Research Article Open Access
The Impact of a One-Day Applied Training in Motivational Interviewing on Health Practitioners’ Perceived Competence, Autonomy, Efficacy, and Attitudes to Facilitate Behavior Change: A Pilot Study
Erin J Wiley, Don Morrow and Jennifer D Irwin*School of Health Studies, Room 207, Arthur and Sonia Labatt Health Sciences Building, University of Western Ontario, London, Ontario, Canada, N6A5B9
- *Corresponding Author:
- Dr. Jennifer D Irwin, PhD
School of Health Studies, Room 207
Arthur and Sonia Labatt Health Sciences Building
University of Western Ontario
London, Ontario, Canada, N6A5B9
Tel: 519-661-2111 ext. 88367
Fax: 519-850-2432
E-mail: jenirwin@uwo.ca
Received date: November 04, 2011; Accepted date: November 16, 2011; Published date: November 18, 2011
Citation: Wiley EJ, Morrow D, Irwin JD (2011) The Impact of a One-Day Applied Training in Motivational Interviewing on Health Practitioners’ Perceived Competence, Autonomy, Efficacy, and Attitudes to Facilitate Behavior Change: A Pilot Study. J Community Med Health Edu 1:101. doi: 10.4172/jcmhe.1000101
Copyright: © 2011 Wiley EJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objective: Because the practical application of motivational interviewing (MI) for health practitioners has been highlighted as a limitation to the approach, the purpose of this pilot study was to assess the impact of a one-day training workshop in MI applied through Co-Active life coaching (CALC) skills on health care practitioners’ perceived competence, autonomy and attitudes toward facilitating health-behavior changes.
Methods: A pre-test/post-test multiple baseline design was used with 10 health care practitioners. Data was collected beginning 25 days prior and for 4 weeks post-training. Participants received a 7.5 hour interactive workshop in January 2011. The Perceived Competence Scale, the Perceived Autonomous Motivation Scale and the Nutrition in Patient care Survey were adapted and administered to assess attitudes toward facilitating health-behavior changes in clinical care.
Results: Significant increases in perceived competence [Cohen’s effect size d =4.61], perceived autonomy [ d =1.62], practitioner efficacy [ d =2.22], and behavior change in routine care [ d =1.69] were reported and remained clinically significant four weeks after the training.
Conclusion: Participation in this applied workshop was effective and should be explored further with a larger group.
Practice Implications: This training improved practitioners’ comfort to counsel behavior changes and may be a useful training model for health professionals.
Keywords
Patient-Practitioner Communication; Health Behavior Counseling; Training; Workshop; Motivational Interviewing; Coaching.
Introduction
The majority of health conditions causing disease and death in Canada and western society are, at least in part, behaviorallymodifiable [1-3]. Usage of primary health care consultation in Canada is high [4]. In 2005, 77% of Canadians aged 18 to 64 years reported that they had consulted a general practitioner in the previous year. Unfortunately, recent research suggests that lifestyle counseling by physicians is minimal [5-7]. The lack of behavior change counseling may be explained in part by the minimal amount of time physicians and patients spend together during a primary care visit, often not more than 10 minutes [8,9]. Other health care professionals such as pharmacists, nurses, and dietitians have been identified as particularly accessible, and interact with patients for a longer duration during visits [8,10] placing them in a good position to provide motivational support [11,12]. Consequently, non-physician health professionals are in a key position to be involved in behavior change counseling [13-15].
One communication technique receiving increased support for assisting health practitioners with behavior change conversations is Motivational Interviewing (MI) [16]. MI is used to resolve ambivalence and a growing body of evidence supports the position that MI principles are effective for activating various health-related behavior changes in individuals including lowering dietary fat intake [17], improving adherence to medication regimes [18], enhancing compliance with exercise programs [19], as well as several other healthrelated improvements [20,21].
Although MI is well described, and has been widely researched in the health care field, health care professionals receive varied and often minimal training towards its practical application [22]. Research indicates that a major challenge with MI in a setting such as daily clinical practice is the lack of understanding about how to integrate the concepts into practice [23]. This may explain the inconsistent results of MI interventions [23-25].
Co-Active Life Coaching (CALC) [26] is a theoretically grounded behavior change method [27]. Recent research has found that a probable reason for much of CALC’s effectiveness lies in the fact that its tools provide tangible methods to bring the tenets of MI to practical use [27,28]. The current study was part of a mixed-methods investigation to explore qualitatively and quantitatively, the impact of a one-day CACL workshop on practitioners’ experiences of behavior change [29].
The purpose of this study was to assess quantitatively the impact of a one-day training workshop in MI applied through CALC skills on health care practitioners’ perceived competence, autonomy and attitudes toward facilitating health-behavior changes among patients in daily clinical practice. It was hypothesized that improvements would be reported in attitudes, perceived competence, and autonomy to facilitate health behavior changes among patients.
Methods
A pre-test/post-test multiple baseline design was employed to examine the impact of MI via CALC tools training workshop on various aspects of participants’ attitudes toward behavior change facilitation in daily clinical practice. Ten health care practitioners from various specialties volunteered to take part in the study; all were female; five registered nurses; two pharmacists; two social workers; and one dietitian. Participants ranged in age from 26- 65 years with 60% between ages 38-55. Ninety percent of participants had 10 or more years of fulltime experience in their current specialty and one participant had two years’ experience. Two participants had previous MI training which consisted of one hour or less. Full participant demographic details are presented in Table 1.
| Demographics | # |
|---|---|
| Gender Male Female |
0 10 |
| Participant Age (years) 25-34 35-44 45-54 55-65 |
1 3 3 3 |
| Years of Full Time Work In Current Specialty 0-5 6-15 16-25 26-30 35-40 |
1 2 3 2 2 |
| Health Care Practitioner Role Dietitian Pharmacist Registered Nurse Social Worker |
1 2 5 2 |
| First Language English Other |
10 0 |
| Ethnicity or Self-Identified Cultural Group Caucasian Italian |
9 1 |
| Previous Motivational Interviewing or Co-Active Life Coaching Training No Yes |
8 2 |
| Length of Previous Training 0-1 hour |
Table 1: Demographic Information of Health Care Practitioners (n=10.)
Participants were eligible if they were health care practitioners working full-time and had an interest in improving their patientcommunication and facilitating behavior change in their patients.
Two certified Co-Active coaches, with extensive experience facilitating workshops focused on the application of MI through CALC for health care practitioners, provided a seven and a half hour interactive training workshop. Together, this team has conducted many MI/CALC workshops (n > 20), most geared to multidisciplinary health care professionals. Health care practitioners were recruited within the Thames Valley Family Health Team and attended the training workshop in MI via CALC tools.
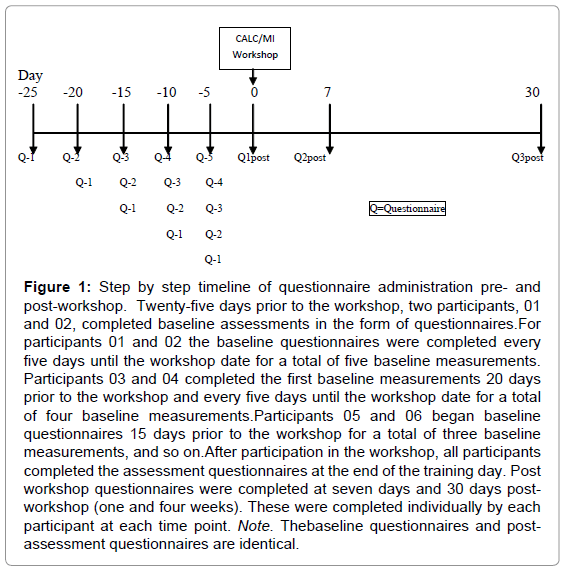
Participants engaged in between one and five baseline measurements with the first baseline questionnaire completed 25 days prior to participation in the workshop. Upon completion of the workshop, participants filled out the same questionnaires again, immediately after the workshop. Thereafter, at weeks one (seven days) and four (30 days) post-workshop questionnaire were completed by each participant. A visual timeline outlining the study structure and data collection period is provided in Figure 1.
Figure 1: Step by step timeline of questionnaire administration pre- and post-workshop. Twenty-five days prior to the workshop, two participants, 01 and 02, completed baseline assessments in the form of questionnaires.For participants 01 and 02 the baseline questionnaires were completed every five days until the workshop date for a total of five baseline measurements. Participants 03 and 04 completed the first baseline measurements 20 days prior to the workshop and every five days until the workshop date for a total of four baseline measurements.Participants 05 and 06 began baseline questionnaires 15 days prior to the workshop for a total of three baseline measurements, and so on.After participation in the workshop, all participants completed the assessment questionnaires at the end of the training day. Post workshop questionnaires were completed at seven days and 30 days postworkshop (one and four weeks). These were completed individually by each participant at each time point. Note. Thebaseline questionnaires and postassessment questionnaires are identical.
Multiple baseline single subject design
This study utilized a multiple baseline single subject research design to determine consistency in practitioners’ self-reported motivation, efficacy, and competency towards working with patients to facilitate health behavior changes prior to the intervention [30,31]. Multiple baseline measurement methodology has been shown to be both reliable and effective in assessing experimentally the types of changes under investigation in this study [30,31].
Measures
Perceived competence scale (PCS): The Perceived Competence Scale (PCS) [32] was adapted and used to assess participants’ competency to facilitate behavior changes among their patients. This is a previously validated, short questionnaire based on self-determination theory with an internal consistency value of 0.8 [32-34]. Items on the PCS are written to be specific to the relevant behavior or domain being studied and thus an adaptation was made so that the scale would address perceived competence to facilitate health behavior changes.
Perceived autonomous motivation scale: The Perceived Autonomous Motivation Scale [35] measured practitioners’ level of perceived internal motivation to pursue behavior change counseling among their patients. The scale is validated and reliable and has been used in a recent study investigating physician motivation to counsel tobacco dependent patients to quit [35]. This scale was adapted to reflect behavior counseling in clinical practice.
Adapted nutrition in patient care survey (NIPS): The Nutrition in Patient care Survey (NIPS) [36] was adapted to address practitioners’ attitudes toward facilitating health behavior changes in routine clinical care. NIPS is a validated tool containing five subscales to assess nutrition in routine care, clinical behavior, practitioner patient relationship, patient behavior/motivation and practitioner efficacy [36]. This tool has good internal consistency and test-retest reliability. The test-retest reliability for the subscale ‘Nutrition in routine care’ has been shown to be 0.80 when tested on 107 medical students [36]. For ‘Physician-patient relationship’ the reliability was reported at 0.55. The reliability is 0.50 and is 0.64 for ‘Patient behavior/motivation’ and ‘Physician efficacy’ respectively. This scale is considered useful to predict patient care practices and to evaluate research on clinical or education interventions [36]. Four of the NIPS subscales questions were adapted. The only adaptations were that the words ‘nutrition counseling’ was changed to ‘behavior change facilitation’ and the word ‘physician’ was changed to ‘health care practitioner’ to address the topic of behavior change facilitation. The subscales are entitled: a) Behavior change in routine care; b) Practitioner-patient relationship; c) Patient behavior/ motivation; and d) Practitioner efficacy.
The responses to each statement on the NIPS scale were scored on a Likert Scale where responses ranged from 1 (strongly disagree) to 5 (strongly agree). Item 6 on the practitioner-patient relationship scale: “Patients need specific instructions about how to change their behaviors” was changed to be reverse scored because the MI applied with CALC approach views the client as being fully competent to identify their own answers and solutions to challenges, and practitioners are encouraged to use probing questions rather than advice-based behavior change methods [26,37]. Item 3 on the practitioner efficacy scale: “For most patients, health education does little to promote adherence to a healthy lifestyle” was changed from being reverse scored to being scored as is, for the same reason as above.
Data analysis and interpretation
The data was plotted on graphs (see Figure 2 and Figure 3 included as supplementary) for each participant individually. Kazin [31] describes the use of visual inspection to analyze graphs for changes in measures involving a very small sample size, as demonstrating statistical significance in trends with low numbers poses a challenge. A change in mean reflects each participant’s average level of perceived competence/ autonomy/etc., and whether it changed over the baseline period and/ or after the intervention. Cohen’s statistical method for examining the degree of effect of an intervention on dependent variables was used via the rule for effect size [38]. Cohen operationally defined a small effect as d=0.2, an effect that is not noticeable to the human eye; medium effect, d=0.5 is noticeable to the unaided eye of a trained researcher or clinician; and large effect, d=0.8, is noticeable to the untrained eye such as a study participant. Cohen’s rule for interpreting effect size was used to objectively evaluate participants’ pre-post attitudes on the four sub-scales of the adapted NIPS scale and perceived competence and autonomy to facilitate behavior change among patients in routine care. For this study, it was determined that evidence of a large effect on the above outcome measures would best support the conclusions that a clinically significant change had occurred as a result of the intervention (as this would represent a change that was noticeable to the study participants).
Results
Individual effect sizes were calculated for each participant. These effect sizes were averaged to give an overall best estimate of effect. Scores for each participant were graphed and analyzed using visual inspection for the Perceived Competence Scale and the Perceived Autonomy Scale and will also be presented.
Perceived competence
The maximum score possible on the Perceived Competence Scale [32] was 35 and participants’ scores for this study ranged from 10 to 32 with higher scores indicating greater perceived competence to facilitate behavior change among patients in routine care.
Individual effect sizes for the perceived competence scale ranged from d=1.73 to 20.82 and the average of the individual effect sizes was d=4.61. This effect size indicates a clinically significant improvement in participants’ perceived competence to facilitate behavior change after completion of the training. Furthermore, visual inspection reveals an increase in each participant’s scores for perceived competence. This data is presented in Figure 2 (included as supplementary).
Perceived autonomy
The maximum score possible on the Perceived Autonomy Scale[35] was 28 and scores for this study ranged from 18 to 28 with higher scores indicating greater perceived autonomy to facilitate behavior change among patients in routine care.
Individual effect sizes for the Perceived Autonomy Scale ranged from d=0.00 to 4.08 and the average of the individual effect sizes was d=1.62. This effect size indicates a clinically significant improvement in participants’ perceived autonomy to facilitate behavior change after completion of the training. Furthermore, visual inspection reveals an increase in the majority of participants’ scores for perceived autonomy. This data is presented in Figure 3 (included as supplementary). It should be noted that the highest possible score on this scale is 28 and two participants consistently scored themselves at 28 during the baseline period, and thus there was no room to show a possible increase after the intervention period.
Adapted NIPS scale
Scale ‘Behavior change in routine care’ had a maximum possible score of 40. Participants’ scores in this study ranged from 28 to 40 with higher scores indicating more positive attitudes towards facilitating behavior change in routine care. ‘Practitioner-patient relationship’ had a maximum possible score of 40. Scores for this scale ranged from 23 to 39. Scale 3: ‘Patient behavior motivation’ had a maximum possible score of 15 and scores for this scale ranged from three to 12. ‘Practitioner efficacy’ had a maximum possible score of 30. Scores in this study ranged from 17 to 26 with higher scores indicating more positive attitudes towards the efficacy of health care practitioners to help facilitate behavior changes among patients.
NIPS effectsizes: Participants scores for ‘Practitioner efficacy’ revealed a large increase (Cohen’s d=2.22] with individual effect sizes ranging from d=0.73 to d=4.24. The overall effect for this scale was d=2.22.
Individual effect sizes for the ‘Behavior change in patient care’ scale ranged from d=-0.71 to 9.53 and the average of the individual effect sizes was d=1.69. Participants’ scores on the ‘Practitioner-patient relationship’ scale revealed a moderate increase (Cohen’s d= 0.61]. Individual effect sizes for this scale ranged from d=-1.87 to d=11.24. Effect size of scores for attitudes towards ‘Patient behavior/motivation’ revealed individual effect sizes ranging from d=-2.83 to d=1.47 with an average overall effect of d=-0.48, indicating a medium decrease. Participants’ scores for ‘Practitioner efficacy’ revealed a large increase (Cohen’s d = 2.22] with individual effect sizes ranging from d = 0.73 to d = 4.95.
The overall effect sizes for ‘Practitioner-patient relationship’ and ‘Patient behavior/motivation’ did not show clinically significant changes. The effect sizes for the ‘Practitioner efficacy scale’ and ‘Behavior change in patient care’ indicated a clinically significant improvement in participants’ attitudes towards behavior change counseling in daily clinical practice after completion of the training intervention. Individual effect sizes and averages for each scale of the adapted NIPS scale are listed in Table 2.
| Participant | Effect SizesBehaviour Change in Routine Care |
Practitioner-Patient Relationship | Patient Motivation | Practitioner Efficacy | Perceived Competence | Perceived Autonomy |
|---|---|---|---|---|---|---|
| 01 | 2.78 | 11.24 | -0.52 | 2.14 | 1.74 | 2.14 |
| 02 | 9.53 | -0.52 | -2.83 | 1.23 | 1.84 | 2.98 |
| 03 | 0.71 | -1.04 | 0.87 | 2.45 | 20.82 | 0.00 |
| 04 | 0.21 | -1.87 | -0.43 | 1.3 | 6.43 | 1.39 |
| 05 | 1.9 | -1.39 | 0.82 | 4.24 | 2.45 | 2.75 |
| 06 | -0.71 | 0.00 | 0.57 | 4.95 | 1.81 | 0.53 |
| 07 | 1.33 | -0.56 | 1.47 | 0.85 | 1.73 | 0.41 |
| 08 | 0.82 | -0.89 | -1.54 | 0.73 | 2.49 | 0.00 |
| 09 | 0.66 | -0.91 | -2.9 | 1.01 | 2.48 | 1.94 |
| 10 | -0.34 | 2.04 | 0.31 | 3.27 | 4.34 | 4.08 |
| Overall Effect | 1.69 | 0.61 | -0.48 | 2.22 | 4.61 | 1.62 |
Note:Small effect size=0.2; medium effect size= 0.5; large effect size= 0.8
Table 2: Effect Sizes for each NIPS scale, Perceived Competence Scale, and Perceived Autonomy scales for Individual Participants of the MI training.
Discussion
The objective of the present study was to determine whether participation in an seven and a half hour MI via CALC tools training workshop improved health care practitioners’ perceived competence, perceived autonomy, or attitude towards behavior change in routine care as assessed through four scales: a) Practitioner efficacy; b) Behavior change in routine care; c) Patient behavior/motivation; and d) Practitioner patient relationship. The major findings were that perceived autonomy, perceived competence, attitude toward practitioner efficacy to facilitate behavior change and attitude towards behavior change in routine care improved after participation in the training. These improvements were still clinically significant four weeks after the training workshop.
There are several important study limitations that must be considered when interpreting the results. First, given the voluntary nature of the study, the presence of selection bias is a concern. Participants who volunteer for this training may have had a high motivation to learn and implement new techniques and are not necessarily representative of all health care practitioners. Second, all measures were self-reported, thus reporting biases cannot be ruled out. Third, the small sample size reduced the power of the study and precluded the ability to examine more nuanced relationships among various subgroups of study participants (e.g., by specialty or gender). Finally, even though several clinically significant findings did emerge, and methods were employed to isolate the impact of the training itself, attributing these positive changes solely to the training intervention would be inappropriate, given that no control group was used [39].
Practice implications
These findings are important because they clearly demonstrate that practitioners are more likely to engage in behavior change conversations with patients if they feel more capable and amenable to do so, and these conversations will increase the likelihood that patients will engage in healthier choices/ behaviors. For example, in the work by Williams et al. [35], who studied both physicians and non-physicians’ predictors and motivations to counsel patients about smoking cessation, the authors reported that improvements in perceived competence and perceived autonomy predicted changes in counseling behavior [35]. Perceived autonomy is of particular significance as the self-determination theory [40] proposes that a change in perceived competence only affects motivation when the changes are experienced as autonomous [35]. Therefore, the results of this study suggest that after the MI/CALC workshop, participants felt more autonomously motivated to engage in behavior change conversations with patients and thus, may engage in this activity more often.
Successfully incorporating MI into a setting such as daily clinical practice is not well understood currently and studies report mixed results [23-25]. This may be due to the lack of understanding about how to integrate the concepts into practice [23]. Co-Active Life Coaching [26] tools can provide tangible methods to bring the tenets of MI to practical use [28] and training health care practitioners in such tools may help increase the amount and effectiveness of behavior change counseling. Up until the implementation of this study, the utility of an MI workshop using CALC tools on practitioners’ attitudes, perceived competence, and motivation to facilitate behavior change in patients had not been researched. Research evaluating MI training suggests skill gains are inconsistent and practitioners often do not achieve desired competency levels [41]. In sharp contrast, the findings from this study provide a preliminary understanding of the utility of this type of MI training that incorporates specific CALC skills to ameliorate health practitioners’ attitudes toward and perceived competency in working with their clients.
Behavior-related illnesses are a major health issue for North Americans and people around the world, and research must continue to evaluate innovative approaches to assist health care practitioners in facilitating effective behavior change counseling. Despite the limitations of this study, MI applied via CALC tools training shows promise as a strategy to improve health care practitioners’ incentive to address behavior change in daily clinical practice. Future research should focus on a larger scale study and include more objective measures of practitioner counseling behavior.
References
- Are integrated approaches working to promote healthy weights and prevent obesity and chronic disease? Health Canada. 2004.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States. JAMA 291: 1238-1245.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2005) Correction: Actual causes of death in the United States. JAMA 293: 293-294.
- Statistics Canada. Going to the doctor. Health reports. Health Statistics Division.2007.
- Ma J, Urizar GG, Alehegn T, Stafford RS (2004) Diet and physical activity counseling during ambulatory care visits in the United States. Prev Med 39: 815-822.
- Thorndike AN, Regan S, Rigotti NA (2003) The treatment of smoking by US physicians during ambulatory visits: 1994. American Journal of Public Health 97: 1878-1883.
- Scott JG, Cohen D, DiCicco BB, Orzano AJ, Gregory P et al. (2004) Speaking of weight: How patients and primary care clinicians initiate weight loss counselling. Prev Med 38: 819-827.
- Ohtaki S, Ohtaki T, Fetters MD (2003) Doctor-patient communication: A comparison of the USA and Japan. J FamPract 20: 276-282.
- Stange KC, Zyzanski SJ, Jaén CR, Callahan EJ, Kelly RB et al. (1998) Illuminating the ‘black box’: A description of 4454 patient visits to 138 family physicians. J Fam Pract 46: 377-389.
- Haddock J, Burrows C (1997) The role of the nurse in health promotion: An evaluation of a smoking cessation programme in surgical pre-admission clinics. J AdvNurs 26: 1098-1110.
- Arnet I, Hersberger KE (2010) Improvement of compliance supported by pharmacists. [Verbesserungen der Compliance durch die Apotheke] TherapeutischeUmschau 67: 293-301.
- National Physician Survey (2010) Fast facts, family physicians and nutrition counselling. Can Fam Phys 56: e93.
- Grumbach K, Coffman J (1998) Physicians and nonphysician clinicians: Complements or competitors? J Am Med Assoc 280: 825-826.
- Pottie K, Farrell B, Haydt S, Dolovich L, Sellors C, et al. (2008) Integrating pharmacists into family practice teams: Physicians’ perspectives on collaborative care. Canadian Family Physician 54: 1714-1715.
- Sommers LS, Marton KI, Barbaccia JC, Randolph J (2000) Physician, nurse, and social worker collaboration in primary care for chronically ill seniors. Arch Intern Med 160: 1825-1833.
- Miller WR (1983) Motivational interviewing with problem drinkers. Behav Cogn Psych other 11: 147-172.
- Brug J, Spikmans F, Aartsen C, Breedveld B, Bes R etal. (2007) Training dietitians in basic motivational interviewing skills results in changes in their counselling style and in lower saturated fat intakes in their patients. J Nutr Educ Behav 39: 8-12.
- DiIorio C, McCarty F, Resnicow K, Holstad MM, Soet J, et al. (2008) Using motivational interviewing to promote adherence to antiretroviral medications: A randomized controlled study. AIDS Care 20: 273-283.
- Scales R, Miller JH (2003) Motivational techniques for improving compliance with an exercise program: Skills for primary care clinicians. Curr Sports Med Rep 2: 166-172.
- Burke BL, Arkowitz H, Menchola M (2003) The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J Consult ClinPsychol 71: 843-861.
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL (2010) A metaanalysis of motivational interviewing: Twenty-five years of empirical studies. Res Soc Work Pract 20: 137-160.
- Rubak S, Sandbaek A, Lauritzen T, Christensen B (2005) Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract 55: 305- 312.
- Mesters I (2009) Motivational interviewing: Hype or hope? Chronic Illn 5: 3-6.
- HettemaJ, Steele J, Miller WR (2005) Motivational interviewing. Annu Rev Clin Psychol 1: 91-111.
- Hettema JE, Sorensen JL, Uy M, Jain S (2009) Motivational enhancement therapy to increase resident physician engagement in substance abuse education. Subst Abuse 30: 244-247.
- Whitworth L, Kimsey HK, Kimsey HH, Sandahl P (2007) Co-active coaching: new skills for coaching people toward success in work and life. 2nd ed. California: Davies-Black Publishing.
- Irwin JD, Morrow D (2005) Health promotion theory in practice: An analysis of co-active coaching. Int Journ of Evid-Based Coach and Ment 3: 29-38.
- Newnham KC, Morrow D, Irwin JD (2010) Motivational coaching: A functional juxtaposition of three methods for health behaviour change: Motivational interviewing, coaching, and skilled helping. Int Journ of Evid-Based Coach and Ment. 8: 27-48.
- Wiley E, Irwin JD, Morrow D, Health Care Practitioners’ Perceptions of a One- Day Applied Training in Motivational Interviewing for Facilitating Behaviour Change. Under review.
- Hayes SC (1981) Single case experimental design and empirical clinical practice. J Consult Clin Psych 49: 193-211.
- KazdinAE (1982) Single-case research designs: Methods for clinical and applied settings. New York: Oxford University Press.
- Williams GC, Deci EL (1996) Internalization of biopsychosocialvalues by medical students: A test of self-determination theory. J Pers Soc Psychol 70: 767-779.
- Williams GC, Deci EL (1998) The importance of supporting autonomy in medical education. Ann Intern Med 129: 303-308.
- Williams GC, Freedman ZR, Deci EL (1998) Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 21: 1644-1651.
- Williams GC, Levesque C, Zeldman A, Wright S, Deci EL, (2003) Health care practitioners’ motivation for tobacco-dependence counseling. Health Educ Res 8: 538-553.
- McGaghie WC, Van HL, Fitzgibbon M, Telser A, Thompson JA, et al. (2001) Development of a measure of attitude toward nutrition in patient care. AmJ Prev Med 20: 15-20.
- Miller WR, RollnickS (2002) Motivational interviewing, preparing people to change addictive behaviour. New York: The Guildford Press.
- Cohen J (1988) Statistical power analysis for the behavioral sciences (2nd ed.). New Jersey: Hillsdale.
- Shadish WR, Cook TD, Campbell DT (2002) Experimental and quasiexperimental designs for generalized causal inference. Boston: Houghton Mifflin.
- Deci EL, Ryan RM (1985) Intrinsic motivation and self-determination in human behavior. New York: Plenum.
- Catley D, Harris KJ, Mayo MS, Hall S, Okuyemi KS, et al. (2006) Adherence to principles of motivational interviewing and client within-session behavior. BehavCognPsychother 34: 43-56.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 14847
- [From(publication date):
November-2011 - Nov 23, 2024] - Breakdown by view type
- HTML page views : 10466
- PDF downloads : 4381