Research Article Open Access
The Prevalence of Unexpected Sexually Transmitted Diseases in Women with Lower Urinary Tract Complaints Suggestive of UTI is High
Weigler G, Perry C, Weigler A, Kim B, Yangouyian M, Vicena J, and Richard Santucci*
Detroit Medical Center, Michigan State University College of Osteopathic Medicine, Michigan, USA
- *Corresponding Author:
- Richard Santucci
M.D., F.A.C.S
Specialist-in-Chief, Urology
Detroit Medical Center, Clinical Professor
Michigan State University College of Osteopathic Medicine
4160 John R. Suite 1017, Detroit
Michigan 48201, USA
Tel: 313-745-4123
Fax: 313-745-8222
E-mail: rsantucc@dmc.org
Received date: August 14, 2013; Accepted date: September 18, 2013; Published date: September 20, 2013
Citation: Weigler G, Perry C, Weigler A, Kim B, Yangouyian M, et al. (2013) The Prevalence of Unexpected Sexually Transmitted Diseases in Women with Lower Urinary Tract Complaints Suggestive of UTI is High. J Community Med Health Educ 3:240. doi:10.4172/2161-0711.1000240
Copyright: © 2013 Weigler G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objective: To examine the prevalence of unrecognized sexually transmitted diseases in women who present to the emergency room with urinary complaints, which generally would be treated only for urinary tract infection. Methods: An eight month, prospective study was performed in a community, teaching hospital emergency department. Sexually active women, ages 18-45, who presented with urinary complaints were solicited for participation. Physician-administered questionnaires queried the demographic, gynecologic, obstetric, sexual history, and presenting symptoms. Patient complaints, physical findings, laboratory results (urinalysis, urine culture, serum Venereal Disease Research Laboratory (VDRL), and cervical cultures for Nisseria gonorrhea, Chlamydia trachomatis, and Trichomonas) were reviewed. Results: A total of 49 patients (66% African American, 28% Caucasian, and 6% other) who met the inclusion criteria were enrolled. The mean age of our participants was 25 years. The range of sexual partners in one’s lifetime was 1 to 50, with a mean of 12.8 partners. Forty-eight percent had a history of a Sexually Transmitted Disease (STD) and 18% had active disease (C. trachomatis 8%, syphilis 2%, and Trichomonas 8%). There was no relationship between the history of a STD and positive cultures or recurrent STD. Thirty-four percent were confirmed to have a UTI. Fourteen percent were co-infected with both a STD and a UTI. Conclusion: The prevalence of occult STDs in women presenting with urinary complaints who underwent pelvic examination was 18%. The evidence emphasizes the importance of diagnosing STDs with performing a pelvic examination and culture on sexually active females with nonspecific urinary complaints, who otherwise might be misdiagnosed as having a simple urinary tract infection.
Keywords
Sexually transmitted diseases; Urinary tract infections; Emergency department; Prevalence; women
Introduction
Urinary Tract Infections (UTIs) account for over 1 million visits to the emergency department every year [1]. While most adults with UTI symptoms can be presumptively treated for simple UTI based on symptoms alone, some retrospective studies have shown that lower urinary tract complaints suggestive of UTI may be the only symptoms present in otherwise asymptomatic Sexually Transmitted Diseases (STDs) in the sexually active female [2,3]. There is danger of misdiagnosis these patients with a simple urinary tract infection, and not treating primary or co-existent STD.
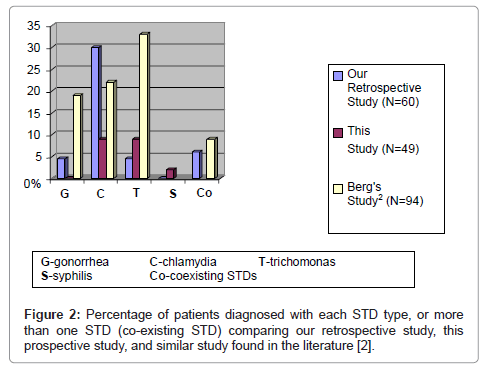
Previously, we performed a preliminary retrospective chart review [3] examining the prevalence of STDs in women who presented to the ED with complaints suggestive of urinary tract infections over a 6 month span. Cervical cultures were taken for N. gonorrhea, C. trachomatis, and Trichomonas. Thirty-nine percent of these patients were found to have a STD (N. gonorrhea 4.5%, C. trachomatis 29.9%, and Trichomonas 4.5%). Six percent of patients had multiple STD infections.
The goal of this prospective study is to validate the findings of our previous retrospective review that STDs have a significant prevalence in the etiology of lower urinary tract symptoms in the sexually active female who presents to the emergency department with said complaints. We hypothesize that women presenting with UTI symptoms will have a high percentage of primary or co-existent STD.
Methods
Using Berg et al. [2] and our own previous retrospective study [3] as models, a prospective study was designed in a community teaching hospital Emergency Department (ED) in conjunction with the department of urology. Garden City Hospital Emergency Department, with >45,000 patient visits per year, is located in a suburb of Detroit, Michigan. The hospital’s Internal Review Board granted approval for the study. All participants signed consents and were provided an opportunity to ask any questions regarding the study prior to signing the informed consent.
Sexually active women, ages 18-45 years of age, who presented to the ED with urinary complaints were enrolled in the study. Physicianadministered questionnaires queried the demographic, gynecologic, obstetric, and sexual history, and their presenting symptoms. Specifically, questions were asked regarding the patient’s age, race, sexual preference, lifetime number of sexual partners, number of sexual partners in the last 2 months, gestational history, history of STDs, and physical complaints. Presenting complaints surveyed included suprapubic tenderness, pelvic pain, back pain, dysuria, urgency, frequency, pelvic pain, hematuria, and vaginal discharge. Physical findings concentrated on vital signs, abdominal exam, and pelvic exams. Laboratory studies included urinalysis, urine culture, cervical cultures, and serum VDRL, all completed at our College of American Pathologists (CAP) and Clinical Laboratory Improvement Amendment (CLIA) certified lab.
Cervical cultures were obtained using cotton swabs during speculum exam. BD BBL™ Trichosel™Broth, modified with 5% Horse Serum (Becton, Dickinson and Company; Sparks, MD) was used to isolate Trichomonas. Gen-Probe® (Gen-Probe Incorporated; San Diego, California) was used in the detection of N. gonorrhea and C. trachomatis. Statistics analysis was supervised by Michigan State University College of Human Medicine, Department of Epidemiology and Biostatistics using IBM SPSS Statistics V 21.
Results
Forty-nine patients were enrolled in the study over an eight month period. The participants consisted of 66% African American, 28% Caucasian, and 6% other. The mean age was 25.2 years. The range of sexual partners per patient was 1 to 50, with a mean of 12.8 partners. Six participants refused to give information regarding number of partners. There existed a wide range of presenting symptoms, with suprapubic tenderness being the most common (Table 1).
| Symptoms at Presentation | Prevalence |
|---|---|
| Suprapubic Tenderness | 70% |
| Urinary Frequency | 48% |
| Urgency | 46% |
| Dysuria | 42% |
| Back Pain | 42% |
| Hematuria | 8% |
Table 1: Symptoms at presentation of 49 prospectively studied females with a clinical picture consistent with UTI.
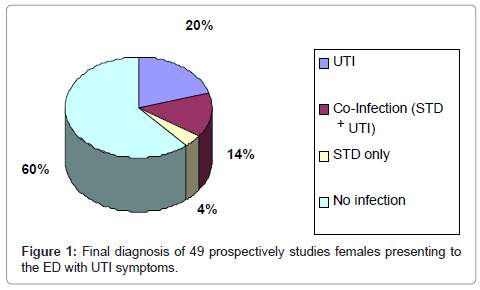
Forty-eight percent gave a history of a prior STD infection(s), but only 18% were found to be currently infected at the time of investigation (C. trachomatis 8%, syphilis 2%, Trichomonas 8%). There was no relationship between a previous history of a STD and positive cultures or recurrent STD (p<0.05). Thirty-four percent of patients had a suspected UTI on urinalysis that was later confirmed by culture. The urine cultures were positive for E. coli in all cases. Fourteen percent of patients diagnosed with a STD were also diagnosed with a UTI (Figure 1). The remaining 60% of patients had UTI as the sole identifiable cause of their presenting complaints.
Discussion
STDs can have severe consequences to the patient when undiagnosed [4]. Our data show that 18% of sexually active women presenting to the ED with urinary tract infection complaints were found to have an STD. This adds support to the notion that STDs can be difficult to diagnose [2,5] and emphasizes the likelihood of misdiagnosis of STD because symptoms are often absent or easily misidentified as a simple urinary tract infection.
Comparisons between this prospective study (n=49), our previous retrospective study (n=60), and that of Berg et al. [2] (n=94) is seen in Figure 2. Berg et al. [2] examined females presenting to the ED with lower urinary complaints at a nearby but more urban locale hospital. They found that 53% had STD as the cause. All the studies showed high levels of STDs in general, with differing ratios of gonorrhea, Chlamydia and Trichomonas (the Berg study did not examine for syphilis) (Figure 2). Our county (Wayne County, Michigan) was reported by the US Center for Disease Control (CDC) to have the highest number of reported cases of primary and secondary syphilis in 2001 (Figure 3) [6], which was seen as a 2% rate of syphilis is our study. There were minor differences in the patters of STD presentation. None of our patients in this prospective study had N. gonorrhea infections, or more than one simultaneous STD infections [2,3]. These differences are probably less important than our main conclusion that a wide variety of different STDs can be present in patients with UTI symptoms.
STDs continue to pose serious long term health consequences including pelvic inflammatory disease, infertility, ectopic pregnancy, salpingitis, and perinatal infections [4]. Adolescents are especially at risk. The Youth Risk Behavior Surveillance Survey in 1997 showed that nearly 50% of high school students questioned admitted to being sexually active. Fifty-seven percent of the sexually active teens reported that neither they, nor their partner, used a condom the last time they engaged in sexual intercourse [7]. Combined with the risky behavior of multiple partners, STDs occur in epidemic proportions [8]. UTIs have been shown to be a marker of sexual activity in the teenage population [9], and these data show that UTI symptoms or culture-proven diagnosis should also be a trigger for STD screening in adult or teenage populations.
These facts make it incumbent on the ED physician, the family physician, the gynecologist/obstetrician, and the urologist to recognize that the diagnosis of STDs is not always straightforward and that it may actually be manifesting as urinary symptoms. A thorough history should include questions regarding current symptoms, sexual history, obstetric and gynecologic history, number of partners, use of contraceptives, previous STDs, and UTIs. The physical exam should focus on the patient’s vital signs, abdomen, flanks, and genitalia. While the abdomen and flanks should be palpated for tenderness, the genitals should be inspected for any lesions and discharge. Cervical swabs should culture for Trichomonas and consist of DNA probes for N. gonorrhea and C. trachomatis. In addition to other lab work that may be performed, Venereal Disease Research Laboratory (VDRL) tests should be included to screen for syphilis.
This study contains certain limitations. First, the study was designed to look for STDs in women specifically presenting with UTI symptoms. We do not know the baseline prevalence of STDs in all sexually active women presenting to our ED. Theoretically, it is possible for the rate to be the same as in our study. Berg et al. also made this observation in his study [2]. Second, findings are limited to this single institution, although our findings are similar to those reported by other centers.
Conclusion
UTIs account for one of the most common presenting etiologies to the ED. Eighteen percent of sexually active women presenting to the ED with UTI symptoms were found to have STDs that may have otherwise gone undiagnosed. This highlights the importance of performing a thorough history, physical, and obtaining laboratory data, including cervical cultures and VDRL, in order to recognize this often times difficult to diagnose entity. Failure to recognize and treat STD infections can have potentially detrimental consequences, especially in the adolescent and younger adult patient.
References
- Howes HS, William YF (1999) Urinary tract infections. In: Tintinalli JE A comprehensive study guide in emergency medicine, 5th ed., Dallas: American College of Emergency Physicians, 625-630.
- Berg E, Benson D, McDonald J, Haraszkiewicz P, Grieb J (1996) High prevalence of sexually transmitted diseases in women with urinary infections. Acad Emerg Med 3: 1030-1034.
- Weigler A, Perry C, Kim B, Yangouyian M (2005) Prevalence of sexually transmitted diseases in women with urinary complaints: a retrospective study. Poster presentation at the American College of Osteopathic Emergency Physicians.
- Berger RE, Jay LC (2002) Sexually transmitted diseases: the classic diseases. In: Walsh P, Retik A, Vaughan, Jr. E, Wein A, Campbell’s urology. Saunders 1: 671-687.
- Centers for Disease Control and Prevention (1993) 1993 sexually transmitted diseases treatment guidelines. Centers for Disease Control and Prevention. MMWR Recomm Rep 42: 1-102.
- Centers for Disease Control and Prevention (CDC) (2002) Primary and secondary syphilis-United States, 2000-2001. MMWR Morb Mortal Wkly Rep 51: 971-973.
- Centers for Disease Control (1997) Youth Risk Behavior Surveillance: National College Health Risk Behavior Survey-United States, 1995. MMWR CDC Surveill Summ46: 1-56.
- Duffy EM, McCollough M (2000) Sexually transmitted diseases in adolescents. The Practical J of Ped Em Med 4: 31-39.
- Nguyen H, Weir M (2002) Urinary tract infection as a possible marker for teenage sex. South Med J 95: 867-869.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 15538
- [From(publication date):
November-2013 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10969
- PDF downloads : 4569