Research Article Open Access
Surgical Treatment of Fracture in Atrophic Jaw
José Carlos Garcia de Mendonça1, Ellen Cristina Gaetti Jardim2*, Gustavo Rodrigues Manrique2, Helena Bacha Lopes2 and Gileade Pereira Freitas21Oral and Maxillofacial Surgeon, MSc, PhD in the Post-Graduation Course School of Dentistry of Campo Grande, Federal University of Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil
2Oral and Maxillofacial Surgeon Resident in the Post-Graduation Course School of Dentistry of Campo Grande, Federal University of Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil
- Corresponding Author:
- Ellen Cristina Gaetti Jardim
Oral and Maxillofacial Surgeon Resident in the
Post-Graduation Course School of Dentistry of Campo Grande
Uricuri-475, Vl. Olinda, CEP-79060-040
Campo Grande – MS, Brazil
Tel: +55-67- 81728272
E-mail: ellengaetti@gmail.com
Received date: December 14, 2011; Accepted date: January 09, 2012; Published date: January 11, 2012
Citation: Mendonça JCGD, Jardim ECG, Manrique GR, Lopes HB, Freitas GP (2012) Surgical Treatment of Fracture in Atrophic Jaw. J Biotechnol Biomaterial 2:123. doi:10.4172/2155-952X.1000123
Copyright: © 2012 Mendonça JCGD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
Abstract
Introduction:Mandible fractures are common injuries in the facial bones. It has a varied etiology, especially automobile accidents, bicycle accidents, motorcycle accidents and assaults.
Objective: This study aims to illustrate a case of a patient with bilateral atrophic mandibular fractures treated surgically.
Clinical case:male patient, 48 years old, victim an accident at work causing bilateral mandibular body fractures treated by internal rigid fixation with titanium plates and screws with the making of access submandibular Risdon bilaterally.
Conclusion: The authors present a discussion of the controversy involved in this type of treatment and showing the advantages of transcutaneous approach for the treatment of mandibular fractures.
Keywords
Mandibular fractures; Internal fixation of fractures; Open Access
Introduction
The face consists of a set of bones articulated with each other, with the jaw as the only mobile bone. The position, prominence and anatomical configuration of the jaw, make it correspond to about 20% to 50% of cases of facial fractures [1]. Some authors consider the second jaw bone of the skull is more susceptible to injury [2].
Mandible fractures can be caused by direct or indirect injuries resulting from automobile accidents, bicycle, motorcycle, work, sports injuries, falls or assaults [3]. Signs and symptoms of fractures include intense sensitivity to palpation, pain, from mild to severe trismus, edema, hematoma, sialorrhea, foul breath, facial asymmetry, crepitation, and bone changes of occlusion [4,5].
When surgery is necessary, many aspects must be taken into consideration, as the possible functional and aesthetic postoperative sequels, given the abundant vascularization and innervation of the region, where the external carotid artery enters the parotid gland and sends his two terminal branches the maxillary and superficial temporal artery [6,7].
The facial nerve is another noble structure that also travels a path inside the parotid gland, medially to the external carotid artery and retromandibular vein, dividing in temporofacial and cervicofacial branches, that originates the terminal branches of facial nerve: temporal, zygomatic, buccal, marginal mandibular, and cervical [8].
These fractures account for less than 5% of all fractures of the jaw as the weak bone is offset by the lower risk activity in the elderly, framed in less physical activity overall in this age group. With the overall decrease in bone mass is an approach the areas of tension and compression on the physiology of functional jaw, implying a high relative position of the inferior dental nerve which is in some cases just below the mucosa, in part of the tract [9].
Due to the greater fragility fractures usually result from trauma to great instability, displaced fragments, there are not rare cases of bilateral and even comminuted fractures. Given the importance of the topic, this study aims to illustrate a case of a patient with bilateral fracture atrophic mandible treated surgically.
Case Report
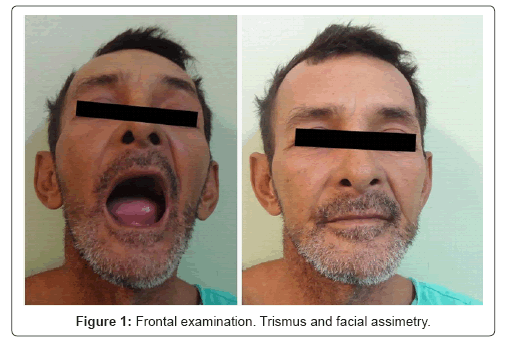
Patient male, 48 years old, sought treatment in the Hospital Center of the Federal University of Mato Grosso do Sul, complaining of difficulty in mouth opening and pain in the jaw region on both sides. The patient reported being a victim of an accident at work resulted to extraoral physical examination in edema in the lower third of face and facial asymmetry at the expense of the same (Figure 1).
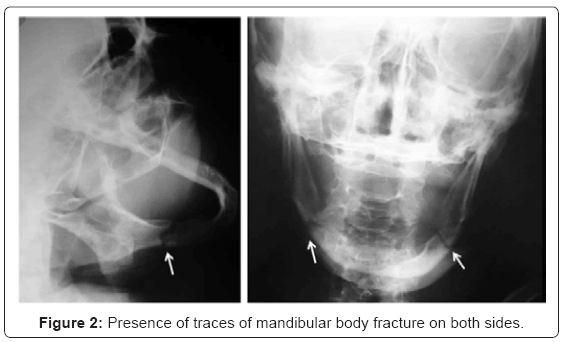
Intraoral clinical examination noted the presence of crepitus bilateral mandibular bone in the body accentuated mobility as well as the site mentioned above (Figure 1). The imaging studies (radiographs anterior- posterior and lateral oblique jaw) showed the presence of traces of mandibular body fracture on both sides, view a complete fracture of a bone atrophic, measuring approximately 12mm in height (Figure 2).
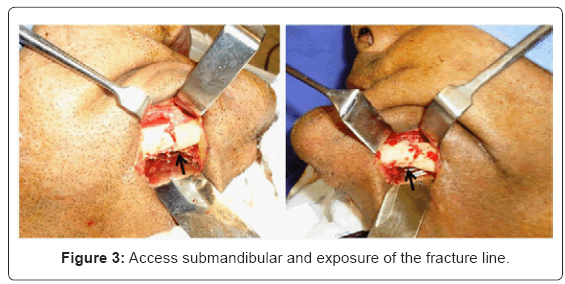
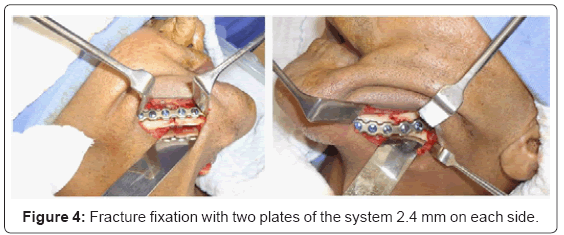
After general anesthesia and nasotracheal intubation antisepsis and placement of sterile surgical drapes was performed. The submandibular incision and divulsion by plans was then made providing a wide field of view and direct access to the traumatized area detached periosteal for exposure of the fracture line. A standard submandibular incision is made with dissection along, avoiding any damage to the upper trunk of the facial nerve. The divulsion is directed antero-superior and slightly medial (Figure 3). After the realignment of the base was performed mandibular fracture fixation with two plates of the system 2.4 mm on each side, due to atrophy of the mandibular ridge, showing good reduction of fractured stumps and stability (Figure 4).
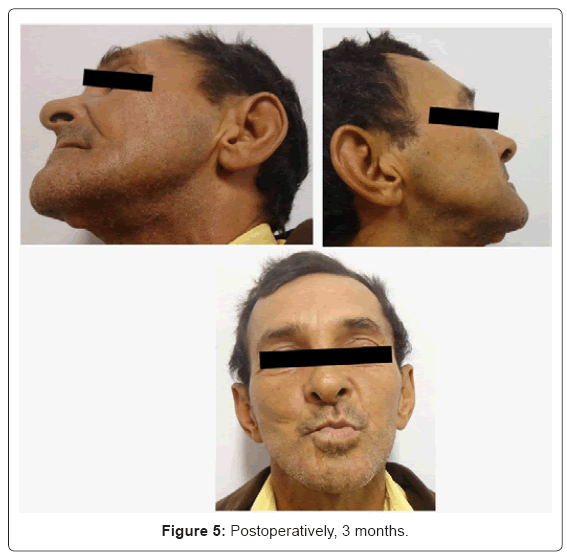
In the post-operative controls, a good healing aspect of surgical approach was observed, the presence of transient motor deficit of the muscles innervated by the facial nerve, as well as satisfactory mouth opening and occlusion (Figure 5).
Results
Although frailty is associated with mandibular elderly patients, becoming more common is the presence of edges in atrophic mandibular fractures in younger patients but that still supports the procedures under general anesthesia in a satisfactory manner. In addition, the mandibular body fracture of the case presented was very displace and bilateral, with the need to use open reduction and internal fixation to establish an appropriate treatment.
As with any surgical procedure, it is clear that detailed knowledge of local anatomy and the application of meticulous surgical technique are necessary, especially in the dissection of the region near to the facial nerve.
Marciani [10] believes that the treatment of fractures in atrophic edentulous jaws in the region of the body should be in an open, using internal fixation and may involve the autogenous bone grafts, since the medical condition permits. For the author, closed techniques in these cases have a high probability of poor and / or non-union or result in any functional impairment for patients.
Although rare, this type of fracture involves an aggressive attitude to the use of plates of appropriate size and thickness, bone grafts and the frequent need for absolute respect for a good stability to achieve a reduction in complications, not forgetting that the main objective is to achieve a good fracture healing for fast healing to dentures.
Thus the surgeon is essential to know in detail the local anatomy and the application of meticulous surgical technique, particularly on dissection of the region for adequate exposure of important structures belonging to the submandibular area, without any damage to the facial nerve [11]. In this context, access to Risdon shows good operative field and is configured as a secure, widely used in surgical means. In this regard, severe facial trauma which leads to fragmentation of bone stumps, it is essential a direct view of the region to intervene. Without adequate exposure of the fracture the resolution of the clinical case in question would be compromised if the surgical approach were reduced or were just simply access the oral cavity.
In situations where the atrophy of the alveolar ridge is so severe that the bone height is less than 7mm, require that techniques of bone grafts from donor sites in the distance, as the iliac crest [12].
In our case the fact that the patient is a carrier of bone structure of atrophic mandible with a bone weakened due to generalized atrophy, reduced osteogenic capacity and, consequently, reduced blood flow, making it more likely to happen fracture [13,14]. Which leads us to oppose the findings of Barber [15] believes that the treatment of fractures in atrophic edentulous jaws, fixed dentures with circumferential wires and the use of maxillomandibular immobilization promote the proper stabilization fracture site, allowing the bone repair. For the author, conservative treatment is feasible, and the absence of teeth enables the fracture reduction, not a difficult aspect, as in patient partial and / or complete denture.
Conversely, some authors as Goldschmit et al. [16], Luhr et al. [17] and Marciani [18] stated that even elderly patients, since there are no systemic contraindications, are best suited to surgery for the fracture, rather than prolonged periods of immobilization jaw. Still, the use of hearing or gutters, used to keep the mouth immobilized, is often traumatic to the buccal mucosa and hard to sanitize and is very painful for the patient [19].
One of the measures chosen against mandibular fractures in geriatric patients is conservative treatment, which is conduct taken against fractures said no favorable action of the muscles of mastication, so no displacement of bone fragments. In these cases, a simple monitoring and guidance will be consolidated at other time. There are many complications of the different methods used for fracture reduction, as demonstrated by Toledo Filho et al. [20] infections, subcutaneous emphysema, edema, osteomyelitis, and bleeding are the most frequent occurrences.
When opting for surgical treatment, one should choose the best surgical approach to fracture. The intra-oral access is indicated, especially the anterior mandible that are not associated with impairment of comminuted alveolar ridge and / or associated soft tissue damage. This fact confirms the case as presented was comminuted fracture of the posterior mandibular region whose extra-oral access when well implemented provides a better fixation of fractures lead to a better exposure of the same.
When correlated to the use of rigid internal fixation in atrophic jaws is imperative the need for increased strength of fixation based on two basic principles of maxillofacial trauma: Load Sharing, when there is good amount of bone available in which the loads are functional divided between the remaining bone and the fixation system and Load Bearing, in which the fastening system supports all or most functional load until bone healing to occur, as is the case of comminuted fractures in atrophic mandibles and free bone grafts targeted performed in the jaw rather painful for the patient [19].
Thus, the atrophic jaws require high strength bonding, even in patients with poor muscle strength and muscle apparently reduced. Thus, the use of more robust means of fixation is necessary in patients with mandibular height as well as decreased thickness generated by atrophy, having to support all functional loads. Not knowing these concepts can lead to complications that include infection, nonunion, poor fracture union and the board [21].
Open reduction of fractures of the edentulous jaws, with fixation with plates lead to a better outcome according to Fonseca [22] and Scolozzi & Richter [23]. In the case report, because it is comminuted fracture of the jaw, surgery for fracture reduction and fixation is indicated. The rigid internal fixation allows the treatment of mandibular fractures with maintaining stability under early functional activity, and reduces or eliminates the use of lock jaw after surgery.
The patient did not have any functional deficits after the surgical procedure, so we stress that the approaches indicated and submandibular when well executed can and should be performed, since they allow adequate exposure to the region of the mandibular angle and body and related structures making satisfactory remembering need for the skill of the surgeon and his team in making the trans-operative approach.
Although the patient is edentulous total, the same did not use any prosthetic devices. In the case of prosthetic rehabilitation of the patient, the best approach in the face of widespread atrophy of the jaw bone is the realization of osseointegrated implants in the anterior and the making of over-denture implants, being the second option to remove internal rigid fixation and making full dentures after bone healing.
Conclusion
Through our study we can conclude that treatment with the open accessed submandibular region was effective with no complications and the installation of such equipment fixation showed satisfactory results.
References
- Wulkan M, Parreira JG Jr, Botter DA (2005) Epidemiologia do trauma facial. Rev Assoc Med Bras 51: 290-295.
- Patrocínio LG, Patrocínio JA, Borba BH, Bonatti Bde S, Pinto LF, et al. (2005) Mandíbular fracture: análise de 293 pacientes tratados no Hospital de Clínicas da Universidade Federal de Uberlândia. Braz J Otorhinolaryngol 71: 560-565.
- Gaetti-Jardim EC, Faverani LP, Guilinelli JL, Queiroz TP, Filho OM, et al. (2009) Epidemiologia das fraturas mandibulares em pacientes atendidos na região de Araçatuba. Rev Bras Cir Cabeça Pescoço 38: 163-165.
- Sakr K, Farog IA, Zeitoun IM (2006) Review of 509 mandibular fractures treated at the University Hospital. Alexandria, Egypt. Br J Oral Maxillofac Surg 44: 107-111.
- Ellis E 3rd, Muniz O, Anand K (2003) Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg 61: 861-870.
- Dolwick MF (2007) Temporomandibular Joint Surgery for Internal Derangement. Dent Clin North Am 51: 195-208.
- Ruíz CA, Guerrero JS (2001) A new modified endaural approach for Access to the temporomandibular joint. Br J Oral Maxillof Surg 39: 371-373.
- Goss CM (1988) Gray' s Anatomy 37ªed., Rio de Janeiro: Ed. Guanabara.
- Matias JG, Andrade MR, Fernandes VS (2004) Edentulous mandible fractures osteosynthesis. Acta Méd Port 17: 145-148.
- Marciani RD (2001) Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg 59: 792-795.
- Gaetti-Jardim EC, Faverani LP, Ramalho Ferreira G, Pereira CCS, Gealh WC, et al. (2011) Acessos cirúrgicos a articulação temporomandibular: revisão de literatura. Rev Bras Cir Cabeça Pescoço 40: 46-52.
- Bell RB, Blakey GH, White RP, Hillebrand DG, Molina A (2002) Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg 60: 1135-1141.
- Peterson I, Ellis E, Hupp J, Tucker M (1998) Contemporary Oral and Maxillofacial Surgery.(3rd ed), St. Louis: Mosby.
- Garcez Filho JA, Seabra MFM, Araújo MG (2008) Retratamento de Fratura Complexa em Mandíbula Atrófica com Instalação Imediata de Implantes Dentarios. Rev Cir Traumatol Buco-Maxilo-fac 8: 39-48.
- Barber HD (2001) Conservative management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg 59: 789-791.
- Goldschmidt MJ, Castiglione CL, Assael LA, Litt MD (1995) Craniomaxillofacial trauma in the elderly. J Oral Maxillofac Surg 53: 1145-1149.
- Luhr HG, Reidick T, Merten HA (1996) Results of treatment of fractures of the atrophic edentulous mandible by compression plating. A retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg 54: 250-255.
- Marciani RD (2001) Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg 59: 792-795.
- Prein J (1998) Manual of internal fixation in the cranio-facial skeleton. Berling Heidelberg: Springer-Verlag
- Toledo Filho JL, Marzola C, Pastori CM, Zorzetto DG (1998) Utilização de miniplacas no tratamento de fraturas da mandíbula - Considerações gerais e apresentação de casos cirúrgicos. Rev APCD 52: 55-62.
- Sikes JW Jr, Smith BR, Mukherjee DP (2000) An in vitrostudy of the effect of bony buttressing on fixation strength ofa fractured atrophic edentulous mandible model. J Oral Maxillofac Surg 58: 56-61.
- Fonseca RJ (2000) Oral and Maxillofacial Trauma, (3rdedn) Philadelphia, W.B. Saunders Company 3: 500p.
- Scolozzi P, Richter M (2003) Treatment of severe mandibular fractures using AO reconstrution places. J Oral Maxillofacial Surg 61: 458-641.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 16103
- [From(publication date):
January-2012 - Apr 01, 2025] - Breakdown by view type
- HTML page views : 11471
- PDF downloads : 4632