Review Article Open Access
The Immune System in the Pathogenesis and Prevention of Prion Diseases
Annissa Furr1,2, Alan J Young1,2* and Jurgen Richt3
1Department of Veterinary and Biomedical Sciences, South Dakota State University
2Medgene Labs LLC, Brookings, SD
3Department of Diagnostic Medicine/Pathobiology, Kansas State University, Manhattan, KS
- *Corresponding Author:
- Dr. Alan J. Young
Department of Veterinary and Biomedical Sciences
South Dakota State University
Brookings, SD. 57006, USA
Tel: 605-688-5982
Fax: 605-688-6003
Email: alan.young@sdstate.edu
Received Date: August 31, 2011; Accepted Date: January 27, 2012; Published Date: February 16, 2012
Citation: Furr A, Young AJ, Richt J (2012) The Immune System in the Pathogenesis and Prevention of Prion Diseases. J Bioterr Biodef S1:012. doi: 10.4172/2157-2526.S1-012
Copyright: © 2012 Furr A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Bovine spongiform encephalopathy (BSE) remains a significant threat to both human and animal health in the United States and in particular a threat to the agriculture industry. The diagnosis of BSE in a single cow within the United States in 2003 led to net losses of billions of dollars and additional studies have pointed to significant sociological consequences of BSE cases in Canada, particularly in terms of the dissolution of rural communities. Unlike other infectious diseases, BSE and other prion diseases are caused by a misfolded protein (PrPSc) that is highly resistant to normal nucleic acid-based disinfection and sterilization procedures. Disease progression is linked to the progressive conversion of a normal cellular molecule (PrPC) into the infectious form (PrPSc) mainly on cells of the immune and neurological systems, leading to formation of multimolecular fibrils associated with progressive neurodegeneration and dementia. Due to the unique nature of this infectious particle and the fact that the disease is caused by a misfolded form of a normal self-protein, development of vaccines and other therapeutics have been challenging. The molecular
mechanisms behind PrPSc targeting to lymph node germinal centers and the failure of immune recognition, remain unclear. Here, we review the current knowledge of prion disease biology, the role of the immune system in disease transmission and pathogenesis and efforts towards development of therapeutics and vaccines. While feed-based control of BSE has been successful in limiting transmission and spread of the disease, the recent description of apparently spontaneous and/or genetic forms of BSE underlies the importance of continued research into tools to counter this unique disease threat to the world economy as well as animal and human health.
Introduction
Bovine spongiform encephalopathy (BSE) is an ongoing threat to the cattle industry worldwide and is also of concern from a biodefense perspective because its causative agent, the infectious prion, is characterized both as a USDA-designated select agent and as a potential object for agroterrorism. The primary focus of prion diseases as a threat to the security of the United States should be the proven economic consequences of the identification of BSE-positive animals and animal products and its significant consequences for the US beef export market. It has been estimated that the 2003 case of BSE in the United States resulted in a net loss to the export market of between $3.2 and $4.7 billion, in addition to the ongoing sociological burden to the rural economy that continues to affect agricultural and associated industries [1,2]. The economic consequences of BSE are further exacerbated by the realization that the BSE agent, unlike other transmissible spongiform encephalopathy (TSE) agents, appears to transmit across species barriers and has resulted in a novel human prion disease, called variant Creutzfeldt-Jacob disease (vCJD), in at least 200 individuals to date [3]. TSEs of sheep (scrapie) had been recognized for more than 200 years when BSE was first recognized in the British cattle herd in 1986 [4]. The origin of the original case(s) of BSE remains an enigma, although several potential causes have been suggested. Hypotheses include (i) the inclusion of sheep- or goatderived scrapie agent-infected tissues in meat and bone meal fed to cattle [5], (ii) a previously undetected sporadic or genetic bovine TSE contaminating cattle feed [6], or (iii) origination from a human TSE through animal feed contaminated with human remains [7]. It is generally accepted that the practice of feeding meat and bone meal from affected animals back to the cattle amplified the disease in the European dairy and beef herds, and implementation of an outright ban on this process has significantly limited further occurrence of the disease. It was estimated that approximately 750,000 animals infected with the BSE agent were slaughtered and consumed by humans in Europe (mainly UK) between 1980 and 1996 [4]. Since that time, it has become largely accepted that BSE is caused by a promiscuous strain of prion pathogen that effectively crosses species barriers and affects both humans and multiple animal species and as a consequence over 200 cases of variant CJD (vCJD) and one case of goat BSE have been identified [3-8]. North America identified its first BSE case in May 2003 in a Canadian-born cow in Alberta, and in December 2003 the first American BSE case was diagnosed [9,10]. Although this animal was later identified as a Canadian import, the identification of two additional indigenous cases in 2005 and 2006 (82,84) clearly established the presence of BSE within the United States, albeit at significantly lower rates than those measured in most parts of Europe. Molecular characterization of these cases indicated three specific etiologies for BSE similar to human TSEs: infectious, genetic and sporadic [10,11]. Regardless of the cause, the severe economic consequences of BSE and its zoonotic potential were the most important aspects of implementing mitigation strategies, with an estimated cost to the US Cattle Markets of $3.2-4.7 billion, most of which was due to losses in the export market [1].
Overview of TSE History and Pathogenesis
Naturally occurring transmissible spongiform encephalopathies (TSEs) have been found in numerous mammalian species including deer and elk (chronic wasting disease, CWD), sheep and goats (scrapie), cattle (bovine spongiform encephalopathy, BSE), mink (transmissible mink encephalopathy, TME) and humans. TSEs of humans include sporadic, genetic and infectious forms of Creutzfeldt-Jakob disease, Kuru, Gerstmann-Sträussler-Scheinker syndrome and familial fatal insomnia. Of these diseases, only BSE agents appear capable of extensively crossing species barriers and are believed to be the cause of vCJD. As a group, these unique diseases pose a considerable health threat to humans and animals and impose a significant financial burden on the agricultural industry. Billions of dollars are lost each year due to trade restrictions, disease surveillance and herd destruction, which could be at least partially ameliorated by a sensitive antemortem test or effective vaccine strategies. Due to its unique nature, however, definitive ante mortem diagnostic tests and development of immune-based counter-therapies have been elusive.
The oldest of the TSEs or prion diseases is scrapie in sheep, which has been known since the middle of the 18th century [12]. It is believed that scrapie, like all TSEs, is caused by ingestion of material containing the altered form, PrPSc, of the normal cellular protein PrPC. Clinical signs of TSEs include degenerative neurological problems, weight loss and marked changes in personality or behavior. In most prion diseases, incubation periods are measured in years, accounting for their early designation as “slow viral diseases” [12].
The normal cellular protein PrPC is a glycosylphosphatidylinositolanchored plasma membrane protein that is highly conserved and encoded by a single copy host gene (Prnp) [13]. PrPCis found on nearly every cell in the body but is highly expressed by neuronal cells and most cells of the immune system. The molecular function of this ubiquitous cellular protein is not yet clear, but its importance in several cellular processes has been identified. As a result of these studies, PrPC appears to be a pleiotropic protein involved in cellular trafficking, copper uptake, protection against oxidative stress, cell adhesion and differentiation, as well as cell signaling and protection against apoptotic activity [14-16]. Clearly, many of these functions are of importance to the immune system, although identification of specific immunological defects in Prnpknockout mice and cattle have not been reported [17,18]. In addition, PrPC appears to have some basic physiological significance based on the fact that it is expressed and rather highly conserved in many species including humans, hamsters, rats, mice, cattle, sheep, goats and chickens [19]. However, it has been reported that mice engineered to lack the gene encoding PrPC exhibit no developmental or behavioral problems except a higher susceptibility to seizures and no significant defects have been observed in prion-knockout cattle [17,20,21].
According to the “protein-only hypothesis”, prions are the causative agent of all TSEs including scrapie in sheep and CWD in deer and elk. Prions are infectious, structurally altered isoforms of the normal cellular proteins that are partially resistant to proteolytic degradation [14,22-24]. PrPSc and PrPC are identical in their primary protein structure; therefore, changes in their secondary structure account for the structural and physiological differences between the two proteins. PrPC is primarily alpha-helical in conformation with very few betasheets, while PrPSc is comprised of significantly fewer alpha-helices but is rich in beta-sheets, although this structure remains to be confirmed by x-ray crystallographic techniques. The mechanism by which PrPC is converted to PrPSc remains elusive, but research indicates that the conversion occurs either on the cell surface, or intracellularly after PrPC has been internalized for degradation [24]. PrPC is therefore converted post-translationally to PrPSc. Once formed, the infectious PrPSc forms multimeric amyloid plaques as it accumulates, causing characteristic and identifiable accumulations within germinal centers of lymph nodes and affected central nervous system tissue. Within the CNS, this results in progressive cell death and the spongiform plaques identified in the brains of infected humans and animals [13,25]. The conversion of PrPC into PrPSc is an autocatalytic process and newly formed PrPSc can then propagate the conversion of more PrPC. In support of this, an in vitro amplification technique known as protein misfolding cyclic amplification (PMCA) has been used with great success in prion research and is the basis for numerous studies designed to identify small but infectious doses of PrPSc in test material. PMCA, which is analogous to PCR in principle, can cause the generation of PrPSc from PrPC by using small amounts of PrPSc infectious protein as seed to catalyze the conversion of native or recombinant PrPC in vitro [26]. Additional studies have confirmed that this newly-amplified PrPSc is in fact infectious in rodent models, although quantitative measurement of prions from other species has been more complex [27]. To date, therefore, mapping of disease pathogenesis has largely relied upon immunohistochemical detection of prion fibrils and biochemical detection of PrPSc.
Transmission of TSEs
Species specificity of TSEs
Although Prnp, the gene that encodes the normal cellular protein PrPC, is highly conserved among species, TSE agents themselves are highly species-restricted. With the exception of the BSE agent, which appears highly capable of crossing species barriers, all other TSE agents tend to be restricted to closely-related species (Table 1). These natural species barriers may be overcome by experimental inoculation, but the mode of infection is generally not one that occurs in nature and the inoculating dose is usually substantially higher than would be expected in nature [28]. Following intraspecies experimental transmission, the incubation period of disease is normally significantly longer than in the natural host, although successive passages through the new species can to some extent ameliorate this [29]. Although not a natural host for prion diseases, murine models of TSEs have been developed either by adapting natural scrapie or TME agents to rodent models, or by engineering mice that express Prnp from sheep, deer, humans, and cattle [30]. These models have been extremely useful in examining the species restriction of prion diseases and development of bioassay systems for infected material from natural hosts. Furthermore, these experiments clearly indicate that transmission of disease depends upon matching the sequence of host PrPC to the original species from which the PrPSc originated [31]. This relationship has been further confirmed using the in vitro PMCA assay [32].
| TSE | Natural Hosts Reported | Human Health Risk |
|---|---|---|
| Scrapie | Sheep, Goats | None Reported |
| Bovine Spongiform Encephalopathy (BSE) | Cattle, transmits readily across species barriers | High – Consumption of affected material |
| Chronic Wasting Disease (CWD) | Wild and Farmed Deer, Elk, Moose | None Reported |
| Transmissible Mink Encephalopathy (TME) | Farmed Mink | None Reported |
| Variant CreutzfeldJakob Disease (vCJD) | Human (derived from BSE) | High – transmission via blood products, Nosocomial, Consumption of BSE-contaminated food products |
| Creutzfeld-Jakob Disease | Humans | Sporadic, Genetic, Iatrogenic. High-transmission by exposure to contaminated brain material, Nosocomial. |
| Kuru | Human | Transmitted by ritualistic cannibalism |
| Fatal Familial Insomnia | Human | Autosomal Dominant,Pathogenic mutation with high penetrance |
| Gerstmann-Straussler- Sheinker disease | Human | Autosomal Dominant,Pathogenic mutation with high penetrance |
Table 1: Known Transmissible Spongiform Encephalopathies and their Natural Hosts.
Genetic susceptibility to infectious TSEs: Scrapie and Chronic Wasting Disease
Genetic susceptibility to prion disease varies depending on target species. Isolation of specific polymorphisms affecting overall susceptibility of wild deer species has been difficult, however recent data may indicate that genotype can affect incubation times of experimental disease [33-36]. Other species, including sheep and elk, appear to have a possible genetic resistance or enhanced susceptibility to prion disease depending on very specific polymorphisms within the Prnp gene [37]. In sheep, amino acid substitutions at three specific codons appear to be most influential for determining susceptibility or resistance to disease progression. These three codons are: alanine (A) or valine (V) at codon 136, arginine (R) or histidine (H) at codon 154, and glutamine (Q) or arginine (R) at codon 171. Animals with the genotype of ARR are most resistant to infection with the scrapie agent, while animals with the genotype VRQ are most susceptible to disease [38]. In elk, one epidemiological study suggested that animals with a leucine at codon 132 may be resistant to infection with the CWD agent, whereas those with methionine are susceptible [29], although this could not be confirmed in experimentally infectedelk [39]. The codon 132 polymorphism is particularly intriguing, given that all patients suffering from vCJD to date are homozygous for methionine at the analogous codon 129 of the human Prnp gene [40,41]. The reason for this genetic resistance or enhanced susceptibility has yet to be explained, but may relate to either the conformation or expression level of native PrPC in these individuals. Susceptible sheep have a higher percentage of cells expressing PrPC on their surface than resistant animals. Furthermore, resistant sheep have a higher percentage of CD4+ and CD8+ cell populations following infection with the scrapie agent [42]. These differences may explain, at least in part, the genetic resistance to disease.
Lymphoid Pathogenesis of TSEss
Involvement of immune cell subsets in prion disease
Current research in prion immunology has suggested the possible involvement of multiple cell types of the lymphoreticular system (LRS) during disease progression. Interestingly, almost all cells of the LRS express high levels of PrPCon their surface, which may be a reason why they are involved in the early stages of the disease [43,44]. Prion accumulation has also been found within granulomas of transgenic mice infected with prions [43], in lymphoid follicles of kidneys in white-tailed deer infected with the CWD agent [45], and has been identified at low levels within the muscle of mule deer infected with the CWD agent and in the muscle tissue of hamsters infected with the TME agent, potentially associated with local inflammation in those tissues [46,47]. This clearly implicates a role for the immune system as a potential target, if not responder, to the prion agent.
Mechanism of Prion Targeting to Lymph Nodes
General considerations
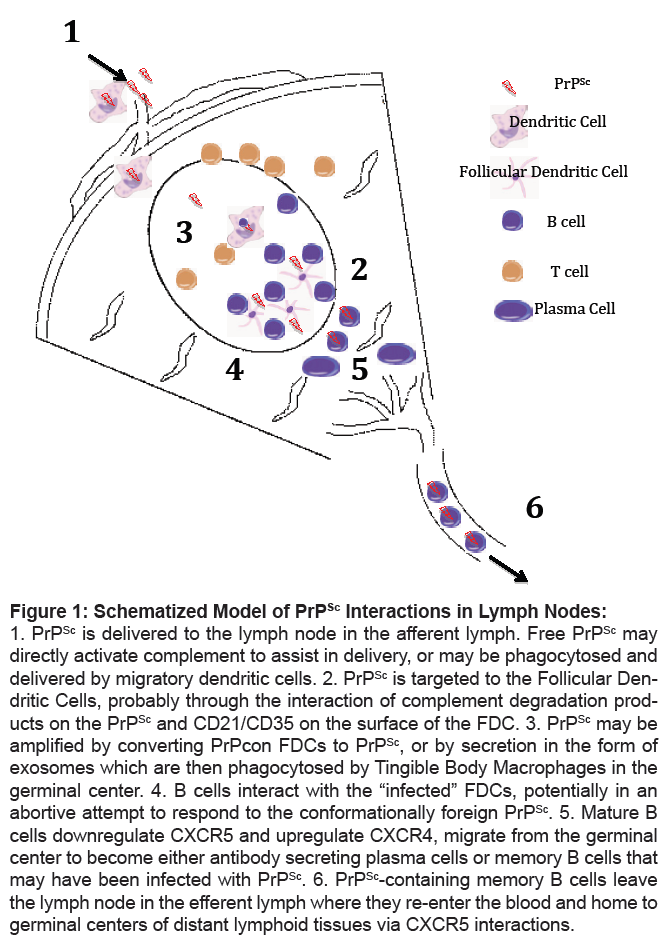
In many ways, targeting of PrPSc to germinal centers appears similar to antigen delivery and deposition within lymph nodes during normal immune responses. Although the current understanding of the function and mechanisms involved in antigen delivery and initiation of T and B cell responses has been reviewed elsewhere, a brief discussion of the normal process ofantigenic recognition and B cell stimulation is warranted in order to discuss similarities and differences associated with prion infection [48-50]. Following introduction into the nonlymphoid tissues of the body, antigen may be delivered to the regional lymph node in one of two mechanisms. Large, insoluble antigens appear to be engulfed by resident dendritic cells, which then actively enter the afferent lymphatics and travel to the draining lymph node. In contrast, small, soluble antigens appear to passively enter the lymph fluid and are then delivered to the outer boundary of the germinal center by virtue of normal lymph flow [51]. There is now evidence to suggest that B cells actively shuttle these antigens to the follicular dendritic cells (FDCs), non-hematopoietic cells found within the germinal center. These antigens are then believed to bind to the surface of FDCs by virtue of Fc or complement receptors, where they are passively “presented” to B cells for activation. Activated B cells can then be stimulated by these immobilized antigen complexes, and receive costimulation from follicular T cells or the FDCs themselves. FDCs possess several characteristics which further regulate B cell differentiation and activation, including cell-surface TLR4 and the chemokine CXCL13 (BLC) which recruits CXCR5 positive B cells to the germinal center [50- 52]. Following stimulation, B cells may differentiate into plasma cells, which actively secrete antibody, or memory B cells, in a mechanism which is not entirely understood. Associated with this differentiation, B cells downregulate expression of CXCR5, and upregulate CXCR4 which promotes their migration towards the dark zone and differentiation to plasma cells [50]. Although the majority of plasma cells migrate to the medulla of the lymph node to secrete antibody, memory B cells and so-called “lymphoblasts” leave the lymph node in the efferent lymph, ultimately migrating to other tissues of the body via the blood (Figure 1).
Figure 1: Schematized Model of PrPSc Interactions in Lymph Nodes:
1. PrPSc is delivered to the lymph node in the afferent lymph. Free PrPSc may
directly activate complement to assist in delivery, or may be phagocytosed and
delivered by migratory dendritic cells. 2. PrPSc is targeted to the Follicular Dendritic
Cells, probably through the interaction of complement degradation products
on the PrPSc and CD21/CD35 on the surface of the FDC. 3. PrPSc may be
amplified by converting PrPcon FDCs to PrPSc, or by secretion in the form of
exosomes which are then phagocytosed by Tingible Body Macrophages in the
germinal center. 4. B cells interact with the “infected” FDCs, potentially in an
abortive attempt to respond to the conformationally foreign PrPSc. 5. Mature B
cells downregulate CXCR5 and upregulate CXCR4, migrate from the germinal
center to become either antibody secreting plasma cells or memory B cells that
may have been infected with PrPSc. 6. PrPSc-containing memory B cells leave
the lymph node in the efferent lymph where they re-enter the blood and home to
germinal centers of distant lymphoid tissues via CXCR5 interactions.
It is interesting to note that the early germinal center response to both T-dependent antigens and T-independent antigens is similar. However, while FDCs may provide important costimulatory signals to B cells in the absence of T cell help, T-independent responses tend to be far shorter than T-dependent responses, with germinal centers beginning to involute within 5 days of stimulation [49]. In the absence of antigen presentation to T cells and resulting T-helper cell responses, therefore, B cell differentiation and response is significantly abrogated, although still present and tends to result in production of low affinity IgM antibody. It is intriguing that the localization of the prion agent in lymphoid tissues following infection appears to parallel many of these mechanisms closely.
Mechanisms of PrPSc Delivery to Lymph Nodes
Antigen trafficking into the germinal center remains somewhat unclear, but recent studies using two-photon microscopy have allowed some insights into these events. Antigens that form immune complexes are retained on the surface of FDCs within germinal centers through specific receptors [48]. FDCs bind immune complexes via complement receptors CD21/CD35 that bind proteolytic components of C3 and C4. These captured immune complexes are then held in the germinal center to allow migrating immune cells to come in contact with and react to the antigens. Research using two-photon microscopy has shown that subcapsular macrophages and B cells are responsible for trafficking the immune complexes from the point of infection to the germinal center [53]. It is possible that prions, being larger than typical antigens, follow a pattern similar to immune complexes as they travel into the germinal center. Accumulation of prions is intensified throughout infection, suggesting that the LRS might be a continuous trafficking medium of prions throughout the course of infection. In addition, the LRS could also be a site of replication of the infectious agent. Upon examination of lymph nodes in varying stages of disease, it is obvious that in a susceptible, infected animal there is a steady increase in the amount of PrPSc as the disease progresses (unpublished observations). Assuming that the animal is not continually exposed to the infectious agent in the environment, it can be assumed that the increase in infectious material is achieved by conversion of host PrPC to PrPSc during disease incubation.
Targeting of Soluble PrPSc to Germinal Centers
Complement, a collection of plasma proteins that make up part of the innate immune system, has the ability to bind to antigen and, through a catalytic amplification loop, activate cells of the immune system. Activation of each active component is accomplished by cleavage of an inactive precursor into an active form capable of activating the next component in the pathway and a cleavage product that may have additional bioactivity. Complement can be activated via the classical pathway, the alternative pathway, or the lectin pathway. Both the classical and alternative pathways have been associated with prion disease [54]. PrPSc has been demonstrated to directly activate complement component C1 in the absence of specific antibody, thereby initiating the classical complement pathway. Ultimately, this results in cleavage of the C3 component, presumably depositing C3b, C3d, and C4d complement components on the surface of the scrapie fibrils. FDCs trap and retain antigen through expressed complement receptors on their surface. Complement receptors CD21 and CD35 bind the complement proteolytic fragments C3b, iC3b, C3d and C4b [53,55]. Both CD21 and CD35 are critical in normal antigen targeting to FDCs and germinal centers [48]. Antigen complexes or PrPSc are then “presented” to B cells through the interaction of surface antibody on B cells and specific receptors on the surface of FDCs, supported by co-receptors CD21 and CD40. Together, surface adsorbed antigen and these co-receptors activate antigen-specific B cells in germinal centers and initiate both T-dependent and T-independent antibody responses to antigen [49]. Clearly, these processes are at least partially interrupted in prion-infected germinal centers, as there is no evidence for significant production of PrPSc-specific antibody, although recent reports suggest low-affinity PrP-specific antibody can be produced late in the disease process in mouse models [56]. Nonetheless, the targeting and accumulation of PrPSc on FDCs appears independent of antibody, and is likely at least partially dependent on complement activation [57]. Mice genetically deficient in antibody production can be infected with PrPSc with no observable differences in incubation time or production of PrPSc infectivity [57]. In contrast, mice that lack CD21/CD35 receptors demonstrate significantly prolonged incubation periods as compared to wild type susceptible mice [58]. Inactivation or elimination of C1q renders mice resistant to prion infection [57,59]. Cobra venom factor (CVF) non-specifically depletes the complement system of mice for up to 5 days. When mice are treated once with CVF and then immediately infected with the scrapie agent, these mice survive the CVF-untreated infected mice by at least 2 months [60]. This further indicates a significant involvement of the complement pathway in the early establishment of infection. In addition, these data imply that early trafficking to the LRS is vital for successful establishment of the disease: even though the alternative complement system is restored after 5 days, the mice retain substantial protection from infection [57].
Cell-Borne Delivery to Germinal Centers
It is generally accepted that initial prion entry in the intestine is mediated by direct uptake from the intestinal lumen by M-cells [61-65]. Following uptake, delivery and dissemination of the prion molecule is less clear, but there is significant evidence for a role for dendritic cell (DC) subsets in transport [66,67]. DCs have the ability to ingest antigen and retain the antigen for extended periods of time, and are believed to play a role in the normal transport of antigen between the tissues and lymph nodes [50,51]. Following infection of the gut, PrPSc-positive DCs can be detected in the intestinal lymph, presumably in transit to the regional lymph nodes [66]. In addition, tingible body macrophages in lymph nodes show infectivity and contain PrPSc at early and late stages of infection, and while generally not believed to be migratory they remain potential candidates for harboring or disseminating infection throughout the lymphoid system [68]. Macrophages carrying PrPSc have been identified in the lymph nodes of infected animals, and appear to act as the primary transport mechanism in animals that have been depleted of FDCs [55]. It therefore seems likely that the earliest stages of prion infection of the lymphoid system involve a normal antigeninduced process designed to clear foreign infections from the host, and that the conversion from antigen to pathogen occurs following delivery to the germinal center.
Amplification of Prions within Germinal Centers
Shortly after PrPSc delivery to the germinal center, the infectious protein accumulates within the light zone, similar to other antigens (Figure 1) [69]. Specifically, the PrPSc is targeted to follicular dendritic cells (FDCs) within the germinal centers that remain positive by immunohistochemistry throughout infection [70]. FDCs are longlived, non-dividing cells of epithelial origin that can retain antigen complexes on their surface for extended periods [71,72]. Although their precise origin remains unknown, it is clear that they are absolutely required for peripheral amplification of PrPSc during infection [18,73]. Murine models have further demonstrated a role for FDCs as the central cell type within lymph nodes for prion pathogenesis by treating mice with gamma-irradiation either before or after infection with PrPSc, a treatment that shows no effect on the establishment of prion disease [74]. Due to the fact that FDCs and neurons are mitotically inactive and therefore survive gamma-irradiation, while T cells, B cells and monocytes are susceptible, these studies demonstrated that FDCs and neuronal cells but not circulating lymphocytes are vital in the pathogenesis of prion disease [54]. Within the germinal center, FDCs constitutively express high levels of PrPC, which presumably functions as a template for PrPSc replication, which results in the deposition of scrapie fibrils [73]. In cattle, there is no detectable amplification or deposition of prion protein in lymph node germinal centers following infection. It is interesting to note that cattle FDCs, unlike those of other species, express an antigenically unique isoform of PrPC different from that observed in neuronal cells, potentially explaining the absence of peripheral replication of the prion agent in cattle [75]. Although pathological changes in lymphoid tissues infected with PrPSc have been difficult to define, one study observed abnormal FDC maturation cycles in the mesenteric lymph nodes of mice infected with the scrapie agent [76]. In general, these alterations limited the ability of FDCs to downregulate PrPC and resulted in increased immune complex and PrPSc deposition. Together, these data suggest a central role for FDCs in prion amplification during disease incubation.
In addition to FDCs, tingible body macrophages within lymph nodes have also been identified as containing PrPSc [68]. These cells normally phagocytose dead and dying B cells within germinal centers, but may also play a central role in the clearance of PrPSc from affected tissues [77]. Macrophages are able to phagocytose small, PrPSc containing vesicles produced by infected FDCs, and elimination of macrophages from prion-infected mice results in significant enhancement in the level of PrPSc within tissues [78]. Interestingly, while resting macrophages can effectively phagocytose and clear PrPSc, activation of macrophages appears to decrease the ability of these cells to phagocytose and degrade the infectious material [79]. Furthermore, activated macrophages appear to increase PrPC expression, potentially providing additional template PrPC for agent amplification. Ultimately, this could lead to accelerated PrPSc replication during immune responses. Interestingly, the presence of bacterial colitis has recently been shown to increase susceptibility to oral prion infection [80]. It is important to note, however, that several studies appear to directly refute this conclusion. Specifically, activation of innate immunity through administration of Freund’s Complete adjuvant significantly prolongs prion disease in mouse models, and interfering with innate immunity through targeted activation of TLR-9 or knockout of TLR-4 accelerates the disease process [81,82]. Therefore, the effect of systemic immune activation in disease pathogenesis remains unclear.
Systemic Dissemination through the Lymphoreticular System
During the asymptomatic period of TSE prion pathogenesis there is significant peripheral spread of PrPSc throughout the lymphoid system. Although it is possible that free PrPSc may effectively enter the efferent lymph, and eventually the blood, causing prionemia, a more likely explanation is the infection and dissemination of recirculating lymphocytes. A number of studies have clearly demonstrated that the infectious agent could be transmitted between susceptible sheep or deer by blood transfusion [83-86]. In rodents, in vitro detection of PrPSc associated with buffy coat leukocytes has illustrated the importance of circulating leukocytes in agent dissemination [87,88]. More recently, several studies have directly implicated blood-borne B cells as the source of this infectivity [83,89]. The mechanism whereby B cells become infected and potentially transmit PrPSc to distant lymph nodes remains unclear; however, it seems likely that it is acquired directly from PrPScinfected FDCs in germinal centers. Whether this acquisition of PrPSc is part of a normal immunological process, or incidental as a result of PrPC expression by B cells, remains to be investigated. It is interesting to note that CXCR4 expression is increased associated with normal B cell maturation within lymph nodes, and that CXCR4 ligation by CXCL13 on murine olfactory cells has been reported to increase PrPC expression [50,90]. Regardless of the mechanism, it seems likely that migratory B cells may be a major factor in the dissemination of PrPSc throughout the lymphoid system of affected animals.
Immune Response to Prions
There does not appear to be a significant protective immune response to PrPSc infection, presumably due to the fact that the primary sequence of PrPSc is identical to PrPC and hence subject to self-tolerance [91]. Since both T and B cells are selected during development to ignore self-antigens in order to develop self-tolerance, one would not expect it to react to an antigen with the same amino acid sequence asPrPC, a normal cellular protein. This concept is supported by the fact that production of PrP-specific antibody and sensitized T cells can only be accomplished effectively in Prnp-knockout mice [92,93]. Recently, low-affinity IgM antibodies specific for PrP have been reported in experimental mice following clinical signs associated with scrapie, suggesting that long-term infection may result in a T-independent response to PrPSc [56]. Despite tolerance, there is substantial lymphoreticular system (LRS) involvement in prion disease. The LRS, primarily the lymph nodes, is a source of accumulation and possible propagation of PrPSc well before the agent is established in the brain, and therefore the circulating immune system remains a primary target for development of ante mortem diagnostic assays [69,94]. Prions accumulate quickly in the lymph nodes and remain there throughout the extended asymptomatic period, whereas they only accumulate in the brain in the later stages of the disease. Incubation periods vary greatly based on species. Incubation times for experimental sheep scrapie are normally 1-2 years, while humans can incubate prion disease in excess of 50 years before showing any clinical signs [31,95]. Therefore, it may eventually be possible to treat prion diseases after infection but before PrPSc accumulation has been established in the brain. As long as accumulation in the brain is inhibited, the host appears to suffer no ill effects from the disease [95].
Immune-Based Approaches to Prion Disease Therapy
Effective prevention and treatment of prion diseases is focused on two major areas: Preexposure prevention, and post-exposure prophylaxis. To date, attempts to prevent prion disease through vaccination of normal individuals has been limited, whereas progress has been made in distinct therapeutic approaches to limit prion fibril replication following infection.
There is no measurable immune response against prions during normal disease progression [96], however, a number of studies have focused on the development of appropriate immunization strategies to develop immunity to PrPC, PrPSc, or both [96]. Attempts to develop vaccination strategies in murine models have been hindered by (i) selftolerance to the primary structure of the PrP molecule (ii) potential autoimmune responses to self- PrPC induced by vaccination and (iii) inability to provide protection to cerebral tissues due to immunological preference of the brain, and impermeability of the blood-brain barrier [96]. Similar difficulties have been illustrated in studies designed to uncover effective vaccination strategies for Alzheimer’s disease. Nonetheless, studies have demonstrated the effectiveness of anti-PrP antibodies in blocking both infection and disease progression in vitro. Specifically, anti-PrP antibodies directed against distinct PrP epitopes have been shown to inhibit prion replication in affected cell lines [97- 99]. In later work, one of these antibodies was engineered as a singlechain antibody (scFv) fragment to allow greater tissue penetration, and was found to retain its ability to inhibit PrPSc conversion in vitro [100]. In an attempt to provide direct, local production of inhibitory antibodies at the site of replication, an adeno-associated virus type 2 was used deliver cDNA of several anti-PrP scFv antibodies in a mouse model of prion infection. While there was apparently little correlation between the affinity of individual scFv fragments for PrPC and their ability to inhibit disease, several constructs did effectively lengthen survival of experimental mice [101].
Additional studies in animal models were also shown to have some success. Mice rendered transgenic for the heavy chain of the 6H4 anti-PrP monoclonal antibody were resistant to prion infection, and both direct immunization of wild-type mice with recombinant PrPC or passive vaccination with PrP-specific antisera delayed disease onset [102-104]. Significantly higher doses of passive antibody were shown to block disease, even when provided to infected mice up to one month after exposure to PrPSc-containing material [105]. This may then represent a potential therapeutic strategy when the date of exposure is known, but is less likely to prove a useful therapy in most clinical or agricultural situations. Passive vaccination is ineffective following development of clinical signs, however.
In terms of direct immunization, a number of strategies have been attempted to bypass selftolerance mechanisms and stimulate active immunity to prevent infection. These include approaches using bacterially-expressed full-length PrP, dimeric PrP, synthetic PrP peptides and polypeptides with various adjuvants and various combinations of the above [106-109]. Unfortunately, anti-PrP titers in all cases tended to be low and more importantly all attempts were nonprotective against prion infection. In an attempt to exploit the speciesspecific differences in PrPC, wild-type mice were immunized with a cDNA coding for human PrPC linked to a T-cell immunostimulatory epitope. In these studies, tolerance was effectively broken in mice given three successive injections of the cDNA construct, as evidenced by generation of autoantibodies directed against the native prion protein [110]. More recently, research has focused on the initiation of T-cell based immunity in order to break the natural tolerance to PrPC. In one such study, dendritic cells were pre-loaded with prion protein peptides and injected into wild-type mice at 15 day intervals [111]. Spleen cells and sera collected 10 days after the final challenge demonstrated that T cells could be induced to produce a good lymphokine response as defined by Interferon-gamma and IL-4 release. When administered prior to challenge with the scrapie agent, PrP-loaded DCs were capable of slowing the disease progression, suggesting that initiating an anti- PrP T cell response may be one means of providing some protection against disease. It has also been suggested that, analogous to cancer therapies, the inoculation of PrPspecific T cells may be used to slow development of prion disease in affected individuals [93,112].
In order to avoid potential autoimmune responses of prion vaccination, investigators have targeted regional immunity at the portal of entry (the mucosa) rather than systemic immunity which could lead to adverse effects. Goni et al. expressed PrP in attenuated Salmonella as a live oral vaccine, which resulted in a significant delay in onset of prion disease in mice [113]. Vaccines based on Salmonella vectors have been used previously in ruminants, and may be an inexpensive route to prevent the spread of prion disease in animals [114]. It will be crucial, however, to limit immunity to the gut, as systemic (and in particular neurological) immunity may lead to significant neuropathology. Following direct intracerebral injection of anti-PrP antibodies, both hippocampal and cerebellar neurons were targeted with bivalent but not monovalent IgG antibodies [115]. While this may be due to direct activation of complement and initiation of Antibody-Dependent Cellular Cytotoxicity, it is equally possible that direct crosslinking of the neuronal PrP resulted directly in neurotoxicity. These questions must be resolved prior to implementation of antibody-based prevention and therapy for prion diseases. An alternative approach would be to directly target the PrPSc molecule, while maintaining tolerance to native PrPC. This approach has had some success in murine models, in which a Tyrosine-Tyrosine-Arginine (YYR) epitope of PrPC was conjugated to a leukotoxin-carrier protein to induce PrPSc-specific immunity [116]. In a murine model system, this vaccine regimen produced a strong PrPSc-specific IgG response, suggesting potential for development of a PrPSc-specific vaccine in the absence of autoimmune complications. It is noteworthy that IgG1 titers were found also within the cerebral spinal fluid and mucosal secretions, suggesting the potential for systemic protection against prion infection. Clearly, more work is necessary, however the potential for active protection against TSEs by direct vaccination remains a possible, and highly desirable, resolution to the potential economic and health threat of prion agents.
Acknowledgment
This work was supported by the NIAID-NIH PO1 AI 77774-01 “Pathogenesis, Transmission and Detection of Zoonotic Prion Diseases”, and NIAID-NIH grant 1R15AI072757. The authors thank April Beyer for assistance in preparation of the manuscript.
References
- Coffey B (2004) The economic impact of BSE on the US Beef Industry: Product Value Losses, Regulatory Costs, and Consumer Reactions., in Kansas State University Ag. Experiment Station and Cooperative Extension Service.
- Mitra D, Amaratunga C, Sutherns R, Pletsch V, Corneil W, et al. (2009) The psychosocial and socioeconomic consequences of bovine spongiform encephalopathy (BSE): a community impact study. J Toxicol Environ Health A 72:1106-1112.
- Ryou C (2007) Prions and prion diseases: fundamentals and mechanistic details. J Microbiol Biotechnol 17: 1059-1070.
- Belay ED, Schonberger LB (2005) The public health impact of prion diseases. Annu Rev Public Health 26: 191-212
- Nathanson N, Wilesmith J, Griot C (1997) Bovine spongiform encephalopathy (BSE): causes and consequences of a common source epidemic. Am J Epidemiol 145: 959-969.
- Ferguson-Smith MA, Richt JA (2009) Rare BSE mutation raises concerns over risks to publichealth. Nature 457: 1079.
- Colchester AC, Colchester NT (2005) The origin of bovine spongiform encephalopathy: the human prion disease hypothesis. Lancet 366: 856-861.
- Eloit M, Adjou K, Coulpier M, Fontaine JJ, Hamel R, et al. (2005) BSE agent signatures in a goat. Vet Rec 156: 523-524.
- Hoag H (2003) BSE case rattles Canadian officials. Nature 423: 467.
- Richt JA, Kunkle RA, Alt D, Nicholson EM, Hamir AN, et al. (2007) Identification and characterization of two bovine spongiform encephalopathy cases diagnosed in the United States. J Vet Diagn Invest 19: 142-154.
- Richt JA, Hall SM (2008) BSE case associated with prion protein gene mutation. PLoS Pathog 4: e1000156.
- Schneider K, Fangerau H, Michaelsen B, Raab WH (2008) The early history of the transmissible spongiform encephalopathies exemplified by scrapie. Brain Res Bull 77: 343-355.
- Stahl N, Baldwin MA, Hecker R, Pan KM, Burlingame AL, et al. (1992) Glycosylinositol phospholipid anchors of the scrapie and cellular prion proteins contain sialicacid. Biochemistry 31: 5043-5053.
- Prusiner SB (1998) Prions. Proc Natl Acad Sci U S A 95: 13363-13383.
- Linden R, Martins VR, Prado MA, Cammarota M, Izquierdo I, et al. (2008) Physiology of the prion protein. Physiol Rev 88: 673-728.
- de Almeida CJ, Chiarini LB, da Silva JP, E Silva PM, Martins MA, et al. (2005) The cellular prion protein modulate sphagocytosis and inflammatory response. J Leukoc Biol 77: 238-246.
- Richt JA, Kasinathan P, Hamir AN, Castilla J, Sathiyaseelan T, et al. (2007) Production of cattle lacking prion protein. Nat Biotechnol 25: 132-138.
- Sailer A, Bueler H, Fischer M, Aguzzi A, Weissmann C, et al. (1994) No propagation of prions in mice devoid of PrP. Cell 77: 967-968.
- Lasmezas CI (2003) Putative functions of PrP(C). Br Med Bull 66: 61-70.
- Martins VR, Linden R, Prado MA, Walz R, Sakamoto AC, et al. (2002) Cellular prion protein: on the road for functions. FEBS Lett 512: 25-28.
- Bueler H, Fischer M, Lang Y, Bluethmann H, Lipp HP, et al. (1992) Normal development and behaviour of mice lacking the neuronal cell-surface PrP protein. Nature 356: 577-582.
- Cohen FE, Pan KM, Huang Z, Baldwin M, Fletterick RJ, et al. (1994) Structural clues to prion replication. Science 264: 530-531.
- Clarke AR, Jackson GS, Collinge J (2001) The molecular biology of prion propagation. Philos Trans R Soc Lond B Biol Sci 356: 185-195.
- Gilch S, Winklhofer KF, Groschup MH, Nunziante M, Lucassen R, et al. (2001) Intracellular re-routing of prion protein prevents propagation of PrP(Sc) and delays onset of prion disease. EMBO J 20: 3957-3966.
- Dickmeiss E, Gerstoft J (2002) Blood infectivity in transmissible spongiform encephalopathies. APMIS 110: 99-103.
- Castilla J, Morales R, Saa P, Barria M, Gambetti P, et al. (2008) Cell-free propagation of prion strains. EMBO J 27: 2557-2566.
- Thorne L, Terry LA (2008) Invitro amplification of PrPSc derived from the brain and blood of sheep infected with scrapie. J Gen Virol 89: 3177-3784.
- Sigurdson CJ, Miller MW (2003) Other animal prion diseases. Br Med Bull 66: 199-212.
- O'Rourke KI, Besser TE, Miller MW, Cline TF, Spraker TR, et al. (1999) PrP genotypes of captive and free-ranging Rocky Mountain elk (Cervus elaphus nelsoni) with chronic wasting disease. J Gen Virol 80: 2765-2769.
- Groschup MH, Buschmann A (2008) Rodent models for prion diseases. Vet Res 39: 32.
- Collinge J, Clarke AR (2007) A general model of prion strains and their pathogenicity. Science 318: 930-936.
- 32. Fernandez-Borges N, deCastro J, Castilla J (2009) In vitro studies of the transmission barrier. Prion 3: 220-223.
- Blanchong JA, Heisey DM, Scribner KT, Libants SV, Johnson C, et al (2009) Genetic susceptibility to chronic wasting disease in free-ranging white-tailed deer: complement component C1q and Prnp polymorphisms. Infect Genet Evol 9: 1329-1335.
- Johnson CJ, Herbst A, Duque-Velasquez C, Vanderloo JP, Bochsler P, et al. (2011) Prion protein polymorphisms affect chronic wasting disease progression. PLoS One 6: e17450.
- Kelly AC, Mateus-Pinilla NE, Diffendorfer J, Jewell E, Ruiz MO, et al. (2008) Prion sequence polymorphisms and chronic wasting disease resistance in Illinois white-tailed deer (Odocoileus virginianus). Prion 2: 28-36.
- Wilson GA, Nakada SM, Bollinger TK, Pybus MJ, Merrill EH, et al. (2009) Polymorphisms at the PRNP gene influence susceptibility to chronic wasting disease in two species of deer (Odocoileus Spp.) in western Canada. J Toxicol Environ Health A 72: 1025-1029.
- vanKeulen LJ, Schreuder BE, Meloen RH, Mooij-Harkes G, Vromans ME, et al. (1996) Immuno histochemical detection of prion protein in lymphoid tissues of sheep with natural scrapie. J Clin Microbiol 34: 1228-1231.
- Greenlee JJ, Hamir AN, WestGreenlee MH (2006) Abnormal prion accumulation associated with retinal pathology in experimentally inoculated scrapie-affected sheep. Vet Pathol 43: 733-739.
- O'Rourke KI, Spraker TR, Zhuang D, Greenlee JJ, Gidlewski TE, et al. (2007) Elk with a long incubation prion disease phenotype have a unique PrPd profile. Neuro report 18: 1935-1938.
- Chen C, Shi Q, Tian C, Li Q, Zhou W, et al. (2011) The first Chinese case of Creutzfeldt-Jakob disease patient with R208H mutation in PRNP. Prion 5: 232-234.
- Haik S, Brandel JP (2011) Biochemical and strain properties of CJD prions:complexity versus simplicity. J Neuro chem 119: 251-261.
- Eaton SL, Rocchi M, Gonzalez L, Hamilton S, Finlayson J, et al. (2007) Immunological differences between susceptible and resistant sheep during the preclinical phase of scrapie infection. J Gen Virol 88: 1384-1391.
- Aguzzi A, Heikenwalder M (2006) Pathogenesis of prion diseases: current status and future out look. Nat Rev Microbiol 4: 765-775.
- Weissmann C, Raeber AJ, Montrasio F, Hegyi I, Frigg R, et al. (2001 Prions and the lymphoreticular system. Philos Trans R Soc Lond B Biol Sci 356: 177-184.
- Hamir AN, Kunkle RA, Miller JM, Hall SM (2006) Abnormal prion protein in ectopic lymphoid tissue in a kidney of anasymptomatic white-tailed deer experimentally inoculated with the agent of chronic wasting disease. Vet Pathol 43: 367-369.
- Mulcahy ER, Bartz JC, Kincaid AE, Bessen RA (2004) Prion infection of skeletal muscle cells and papillae in the tongue. J Virol 78: 6792-6798.
- Angers RC, Browning SR, Seward TS, Sigurdson CJ, Miller MW, et al. (2006) Prions in skeletal muscles of deer with chronic wasting disease. Science 311: 1117.
- ElShikh ME, El Sayed RM, Sukumar S, Szakal AK, Tew JG, et al. (2010) Activation of B cells by antigens on follicular dendritic cells. Trends Immunol 31: 205-211.
- Vinuesa CG, Linterman MA, Goodnow CC, Randall KL (2010) T cells and follicular dendritic cells in germinal center B-cell formation and selection. Immunol Rev 237: 72-89.
- Gatto D, Brink R (2010) The germinal center reaction. J Allergy Clin Immunol 126: 898-907.
- Cyster JG (2010) B cell follicles and antigen encounters of the third kind. Nat Immunol 11: 989-996.
- Garin A, Meyer-Hermann M, Contie M, Figge MT, Buatois V, et al. (2010) Toll-like receptor 4 signaling by follicular dendritic cells is pivotal for germinal center on set and affinity maturation. Immunity 33: 84-95.
- Phan TG, Grigorova I, Okada T, Cyster JG (2007) Subcapsular encounter and complement-dependent transport of immune complexes by lymph node B cells. Nat Immunol 8: 992-1000.
- Mabbott NA, Bruce ME (2002) Follicular dendritic cells as targets for intervention intransmissible spongiform encephalopathies. Semin Immunol 14: 285-293.
- Aucouturier P, Carnaud C (2002) The immunesystem and prion diseases: a relationship of complicity and blindness. J Leukoc Biol 72: 1075-1083.
- SassaY, Kataoka N, Inoshima Y, Ishiguro N (2010) Anti-PrP antibodies detected at terminal stage of prion-affected mouse. Cell Immunol 263: 212-218.
- Klein MA, Kaeser PS, Schwarz P, Weyd H, Xenarios I, et al. (2001) Complement facilitates early prion pathogenesis. Nat Med 7: 488-492.
- Zabel MD, Heikenwalder M, Prinz M, Arrighi I, Schwarz P, et al. (2007) Stromal complement receptor CD21/35 facilitates lymphoid prion colonization and pathogenesis. J Immunol 179: 6144-6152.
- Dumestre-Perard C, Osmundson J, Lemaire-Vieille C, Thielens N, Grives A, et al. (2007) Activation of classical pathway of complement cascade by soluble oligomers of prion. Cell Microbiol 9: 2870-2879.
- Mabbott NA, Bruce ME, Botto M, Walport MJ, Pepys MB (2001) Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie. Nat Med 7: 485-487.
- Foster N, Macpherson GG (2010) Murine cecal patch Mcells transport infectious prions in vivo. J Infect Dis 202: 1916-1919.
- Jeffrey M, González L, Espenes A, Press CM, Martin S, et al. (2006) Transportation of prion protein across the intestinal mucosa of scrapie-susceptible and scrapie-resistant sheep. J Pathol 209: 4-14.
- Jeffrey M, McGovern G, Siso S, Gonzalez L (2011) Cellular and sub-cellular pathology of animal prion diseases: relationship between morphological changes, accumulation of abnormal prion protein and clinical disease. Acta Neuropathol 121: 113-134.
- Miyazawa K, Kanaya T, Takakura I, Tanaka S, Hondo T, et al. (2010) Transcytosis of murine-adapted bovine spongiform encephalopathy agents in an in vitro bovine M cell model. J Virol 84:12285-12291.
- Takakura I, Miyazawa K, Kanaya T, Itani W, Watanabe K, et al. (2011) Orally administered prion protein is incorporated by m cells and spreads into lymphoid tissues with macrophages in prion protein knock out mice. Am J Pathol 179: 1301-1309.
- Huang FP, Farquhar CF, Mabbott NA, Bruce ME, MacPherson GG (2002) Migrating intestinal dendritic cells transport PrP(Sc) from the gut. J Gen Virol 83: 267-271.
- Langevin C, Gousset K, Costanzo M, Richard-Le Goff O, Zurzolo C (2010) Characterization of the role of dendritic cells in prion transfer to primary neurons. Biochem J 431: 189-198.
- Jeffrey M, McGovern G, Martin S, Goodsir CM, Brown KL (2000) Cellular and sub-cellular localisation of PrP in the lymphoreticula rsystem of mice and sheep. ArchVirol 16: 23-38.
- Davies ML, Hopkins LJ, Halliday S, Houston F, Hunter N, et al. (2004) Architecture of secondary lymphoid tissue in sheep experimentally challenged with scrapie. Immunology 111: 230-236.
- Aguzzi A, Heikenwalder M (2005) Prions, cytokines, and chemokines:a meeting in lymphoid organs. Immunity 22: 145-154.
- Kosco-Vilbois MH (2003) Are follicular dendritic cells really good for nothing? Nat Rev Immunol 3: 764-769.
- Keele BF, Tazi L, Gartner S, Liu Y, Burgon TB, et al. (2008) Characterization of the follicular dendritic cell reservoir of human immunodeficiency virus type1. J Virol 82: 5548-5561.
- Aguzzi A, Krautler NJ (2010) Characterizing follicular dendritic cells: A progress report. Eur J Immunol 40: 2134-2138.
- Brown KL, Stewart K, Ritchie DL, Mabbott NA, Williams A, et al. (1999) Scrapie replication in lymphoid tissues depends on prion protein-expressing follicula rdendritic cells. Nat Med 5: 1308-1312.
- Thielen C, Melot F, Jolois O, Leclercq F, Tsunoda R, et al. (2001) Isolation of bovine follicular dendritic cells allows the demonstration of a particular cellular prion protein. Cell Tissue Res 306: 49-55.
- McGovern G, Mabbott N, Jeffrey M (2009) Scrapie affects the maturation cycle and immune complex trapping by follicular dendritic cells in mice. PLoS One 4: e8186.
- Herrmann LM, Cheevers WP, Davis WC, Knowles DP, O'Rourke KI (2003) CD21-positive follicular dendritic cells: A possible source of PrPSc in lymphnode macrophages of scrapie-infected sheep. Am J Pathol 162: 1075-1081.
- Beringue VP, Couvreur, Dormont D (2002) Involvement of macrophages in the pathogenes is of transmissible spongi for mencephalopathies. Dev Immunol 9: 19-27.
- Gilch S, Schmitz F, Aguib Y, Kehler C, Bulow S, et al. (2007) CpG and LPS can interfere negatively with prion clearance in macrophage and microglial cells. FEBS J 274: 5834-5844.
- Sigurdson CJ, Heikenwalder M, Manco G, Barthel M, Schwarz P, et al. (2009) Bacterial colitis increases susceptibility to oral prion disease. J Infect Dis 199: 243-252.
- Tal Y, Souan L, Cohen IR, Meiner Z, Taraboulos A, et al. (2003) Complete Freund's adjuvant immunization prolongs survival in experimental prion disease in mice. J Neurosci Res 71: 286-290.
- Spinner DS, Cho IS, Park SY, Kim JI, Meeker HC, et al. (2008) Accelerated prion disease pathogenesis in Toll-like receptor 4 signaling-mutant mice. J Virol 82: 10701-10708.
- Mathiason CK, Hayes-Klug J, Hays SA, Powers J, Osborn DA, et al. (2010) B cells and platelets harbor prion infectivity in the blood of deer infected with chronic wasting disease. J Virol 84: 5097-5107.
- Houston F, McCutcheon S, Goldmann W, Chong A, Foster J, et al. (2008) Prion diseases are efficiently transmitted by blood transfusion in sheep. Blood 112: 4739-4745.
- Siso S, Gonzalez L, Houston F, Hunter N, Martin S, et al. (2006) The neuropathologic phenotype of experimental ovine BSE is maintained after blood transfusion. Blood 108: 745-748.
- Siso S, Jeffrey M, Houston F, Hunter N, Martin S, et al. (2010) Pathological phenotype of sheep scrapie after blood transfusion. J Comp Pathol 142: 27-35.
- Castilla J, Saa P, Soto C (2005) Detection of prions in blood. Nat Med 11: 982-985.
- Saa P, Castilla J, Soto C (2006) Presymptomatic detection of prions in blood. Science 313: 92-94.
- Edwards JC, Moore SJ, Hawthorn JA, Neale MH, Terry LA (2010) PrP(Sc) is associated with B cells in the blood of scrapie-infected sheep.Virology 405: 110-119.
- Shyu WC, Liu DD, Lin SZ, Li WW, Su CY, et al. (2008) Implantation of olfactory ensheathing cells promotes neuroplasticity in murine models of stroke. J Clin Invest 118: 2482-2495.
- Sakaguchi S (2009) Prospects for preventative vaccines against prion diseases. Protein Pept Lett 16: 260-270.
- Petsch B, Muller-Schiffmann A, Lehle A, Zirdum E, Prikulis I, et al. (2011) Biological effects and use of PrPSc- and PrP- specific antibodies generated by immunization with purified full-length native mouse prions. J Virol 85: 4538-4546.
- Iken S, Bachy V, Gourdain P, Lim A, Gregoire S, et al. (2011) Th2-polarised PrP-specific Transgenic T-cells confer partial protection against murine scrapie. PLoS Pathog 7: e1002216.
- van Keulen LJ, Vromans ME, van Zijderveld FG (2002) Early and late pathogenesis of natural scrapie infection in sheep. APMIS 110: 23-32.
- Andreoletti O, Berthon P, Levavasseur E, Marc D, Lantier F, et al. (2002) Phenotyping of protein-prion (PrPsc)-accumulating cells in lymphoid and neural tissues of naturally scrapie-affected sheep by double-labeling immunohistochemistry. J Histochem Cytochem 50: 1357-1370.
- Gregoire S, Bergot AS, Feraudet C, Carnaud C, Aucouturier P, et al. (2005) The murine B cell repertoire is severely selected against endogenous cellular prion protein. J Immunol 175: 6443-6449.
- Enari M, Flechsig E, Weissmann C (2001) Scrapie prion protein accumulation by scrapie-infected neuroblastoma cells abrogated by exposure to a prion protein antibody. Proc Natl Acad Sci USA 98: 9295-9299.
- Pankiewicz J, Prelli F, Sy MS, Kascsak RJ, Kascsak RB, et al. (2006) Clearance and prevention of prion infection in cell culture by anti-PrP antibodies. Eur J Neurosci 23: 2635-2647.
- Peretz D, Williamson RA, Kaneko K, Vergara J, Leclerc E, et al. (2001) Antibodies inhibits prion propagation and clear cell cultures of prion infectivity. Nature 412: 739-743.
- Donofrio G, Heppner FL, Polymenidou M, Musahl C, Aguzzi A (2005) Paracrine inhibition of prion propagation by anti-PrP single-chain Fv miniantibodies. J Virol 79: 8330-8338.
- Wuertzer CA, Sullivan MA, Qiu X, Federoff HJ (2008) CNS delivery of vectored prion-specific single-chain antibodies delays disease onset. Mol Ther 16: 481-486.
- Heppner FL, Musahl C, Arrighi I, Klein MA, Rulicke T, et al. (2001) Prevention of scrapie pathogenesis by transgenic expression of anti-prion protein antibodies. Science 294: 178-182.
- Sigurdsson EM, Brown DR, Daniels M, Kascsak RJ, Kascsak R, et al. (2002) Immunization delays the onset of prion disease in mice. Am J Pathol 161: 13-17.
- Sigurdsson EM, Sy MS, Li R, Scholtzova H, Kascsak RJ, et al. (2003) Anti-prion antibodies for prophylaxis following prion exposure in mice. Neurosci Lett 336: 185-187.
- White AR, Enever P, Tayebi M, Mushens R, Linehan J, et al. (2003) Monoclonal antibodies inhibit prion replication and delay the development of prion disease. Nature 422: 80-83.
- Koller MF, Grau T, Christen P (2002) Induction of antibodies against murine full-length prion protein in wild-type mice. J Neuroimmunol 132: 113-116.
- Polymenidou M, Heppner FL, Pellicioli EC, Urich E, Miele G, et al. (2004) Humoral immune response to native eukaryotic prion protein correlates with anti- prion protection. Proc Natl Acad Sci USA: 14670-14676.
- Gilch S, Wopfner F, Renner-Müller I, Kremmer E, Bauer C, et al. (2003) Polyclonal anti- PrP auto- antibodies induced with dimeric PrP interfere efficiently with PrPSc propagation in prion- infected cells. J Biol Chem 278: 18524-18531.
- Heppner FL, Aguzzi A (2004) Recent developments in prion immunotherapy. Curr Opin Immunol 16: 594-598.
- Alexandrenne C, Wijkhuisen A, Dkhissi F, Hanoux V, Priam F, et al. (2010) Electrotransfer of cDNA coding for a heterologous prion protein generates autoantibodies against native murine prion protein in wild- type mice. DNA Cell Biol 29: 121-131.
- Bachy V, Ballerini C, Gourdain P, Prignon A, Iken S, et al. (2010) Mouse vaccination with dendritic cells loaded with prion protein peptides overcomes tolerance and delays scrapie. J Gen Virol 91: 809-820.
- Carnaud C, Bachy V (2010) Cell-based immunotherapy of prion diseases by adoptive transfer of antigen- loaded dendritic cells or antigen- primed CD(4+) T lymphocytes. Prion 4: 66-71.
- Goni F, Knudsen E, Schreiber F, Scholtzova H, Pankiewicz J, et al. (2005) Mucosal vaccination delays or prevents prion infection via an oral route. Neuroscience 133: 413-421.
- Villarreal-Ramos B, Manser J, Collins RA, Dougan G, Chatfield SN, et al. (1998) Immune responses in calves immunised orally or subcutaneously with a live Salmonella typhimurium aro vaccine. Vaccine 16: 45-54.
- Solforosi L, Criado JR, McGavern DB, Wirz S, Sanchez-Alavez M, et al. (2004) Cross- linking cellular prion protein triggers neuronal apoptosis invivo. Science 303: 1514-1516.
- Hedlin PD, Cashman NR, Li L, Gupta J, Babiuk LA, et al. (2010) Design and delivery of a cryptic PrP(C) epitope for induction of PrP(Sc)- specific antibody responses. Vaccine 28: 981-988.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 16503
- [From(publication date):
specialissue-2012 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11827
- PDF downloads : 4676