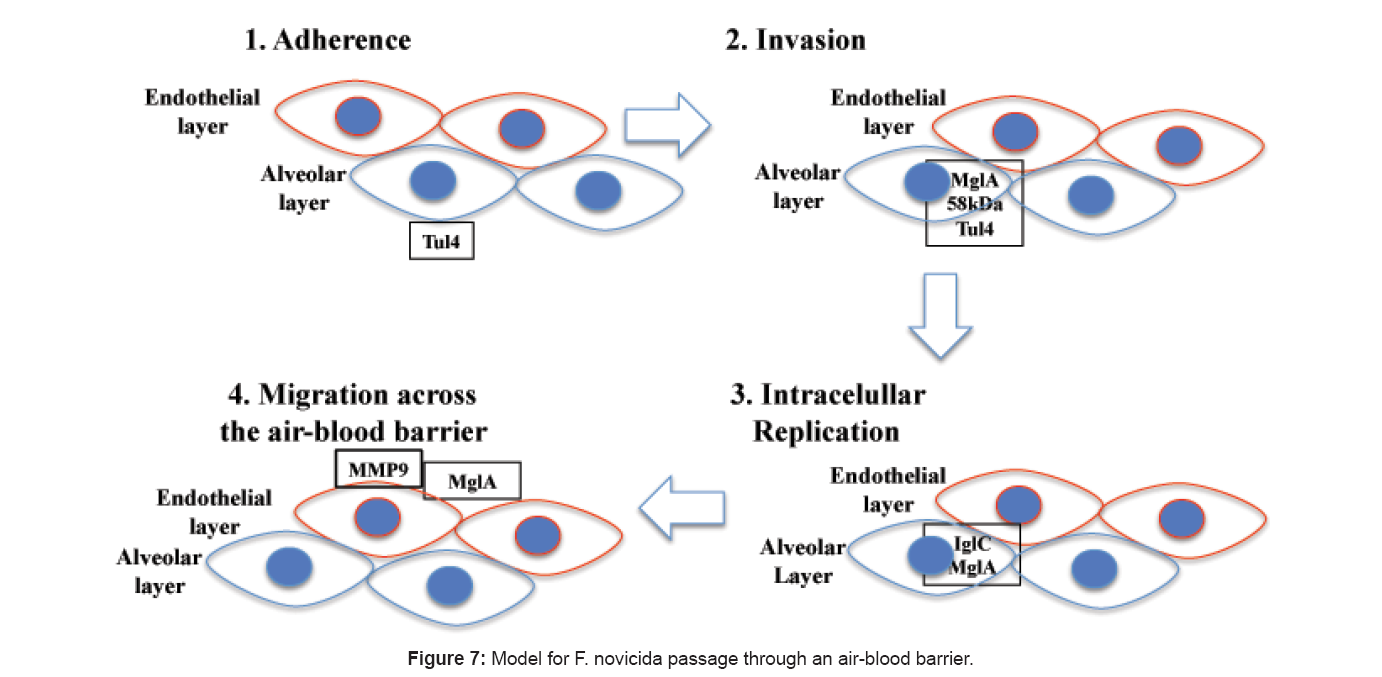
We also tested whether F. novicida could get across the air-blood barrier between the epithelial cells by disrupting the intraepithelial junction proteins. Immunofluorescence staining of adherens junction proteins pan-cadherin, a and b-catenins in A549 cells infected with F. novicida after 24 hrs showed a significant decrease in their expression compared to uninfected cells (Figure 6). Recent studies report that MMP-9 activity enhances the host susceptibility to pulmonary infection with Francisella [36]. In addition it has been shown that some bacterial pathogen proteinases can generate the active form of MMP-9 which is then implicated in tissue injury [43]. Furthermore, in vivo assays show that MMP-9 is one of the few proteins whose expression is increased in lung homogenates and bronchoalveolar lavage fluid (BALF) of mice early after infection [30]. Immunofluorescence staining of A549 cells uninfected and infected with F. novicida after 24 hrs showed that cells containing intracellular bacteria had an increased expression of MMP-9 compared to uninfected cells (Figure 6). Altogether, these data suggest that a possible mechanism F. novicida uses to cross the air-blood barrier is by inducing an increase in the expression of MMP- 9 which results in disruption of intraepithelial junction proteins as well as the basal membrane protein. Finally, we propose a model for F. novicida passage across an air-blood barrier (Figure 7); following respiratory infection with F. novicida and when the bacterium gets in close proximity to the alveolar epithelium, its membrane lipoprotein Tul4 mediates its adherence to this barrier of cells. Once the bacteria are attached, invasion is mediated through the transcriptional regulator MglA and the membrane lipoproteins 58kDa and Tul4. Subsequently, intracellular replication within these cells is mediated by MglA and IglC proteins. Then, for translocation to the apical side, the bacteria induces the expression of MMP9 and it also requires MglA.
Acknowledgements
This work was supported by a NIH AI 59703, PO1 AI057986, NS 35974 and in part by San Antonio Life Science Institute (10003177).
We thank Marco Leung, Elizabeth Morris, Michelle Georges and Ernesto Hinojosa for their technical support. We also thank Dr. Jyotika Sharma for her advice.
References
- Zeidner N S, Carter L G, Monteneiri J A, Petersen J M, Schriefer M, et al. (2004) An outbreak of Francisella tularensis in captive prairie dogs: an immunohistochemical analysis. J Vet Diagn Invest 16: 150-152.
- Oyston P C, Sjostedt A, Titball RW (2004) Tularaemia: bioterrorism defence renews interest in Francisella tularensis. Nat Rev Microbiol 2: 967-978.
- Abd H, Johansson T, Golovliov I, Sandstrom G, and Forsman M (2003) Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl Environ Microbiol 69: 600-606.
- Lauriano C M, Barker J R, Yoon S S, Nano F E, Arulanandam B P, et al. (2004) MglA regulates transcription of virulence factors necessary for Francisella tularensis intraamoebae and intramacrophage survival. Proc Natl Acad Sci 101: 4246-4249.
- Hall J D, Craven R R, Fuller J R, Pickles R J, Kawula T H (2007) Francisella tularensis replicates within alveolar type II epithelial cells in vitro and in vivo following inhalation. Infect Immun 75: 1034-1039.
- Bosio C M, Dow S W (2005) Francisella tularensis induces aberrant activation of pulmonary dendritic cells. J Immunol 175: 6792-6801.
- Sjostedt A (2006) Intracellular survival mechanisms of Francisella tularensis, a stealth pathogen. Microbes Infect 8: 561-567.
- Chen W, KuoLee R, Shen H, Conlan J W (2004) Susceptibility of immunodeficient mice to aerosol and systemic infection with virulent strains of Francisella tularensis. Microb Pathog 36: 311-318.
- Ellis J, Oyston P C, Green M, Titball R W (2002) Tularemia. Clin Microbiol Rev 15: 631-646.
- Dennis D T, Inglesby T V, Henderson D A, Bartlett J G, Ascher M S, et al. (2001) Tularemia as a biological weapon: medical and public health management. JAMA 285: 2763-2773.
- Elkins K L, Cowley S C, Collazo C M (2003) Francisella: a little bug hits the big time. Expert Rev Vaccines 2: 735-738.
- Tarnvik A (1989) Nature of protective immunity to Francisella tularensis. Rev Infect Dis 11: 440-451.
- Mares C A, Ojeda S S, Morris E G, Li Q, Teale JM (2008) Initial delay in the immune response to Francisella tularensis is followed by hypercytokinemia characteristic of severe sepsis and correlating with upregulation and release of damage-associated molecular patterns. Infect Immun 76: 3001-3010.
- Knight D A, Holgate S T (2003) The airway epithelium: structural and functional properties in health and disease. Respirology 8: 432-446.
- Diamond G, Legarda D, Ryan L K (2000) The innate immune response of the respiratory epithelium. Immunol Rev 173: 27-38.
- Craven R R, Hall J D, Fuller J R, Taft-Benz S, Kawula T H (2008) Francisella tularensis invasion of lung epithelial cells. Infect Immun 76: 2833-2842.
- Lindemann S R, McLendon M K, Apicella M A, Jones B D (2007) An in vitro model system used to study adherence and invasion of Francisella tularensis live vaccine strain in nonphagocytic cells. Infect Immun 75: 3178-3182.
- Broekhuijsen M, Larsson P, Johansson A, Bystrom M, Eriksson U, et al. (2003) Genome-wide DNA microarray analysis of Francisella tularensis strains demonstrates extensive genetic conservation within the species but identifies regions that are unique to the highly virulent F.tularensis subsp. tularensis. J Clin Microbiol 41: 2924-2931.
- Forsman M, Sandstrom G, Sjostedt A (1994) Analysis of 16S ribosomal DNA sequences of Francisella strains and utilization for determination of the phylogeny of the genus and for identification of strains by PCR. Int J Syst Bacteriol 44: 38-46.
- Gallagher L A, Ramage E, Jacobs M A, Kaul R, Brittnacher M, et al. (2007) A comprehensive transposon mutant library of Francisella novicida, a bioweapon surrogate. Proc Natl Acad Sci 104: 1009-1014.
- Lauriano CM, Barker J R, Nano F E, Arulanandam B P, Klose K E (2003) Allelic exchange in Francisella tularensis using PCR products. FEMS Microbiol Lett 229: 195-202.
- Schultheiss D, Handrick R, Jendrossek D, Hanzlik M, and Schuler D (2005) The presumptive magnetosome protein Mms16 is a poly(3-hydroxybutyrate) granule-bound protein (phasin) in Magnetospirillum gryphiswaldense. J Bacteriol 187: 2416-2425.
- Giard DJ, Aaronson S A, Todaro G J, Arnstein P, Kersey JH, et al. (1973) In vitro cultivation of human tumors: establishment of cell lines derived from a series of solid tumors. J Natl Cancer Inst 51: 1417-1423.
- Stoner G D, Kikkawa Y, Kniazeff A J, Miyai K, Wagner RM (1975) Clonal isolation of epithelial cells from mouse lung adenoma. Cancer Res 35: 2177- 2185.
- Gentry M, Taormina J, Pyles R B, Yeager L, Kirtley M, et al. (2007) Role of primary human alveolar epithelial cells in host defense against Francisella tularensis infection. Infect Immun 75: 3969-3978.
- Nano F E, Schmerk C (2007) The Francisella pathogenicity island. Ann N Y Acad Sci 1105: 122-137.
- Sjostedt A, Tarnvik A, Sandstrom G (1991) The T-cell-stimulating 17-kilodalton protein of Francisella tularensis LVS is a lipoprotein. Infect Immun 59: 3163- 3168.
- Thakran S, Li H, Lavine C L, Miller M A, Bina J E, et al. (2008) Identification of Francisella tularensis lipoproteins that stimulate the toll-like receptor (TLR) 2/ TLR1 heterodimer. J Biol Chem 283: 3751-3760.
- Liu J, Zogaj X, Barker J R, and Klose K E (2007) Construction of targeted insertion mutations in Francisella tularensis subsp. novicida Biotechniques 43: 487-492.
- Sharma J, Li Q, Mishra B B, Pena C, Teale J M (2009) Lethal pulmonary infection with Francisella novicida is associated with severe sepsis. J Leukoc Biol 86: 491-504.
- Twine S, Bystrom M, Chen W, Forsman M, Golovliov I, et al. (2005) A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect Immun 73: 8345-8352.
- Fuller J R, Craven R R, Hall J D, Kijek T M, Taft-Benz S, et al. (2008) RipA, a cytoplasmic membrane protein conserved among Francisella species, is required for intracellular survival. Infect Immun 76: 4934-4943.
- Anthony L D, Burke R D, Nano F E (1991) Growth of Francisella spp. in rodent macrophages. Infect Immun 59: 3291-3296.
- Bolger C E, Forestal C A, Italo J K, Benach J L, Furie M B (2005) The live vaccine strain of Francisella tularensis replicates in human and murine macrophages but induces only the human cells to secrete proinflammatory cytokines. J Leukoc Biol 77: 893-897.
- Groschwitz K R, Hogan S P (2009) Intestinal barrier function: molecular regulation and disease pathogenesis. J Allergy Clin Immunol 124: 3-20.
- Malik M, Bakshi C S, McCabe K, Catlett S V, Shah A, et al. (2007) Matrix metalloproteinase 9 activity enhances host susceptibility to pulmonary infection with type A and B strains of Francisella tularensis. J Immunol 178: 1013-1020.
- Vermeer PD, Denker J, Estin M, Moninger TO, Keshavjee S, et al. (2009) MMP9 modulates tight junction integrity and cell viability in human airway epithelia. Am J Physiol Lung Cell Mol Physiol 296: L751-L762.
- Hall J D, Woolard M D, Gunn B M, Craven R R, Taft-Benz S, et al. (2008) Infected-host-cell repertoire and cellular response in the lung following inhalation of Francisella tularensis Schu S4, LVS, or U112. Infect Immun 76: 5843-5852.
- Brotcke A, Weiss D S, Kim C C, Chain P, Malfatti S, et al. (2006) Identification of MglA-regulated genes reveals novel virulence factors in Francisella tularensis. Infect Immun 74: 6642-6655.
- Forestal C A, Malik M, Catlett S V, Savitt A G, Benach J L, et al. (2007) Francisella tularensis has a significant extracellular phase in infected mice. J Infect Dis 196: 134-137.
- Ojeda S S, Wang Z J, Mares C A, Chang T A, Li Q, et al. (2008) Rapid dissemination of Francisella tularensis and the effect of route of infection. BMC Microbiol 8: 215.
- Bar-Haim E, Gat O, Markel G, Cohen H, Shafferman A, et al. (2008) Interrelationship between dendritic cell trafficking and Francisella tularensis dissemination following airway infection. PLoS Pathog 4: e1000211.
- Okamoto T, Akuta T, Tamura F, van D, V Akaike T (2004). Molecular mechanism for activation and regulation of matrix metalloproteinases during bacterial infections and respiratory inflammation. Biol Chem 385: 997-1006.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 14869
- [From(publication date):
specialissue-2012 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 10175
- PDF downloads : 4694