Review Article Open Access
Smallpox: New Perspectives Regarding Risk Assessment & Management
Jan-Cedric Hansen*
Director of European Strategies at MEDCOM, a Military Medicine Division of StratAdviser Ltd, UK
- *Corresponding Author:
- Jan-Cedric Hansen
Director of European Strategies at MEDCO
a Military Medicine division of StratAdviser Ltd, UK
E-mail: jc.hansen@stratadviser.com
Received Date: August 25, 2012; Accepted Date: September 28, 2012; Published Date: September 29, 2012
Citation: Hansen JC (2012) Smallpox: New Perspectives Regarding Risk Assessment & Management. J Bioterr Biodef S4:002. doi:10.4172/2157- 2526.S4-002
Copyright: © 2012 Hansen JC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Although official stockpile of smallpox are limited to two sites, everlasting rumors of bioterrorism use of this virus make its risk assessment controversial. After a quick overview of the history of smallpox and its current situational analysis, the author presents his own vision regarding likelihood of smallpox weaponization and new trends regarding its risk management. In particular, four scenarios on how to get hold of smallpox samples are discussed as well as the following steps of potential deliberate release in light of feasibility from the terrorist standpoint. Following, early detection strategies are overviewed with a special focus on their respective limitations. Then up to date therapeutic armamentarium, including drugs under development is detailed. In conclusion, the author exposes a surprising paradox regarding the potential use of smallpox as an agent of bioterrorism by Al-Qaeda terrorists and alike.
Keywords
Smallpox; Variola; Bioterrorism; Bioweapon; Response plan; Strategy
Introduction
Smallpox is caused by either of two virus variants, Variola major and Variola minor (VARV), both members of the poxviridae family. The noun “smallpox” arouse in the 15th century to distinguish variola from syphilis known as the “great pox”; the noun “Variola” comes from the Latin word “varus” meaning “pimple”. Smallpox history dates back to ca. 1350 BCE when it spread from the Egyptians to the Hittites in Syria [1]. From the phylogenetic point of view, VARV probably mutated from the Camel pox virus in the Middle East some 6,000-10,000 years ago [2,3]. Ever since, it has been recorded throughout human history as a devastating human disease that affected up to 500 millions worldwide during the 20th century until the last naturally occurring cases being reported in 1977 in Somalia [4].
In humans, smallpox is contracted by inhalation of variola virions (virus particles) via saliva during face-to-face contact – coughing releases large amounts from mucosal lesions in the nose, throat and mouth sphere – or from pus and scabs encountered on bed sheets or other contact vectors. The clinical manifestations of acquired smallpox begin after an incubation period of 7–17 days following exposure. The initial symptoms of disease are indistinguishable from many other virus infections with a fever that can spike upwards of 39°C and may include myalgia, headache, vomiting, and prostration. The febrile phase may continue for 3-4 days before the appearance of a centrifugally distributed, systemic rash. The rash progresses from a macular to papular stage, after which vesicles evolve on day 4 and pustules on day 7 post fever onset. The WHO has divided the classical form of smallpox, caused by variola major into five clinical types [5]:
1. Ordinary smallpox that occurs in 90% of cases with a case-fatality rate ranging from 10–75% correlated with the severity of rash.
2. Modified smallpox, that occurs in 5% of cases with a case-fatality rate near 10%, less severe in its clinical presentation and frequent among previously vaccinated individuals;
3. Flat smallpox, that occurs in 5% of cases with a case-fatality rate above 80%, distinguished by a more slowly developing rash and generalized infection;
4. Haemorrhagic smallpox, that occurs in 1% of cases with casefatality rate of 100%, characterized by haemorrhages into the skin and mucous membranes;
5. Variola sine eruption, that presents as a fever without rash; thus, serological evidence is required to confirm VARV infection.
Risk assessment
Potential population threat: Two hundred years after its introduction as the smallpox vaccine, the wide spread use of Vaccinia virus (VACV), another member of the poxviridae family, has enabled the Global Commission for the Certification of Smallpox Eradication to declare the world free of smallpox in December, 1979. The World Health Assembly, the decision-making body of World Health Organization (WHO), ratified this declaration 6 months later. Subsequent cessation of vaccination has resulted in an ever-growing immunologically naive human population that would be at risk and VARV should be used as an agent of bioterrorism [6]. To evaluate the intensity of the threat is simple: the median population age of the 27 European countries is around 40 years (ranging between 34 years in Ireland and 44 years in Germany) while the median age of Americans is 37 years [7,8]. This means that nearly half of the EU and US population would be decimated by a smallpox terrorist outbreak.
Bioterrorism attractiveness: Smallpox is attractive as an agent of bioterrorism because it does not cause a specific illness for several days giving infected individuals time to scatter far from the infection site (making it difficult to track down the initial spot and multiplying face to face contacts), it can be spread as an aerosol, or simply by contact from person to person. An aerosol release of variola virus would disseminate widely, given the considerable stability of the VARV in aerosol form and the likelihood that the infectious dose is very small [9]. Due to its social representation within the world population; it is likely to create mass panic and disruption within the targeted social group. In recent history, widespread concerns and, sometimes, panic occurred, even with outbreaks of lesser than 100 cases, as during 1970s in Europe, when smallpox was imported in a German hospital (as many as 10 to 20 second-generation cases were often infected from a single case) [10]. Because of those properties, Smallpox is ranked among the Category A Priority Pathogens of the National Institute of Allergy and Infectious Diseases (NIAID), which is the reference scale for most of NATO member and associate states [11].
Batch availability: Following official eradication of smallpox in 1980, the remaining stocks of VARV were supposed to have been either consolidated into two maximum-containment facilities namely “Biosafety Level 4 laboratories” designated as the WHO Collaborating Centers for Smallpox and Other Poxvirus Infections, or destroyed [12]. Officially, 451 samples of smallpox virus are being held by the Center for Disease Control and Prevention (CDC) in Atlanta, Georgian USA and 120 are stored at the State Research Centre of Virology and Biotechnology (SRCVB) in Koltsovo, Siberia, Russia [13]. The CDC’s batches include samples from Britain, Japan and the Netherlands. The SRCVB’s batches include samples selected for their increased virulence and ability to become biological weapons [14].
In 2011, the WHO wondered whether the 2 known remaining USA and Russian stockpiles of smallpox virus were to be destroyed or retained [15]. The final conclusion was that to review the decision in 2014 because the USA claimed that more research was needed and the stockpiles could help prevent one of the world’s deadliest pathogens from being used as a biological weapon [16].
By the time of the eradication during the 70's, a smallpox outbreak in Aralsk, Kazakhstan demonstrated that the USSR – now the Russian Federation – was developing VARV as a strategic bioweapon despite official denegation (the USSR signed the 1972 Biological Weapons Convention) [17,18]. It is noteworthy to keep in mind that the Kazakhstan, now an independent state, is the lead of the Central Asian Union (Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan and Uzbekistan) a critical east-west and north-south trade and transport crossroads bordering regional powers such as Russia, China, and Iran. Security concerns faced by these states include mixes of “social disorder, crime, corruption, terrorism, ethnic and civil conflict, border tensions, water and transport disputes, the proliferation of weapons of mass destruction (WMD), and trafficking in illegal narcotics and persons” [19].
Rumors about undeclared smallpox stockpiles in countries like Iraq or North Korea and possibly others like China, Cuba, India, Iran, Israel, Pakistan, Syria and former Yugoslavia (now scattered into Slovenia, Macedonia, Croatia, Serbia and Montenegro, and Bosnia) have never been officially proven [20]. But the required technology to develop smallpox as an efficient bioweapon was available in the 70’s in the USSR therefore a team of 21st century post graduate student in Virology of any country can do it if the appropriate financial support is provided.
Weaponization potential and likelihood: Considering smallpox threat, the only limiting factor is to get enough virions to trigger a culture. There are many ways to achieve this. VARV is one of the largest and most complex of all viruses provided with a linear double-stranded DNA encoding over 100 genes, protected by a brick-shaped nucleocapsid surrounded by a palisade layer, which in turn is protected by an outer envelope [21]. Therefore, its ability to keep its pathogenic properties while “quiescent” in a 50-year-old dried fleck of pus is high. Recently, VACV was used as a comparator in a study designed to test Ultra Violet (UV) resistance of viruses dried onto non-porous surfaces. Results showed a significant population of virions (from 3 to 10% of virus in the inoculum) that appeared substantially protected from the effect of UV [22].
Nowadays, in order to get some smallpox virions, at least four scenarios are available:
• Wander old endemic smallpox spots in the horn of Africa (namely Djibouti, Eritrea, Ethiopia, Kenya, Somalia, and Sudan known as a major source of terrorism) hoping to find hypothetical contaminated material with quiescent virions.
• Track the different survival members of the medical teams that were involved in the last outbreaks of smallpox (US/Canada in 62, Kazakhstan in 71, India in 75 or Somalia in 77) and gather any remains from those expeditions to track quiescent virions (by that time it was common to keep dangerous remains in “secure” sealed container as a “souvenir” among healthcare professionals).
• Contact the numerous underpaid scientists and servants from the “50” sites of the former Soviet Union Biopreparat program and see what kind of material they are ready to bargain from dilapidated area of their compound (most of the time they would ignore that a rusted pipe from an old tank or that very old egg incubator may still have some quiescent virions in it).
• Attempt to bribe critical collaborators from the western and eastern authorized smallpox research facilities to get samples from their batches.
The fact that anybody reading those scenarios would spontaneously consider a differential probability for each of them demonstrates that despite the fact that they seem to be as improbable as to find a needle in a stack of hay, they may occur in the near future if not yet. It would be interesting to use Influence Diagram (ID) methodology to assess the likelihoods of those scenarios since reliable data is not available to enable a true probabilistic assessment [23].
If we take the first scenario, a group of terrorist would tediously look for abandoned village in Somalia. The group would focus on places said to have been struck by smallpox in the past. Then they would gather any remains of clothes, blankets or even cadavers buried in the ruins. Samples of those remains would be dispersed in an appropriate solution. Use of Density Gradient Ultracentrifugation would allow isolating potential virions because although invisible, their size and density would concentrate them in a known portion of the centrifugation tube. An aliquot of the known portion of the centrifugation tube would then be placed in a portable PCR system. This system allows duplicating any trace of DNA to such an extent that the resulting amount authorizes any kind of analysis. Appropriate Smallpox DNA probes would then tell the terrorists, whether the remains contain the desired virions or not. Terrorists would be able to achieve this task because nobody would dare to ask what those guys are doing in ruins of a ghost town nowhere in Somalia with some lab equipment and a generator to run the whole. As soon as some smallpox virions are isolated, it is very simple to start a replication process with the standard procedure of Embryonated Hen (or Chicken) Eggs that any postgraduate student in microbiology is supposed to be familiar with. Egg culture is a standard virus culture method used for many vaccine productions. Development of smallpox bioweapons in the 20th century used egg culture as a way to produce massive amounts of virions in batches.
All the terrorists have to do is to inoculate hundreds of eggs with more aliquots (at this step, they don’t need to bother about hygiene because they do not intend to grow a harmless vaccine and because the gradient density ultra centrifugation is both a thorough and reproducible process). The only tricky step is to inoculate the chorioallantoic membrane of the embryonated egg to optimise VARV replication. Incubators are standard laboratory equipment and can be purchased on the Internet. Further steps such as purification of virus batches are described in good practice manuals of the pharmaceutical industry [24]. In fact, there is a book available for less than 40 Euro at the Springer website that covers anything needed to grow smallpox: “Working Safely with Vaccinia Virus: Laboratory Technique and Review of Published Cases of Accidental Laboratory Infections) [25]. From the terrorist stand point; you don’t need a Biosafety Level 4 laboratory or a secret Bunker like those of the Pokrov Biologics Plant to produce your bioweapon because human loss among servants is part of the payload to reach their goal.
The weaponization of the produced batches of smallpox is not a difficult task either. During the 18th century, British forces distributed smallpox-infected blankets to Native American tribes in Ottawa who lacked any degree of immunity to it [26]. The most rustic yet efficient way would be to use some spray bottle with or without fans and suggest to some volunteers to disseminate the content in a crowded place acting as a crossroad (public area of an airport, train station, discotheque, etc.) during a heat wave. Another option would be to contaminate some fabric ready for export. Volunteers would certainly die in the process but this would grant them with the socially rewarding “martyr” status among their peers.
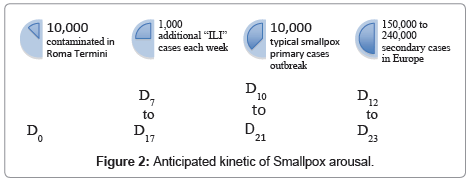
A reasonable scenario of smallpox introduction and dissemination (Figure 1) could take place at Roma Termini (Rome’s central train station), frequented by approximately 480,000 persons per day (20,000 per hour) that is linked every 30 minutes with Rome Fiumicino Airport, frequented by approximately 80,000 persons per day (3,300 per hour) by the Leonardo Express, which owns a seating capacity for 300 passengers (600 per hour). During early July for example, some people may sell small spray bottles of apparently crystal water to help tourist coping with the heat wave. In fact bottles would contain a solution of smallpox virions. Hundreds of tourists about to visit Roma or on their way back home would thus unwillingly spread this solution on their face, their children/friends and the crowd surrounding them. In a single day, hundreds of tourists would have sprayed the solution within the Leonardo Express confined atmosphere as well. At the end of the day, as much as 10,000 people would have been contaminated on their way to the airport. Around 3,000 would have come back to Madrid (Spain), 2,500 to Paris-CDG (France), 2,000 to London-Heathrow (United Kingdom), 1,500 to Amsterdam (Netherlands), 1,000 to Frankfurt am Main (Germany) and 1,000 to Brussels (Belgium), not counting the contaminated that stayed in Italy. During the next 7–17 days nothing would happen (incubation period). Serious things would start with the onset of the febrile phase that last 3-4 days (fever can spike upwards of 39°C and may include myalgia, headache, vomiting, and prostration) for all of the thousands of infected people wherever their living place in Europe. Nothing distinguish this fever from an Influenza Like Illness (ILI), which includes the common cold and influenza. Therefore, most of the infected people stay home and or get acetaminophen from their GP. During week 30 (late July), there can be up to 70,000 cases of ILI in a given country (e.g. UK) [27]. The 2,000 additional cases linked to smallpox are responsible for a 2% increase only (doubtfully detectable at this step, figures are the same for the other countries). During this dissemination phase, infected people can easily contaminate both their private and professional contacts. A recent empirical study regarding the pattern, number and duration of contacts between individuals within a social group (face-to-face) reveals that the mean number of contact per day for an individual is 30 with a mean cumulated duration of the interaction between two individuals of 2 minutes. The fraction of repeated contacts in the second day with respect to the first is 12%. With such conditions, outbreaks tend to be explosive (attack rate between 51% and 80%) [28]. In other words, the 2,000 smallpox primary cases – still unknown from the UK health authorities – can contaminate between 51% and 80% of their 30 contacts per day i.e. the 2,000 UK smallpox primary cases are likely to generate 30,000 to 48,000 additional secondary cases before the first centrifugally distributed, systemic rash occurs. Hopefully, by that time the number of rash would intrigue doctors in hospitals and trigger the regional Diagnosis and Response Team. Back to the 10,000 infected people from Roma Termini, they are likely to generate an overall 150,000 to 240,000 additional cases outside Italy (Figure 2). From that point, available smallpox outbreak models make sense and can help decision makers [29,30]. Unfortunately those cases will occur at random within the time frame anywhere within the targeted countries. When intriguing rashes and possibly pustules occur (at D10 at the earliest), microbiologists start sending samples to the reference centre most likely by post mail (expect 2 to 3 days for samples to reach reference centre then additional 12-24 hours to get official confirmation, thus smallpox response plan are likely to be triggered not earlier than D13). Identifying the initial spot and all the contact persons all around Europe is going to be a nightmare for health authority officers. Indeed, if any fever and/or ILI syndrome would benefit from random smallpox screening in Europe, chances are that we detect the attack at an early stage thus maximizing containment.
Limitation of experts’ opinion: Thus WHO experts’ statement such as “it is unlikely that terrorists would resort to smallpox in a biological attack” because “they are just not capable of doing this stuff” is simply irresponsible. Even if said by a Canadian smallpox expert who was part of the WHO team that inspected both the CDC and SRCVB Biosafety Level 4 laboratories [31]. Following the same logic, a recent thesis published in the USA by the Naval Post Graduate School concludes, “Terrorists are unlikely to be able to master the acquisition, production, weaponization and dissemination of the virus, and would likely pursue other types of weapons” [32]. This statement again misses the fact that terrorists don’t need to reach NATO STANAGs when it comes to the design and operability of bioweapons because they don’t really care about the servants.
More threats: VARV is not the only threat because otherstrains of orthopoxviridae can infect humans such as the Monkeypox virus (MPXV), which is considered as the most significant human public health threat in the genus Orthopoxvirus since the eradication of variola virus: in 2003, MPXV caused an outbreak in the United States due to the importation of infected African rodents, and subsequent sequential infection of humans [33]. The same year – 2003 – pattern of sustained human-to-human transmission was observed in the Republic of Congo. Up to six sequential transmissions of MPXV from person to person have occurred, making this the longest uninterrupted chain of human Monkeypox fully documented to date [34].
Thus the problem is not “whether terrorists – or so called “rogue countries” – will get a smallpox bioweapon or not” but rather “will we have the ability to elicit the appropriate response on time to minimize the death toll and other public health impact as well as social/political consequence”.
Risk management
Doctrine comes first: Appropriate response calls for relevant doctrine. Therefore, many expert groups from several industrialized countries, like the USA Civilian Biodefense initiative, have elicited specific consensus guidelines which encompasses early detection, isolation of infected individuals, surveillance of contacts, therapy, post exposure isolation and infection control, hospital epidemiology and infection control, home care, decontamination of the environment, and a focused selective vaccination program in the event of an actual outbreak of smallpox and subsequent epidemic [35].
Early detection is key: Early detection is the critical entry point of the response. It is in the hands of the Regional Smallpox Diagnosis and Response Group (RSDRG) in the UK, the Centre National de Crise (CNC) in France, the CDCs in the US, and so on (each NATO member states has his own Diagnosis and Response Team). Unfortunately, in most of Smallpox response plan, the early detection part is often minimalistic and epidemiologic diagnostic criteria as well as threshold parameters to elicit response plan are insufficiently developed. Indeed, since smallpox no longer occurs naturally, a single confirmed case should prompt implementation of smallpox response plans. But what is the “cost” of this first confirmed case?
Moreover, despite improvements in the past decade, public health surveillance, hence, Diagnosis and Response Teams, capabilities to achieve early detection, remain limited and fragmented. When WHO claims that it “monitors and verifies all rumours of smallpox through its epidemic intelligence activities within its global alert and response operations”, it is rather incantatory because essentially it is the Diagnosis and Response Teams that nurture WHO [36].
The situation should improve thanks to new technological and conceptual advances that are currently addressing this issue. Such advances were elicited by the revised International Health Regulations (IHR 2005) and other initiatives, including ProMED-mail, Health Map, the Global Public Health Intelligence Network (GPHIN), WHO global outbreak alert and response network (GOARN), Global emerging infections system (GEIS), the national electronic disease surveillance system (NEDSS), all allowing the use of new data sources and methods to improve global coverage, sensitivity, and timeliness. In addition, the Emerging Pandemic Threats (EPT) program, which includes the PREDICT project is building global capacity for surveillance of infections that have pandemic potential as well as elaborating a framework for risk assessment [37].
Early detection is challenging: Whatever the provided tools, all of those Diagnosis and Response Teams are facing a rather challenging syndromic surveillance based on a subtle signal/noise discrimination process: ideally they have to be able to identify unexpected peak of fever over numerous ones–in other words to distinguish potential smallpox symptoms among numerous naturally occurring influenza like symptoms (which are basically the same)–then to monitor every suspected patients during more than 4 days to check whether any systemic rash occur. Even in the occurrence of such a rash, there is still little chance to be certain that a smallpox outbreak is on its way from neither the clinical presentation nor the epidemiologic kinetic. Pathogen identification tests should then be performed if not already done to assert whether VARV is responsible for the symptoms because it would be devastating to wait for another 7 days to see the first pustules before triggering the response program (patients start to actively contaminate those they encounter as soon as the fever rises).
WHO is assisting those Diagnosis and Response Teams “by directing them to the most appropriate and convenient laboratory for diagnosis of suspected smallpox infections, using the network of WHO Collaborating Centers as well as other laboratories”. This statement is again rather incantatory because early detection of VARV in the field is extremely complex and addresses at least 3 key questions in a practical project [38]:
1. Will the virions that originated from one or a very few infected persons be recovered and detected?
2. Will the presence of antibodies in the starting samples against most known viruses affect the detection?
3. Can this process be carried out rapidly enough to support a timely therapeutic or prophylactic response?
To routinely detect a potential outbreak of smallpox, Diagnosis and Response Teams need to have completely automated and contained laboratories that continually search for and sequence viruses from a wide variety of sources. This implies to continuous honing of skills, demonstrate efficiency and develop improved systems, methods and reagents [39]. Indeed those automated and contained laboratories are useless without routine random sample collection of serum in emergency wards taking care of “fever” or “Influenza like Illnesses”.
The standard method for detecting VARV is to titrate in the serum neutralizing antibodies produced by the immune responses. A test that is specific but also time-consuming and laborious. Therefore, combination of a rapid, sensitive, high-throughput assays allowing large-scale use with its related statistical method involved in analysing the large quantity of data generated are developed [40]. A “T cell-driven” methodology based on the specificity of the lymphocyte T cell response upon infection by VARV is developed too [41]. Another option is to detect viral genetic material itself (measure of mRNA transcription for example) as a marker for actively replicating VARV using real-time PCR [42].
Trying to identify smallpox virions before they contaminate individuals is not easy either. Screening substances (powder, liquids, aerosols) with unknown potentials for biological threat question the speed, sensitivity, and reliability – including influence by different common household products present in the environment – of diagnostic methods such as real-time PCR, electron microscopy, and virus isolation tests. Thus, a positive result obtained by any one of these techniques as to be followed by a biological method to confirm the putative diagnosis. Confirmatory methods include virus isolation followed by an agent-specific immunofluorescence assay to confirm the presence of replication-competent virions [43]. Again, it is a time consuming process with limited reactivity (expect 2 to 4 days to achieve task).
Containment strategy
Nevertheless, it is of utmost importance to maintain a comprehensive defense strategy to counter the anticipated “low-probability”, high-impact threat of smallpox, as well as the on-going threat of naturally occurring poxviridae diseases. The most relevant primary strategy to control any smallpox outbreak is containment (or ring vaccination). In addition, some health authorities recommend that, in the event of an outbreak, at the national or regional level, local health departments apply plans to allow rapid vaccination of their populations within 10 days, as an adjunct to ring vaccination. Ten days is the period chosen because the 7-17 days incubation period of smallpox is usually more of about 12–14 days. Therefore, completing vaccination of the public within 10 days would permit vaccination of most persons within the incubation period of the first generation of cases, limiting the second generation of cases, and preventing a third generation of cases [44].
After eradication, VACV has been reserved for select populations who might be at significant risk for poxviridae infections [45]. Substantial animal and limited human data suggest that second and third generation smallpox vaccines, specifically tissue-cultured VACV and replication-competent, highly attenuated VACV possess immunogenicity and surrogate efficacy profiles similar to those of first generation [46]. The currently licensed live-virus smallpox vaccine ACAM2000 from Sanofi is effective, but associated with serious and even life-threatening adverse events such as postvaccinial encephalitis, encephalomyelitis, encephalopathy, progressive vaccinia (vaccinianecrosum) and eczema vaccinatum. Severe disability, permanent neurological sequelae, and/or death may occur at a rate of approximately 1 death per million primary vaccinations and 1 death per 4 million revaccinations. Death has also occurred in unvaccinated contacts of vaccinated persons [47]. The health threat posed by this vaccine, and other previously licensed vaccines that are still stored in strategic stockpiles, limits their use among the general population to the response of a documented outbreak. Replication-defective, attenuated VACV may have utility as a priming agent in those with contraindications to live VACV. As an example, the Modified Vaccinia Ankara (MVA) is one of such attenuated VACV candidates [48].
Another option is to avoid vaccines containing live virus (even attenuated) and to focus on so called subunit vaccines which target specific viral proteins [49]. Those novel subunit/component vaccines may play roles in unconventional strategies to defend against smallpox used as a weapon of mass destruction [50]. Type I interferon-binding protein is a major virulence factor in smallpox animal models; vaccination with this protein induces protective immunity (its neutralization prevents disease progression as well) [51]. A candidate DNA-based subunit vaccine, termed “4pox”, targets four viral structural components [52].
Whatever the vaccine, the route of administration has a critical implication for massive vaccination programs in a limited time. Five different routes of vaccination are available including intramuscular, intranasal, oral, mucosal and subcutaneous inoculations. Among those the mucosal inoculation seems the most attractive but it is the subcutaneous which is currently the standard one [53].
Treatment strategy: When a smallpox case is declared then vaccination is of little help except for those infected who are within four days after exposure to the virus. Therefore, treatments for smallpox focus on providing relief of symptoms with supportive care:
1. Medications to control fever and pain.
2. Intravenous fluids to compensate dehydration and electrolyte loss from sweating.
3. Good nursing care of pustules.
4. Antibiotics to prevent secondary infections from bacteria.
On the other hand, non-vaccine compounds can prevent cellular infection from VARV with minimal cytotoxicity. An interesting compound expresses a disruptive action against the VACV “processivity” complex (comprising proteins that enable the viral DNA polymerase to synthesize extended strands) thus halting the replication process [54].
Currently, the therapeutic option for the treatment of poxvirus infections relies on the broad-spectrum viro static nulceosid analogcid of ovir– active against virtually all DNA viruses– which has been proven to be more effective than “curative” smallpox vaccination in an animal model based on MPXV infection [55]. Cidofoviris, therefore, is considered very effective in the therapy and short-term prophylaxis of smallpox and related poxvirus infections in humans, as well as the treatment of the complications that may arise in immunocom promised patients inadvertently inoculated with VACV [56]. Cidofoviris addresses only one step of the viral replication cycle. A good understanding of poxvirus pathogenesis raises the possibility to explore other appropriate targets within the cycle. Gefitinib, for instance, known as an anti-tumour therapy, demonstrates the ability to inhibit the process that facilitate virus spreading among the cells of the infected individuals. This property may provide a new therapeutic option for single or combination therapy of acute VACV infections, while reducing the risk of viral resistance to treatment [57].
The protease inhibitor with orphan drug status ST-246 is being evaluated as a treatment for pathogenic poxviridae infections in humans. Results from phase II, double blind, randomized, placebo-controlled, multicentre trial support further testing in a multicentre pivotal clinical safety study for licensure application [58].
Conclusion
Past experiences with outbreaks of anthrax, severe acute respiratory syndrome, avian flu and monkey pox demonstrate that intentional or naturally occurring outbreaks require the same combination of electronic health information networks, Strategic National Stockpile, strengthened relationships between the practice and academic communities and increased cooperation among all the actors of the response plans despite expanded lines of reporting and unremitting inflows of new guidance documents.
Beyond its not so controversial risk assessment, the specific situational analysis of smallpox threat makes it a perfect model to sharpen national public health emergency response capability against bioterrorism and pandemic threats from the early detection down to the treatment of casualties. Without such treatments rapid agent identification is not necessary, but without such identification no pressing political/commercial justification for developing specific antiviral agents exists, because they will be perceived as useless. To be successful, diagnosis and therapy must be linked.
Whatever the likelihood of smallpox weaponization is, Al-Qaeda terrorists and alike obviously favour indiscriminate slaughter and Smallpox offer a convenient way to respond to this inclination. Strikingly, the “historical birthplace” of Smallpox is located within the Sumer and its pre-Islamic gods’ territory. “Erra”, for instance, was the Sumerian “god of indiscriminate slaughter” also known as the “god of war and pestilence” (thus linked to epidemic threat) [59]. Some Sumerian gods were later incorporated in the Islamic demonology. In other words, from a sociological/theological standpoint, should Al-Qaeda terrorists and alike use smallpox for slaughtering people? They would, in fact, as a paradox, behave as worshippers of their own demons while pretending/believing to serve their God.
References
- Hopkins DR (2002) Chicago: University of Chicago Press, The Greatest Killer: Smallpox in History.
- Li Y, Carroll DS, Gardner SN, Walsh MC, Vitalis EA, et al. (2007) On the origin of smallpox: correlating variola phylogenics with historical smallpox records. Proc Natl Acad Sci USA 104: 15787-15792.
- Shchelkunov SN (2009) How long ago did smallpox virus emerge? Arch Virol 154: 1865-1871.
- Fenner F (1982) A successful eradication campaign. Global eradication of smallpox. Rev Infect Dis 4: 916-930.
- Fenner F, Henderson DA, Arista I, Jezek Z, Ladnyi ID (1988) Smallpox and Its Eradication. Communicable Disease Surveillance and Response. The clinical features of smallpox 1-68.
- Wahl-Jensen V, Cann JA, Rubins KH, Huggins JW, Fisher RW, et al. (2011) Progression of pathogenic events in cynomolgus macaques infected with variola virus. PLoS One 6: e24832.
- https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_pjanind&lang=en
- https://2010.census.gov/news/releases/operations/cb11-cn147.html
- HARPER GJ (1961) Airborne micro-organisms: survival tests with four viruses. J Hyg (Lond) 59: 479-486.
- Wehrle PF, Posch J, Richter KH, Henderson DA (1970) An airborne outbreak of smallpox in a German hospital and its significance with respect to other recent outbreaks in Europe. Bull World Health Organ 43: 669-679.
- topics/biodefenserelated/biodefense/pages/cata.aspx
- Damon I (2007) Poxviruses. Fields Virology. (5thedn), Lippincott Williams & Wilkins, New York 2948-2975.
- WHO Advisory Committee on Variola Virus Research (2007). WHO report of the ninth meeting, Geneva, Switzerland 29-30.
- Weinstein RS (2011) Should remaining stockpiles of smallpox virus (variola) be destroyed? Emerg Infect Dis 17: 681-683.
- Henderson DA (2011) Smallpox virus destruction and the implications of a new vaccine. Biosecur Bioterror 9: 163-168.
- https://www.cbsnews.com/8301-504763_162-20065775-10391704.html
- Henderson DA, Inglesby TV, Bartlett JG, Ascher MS, Eitzen E, et al. (1999) Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA 281: 2127-2137.
- Zelicoff AP (2003) An epidemiological analysis of the 1971 smallpox outbreak in Aralsk, Kazakhstan. Crit Rev Microbiol 29: 97-108.
- Nichol J (2010) Central Asia’s Security: issues and implications for US interests. Congressional Research Service.
- Koblentz G (2003) Assessing the Proliferation of Smallpox. Security Studies Program Massachusetts Institute of Technology. ESDP-Lincoln Lab Conference.
- Dulbecco R, Ginsberg HS (1988) Virology (2ndedn), Philadelphia: J.B. Lippincott Company 179-191.
- Sagripanti JL, Lytle CD (2011) Sensitivity to ultraviolet radiation of Lassa, vaccinia, and Ebola viruses dried on surfaces. Arch Virol 156: 489-494.
- Gaudioso J, Brooks T, Furukawa K, Lavanchy DO, Friedman D, et al. (2011) Likelihood of Smallpox Recurrence. J Bioterr Biodef.
- https://www.ifpma.org/resources/influenza-vaccines/influenza-vaccines/vaccine-manufacture-virus-processing.html
- https://www.springerlink.com/content/m5517x173u133478/#section=1082729&page=1
- Jaskoski H (1996) A Terrible Sickness Among Them: Smallpox and Stories of the Frontier. Early Native American Writing: New Critical Essays. Cambridge University Press.
- Tilston NL, Eames KT, Paolotti D, Ealden T, Edmunds WJ (2010) Internet-based surveillance of Influenza-like-illness in the UK during the 2009 H1N1 influenza pandemic. BMC Public Health 10: 650.
- Stehlé J, Voirin N, Barrat A, Cattuto C, Colizza V, et al. (2011) Simulation of an SEIR infectious disease model on the dynamic contact network of conference attendees. BMC Med 9: 87.
- Aldis GK, Roberts MG (2005) An integral equation model for the control of a smallpox outbreak. Math Biosci 195: 1-22.
- Burke DS, Epstein JM, Cummings DA, Parker JI, Cline KC, et al. (2006) Individual-based computational modeling of smallpox epidemic control strategies. Acad Emerg Med 13: 1142-1149.
- https://www.mmi.med.ualberta.ca/staff_students/david_evans.php
- Musson GC (2011) Smallpox as a Bioweapon Should We Be Concerned. Thesis Collection 2012.
- Hutson CL, Carroll DS, Gallardo-Romero N, Weiss S, Clemmons C, et al. (2011) Monkeypox disease transmission in an experimental setting: prairie dog animal model. PLoS One 6: e28295.
- Learned LA, Reynolds MG, Wassa DW, Li Y, Olson VA, et al. (2005) Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo, 2003. Am J Trop Med Hyg 73: 428-434.
- https://www.who.int/csr/disease/smallpox/preparedness/en/index.html
- Morse SS (2012) Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 10: 6-16.
- Anderson NG, Gerin JL, Anderson NL (2003) Global screening for human viral pathogens. Emerg Infect Dis 9: 768-774.
- Okonko IO, Ojezele MO, Babalola ET, Nwanze JC, Mejeha OK, et al. (2011) Emerging infections and bioterrorism emergencies: Where do we go from here? Biotechnology and Molecular Biology Reviews 6: 21-30.
- Kennedy R, Pankratz VS, Swanson E, Watson D, Golding H, et al. (2009) Statistical approach to estimate vaccinia-specific neutralizing antibody titers using a high-throughput assay. Clin Vaccine Immunol 16: 1105-1112.
- Judkowski V, Bunying A, Ge F, Appel JR, Law K, et al. (2011) GM-CSF production allows the identification of immunoprevalent antigens recognized by human CD4+ T cells following smallpox vaccination. PLoS One 6: e24091.
- Kramski M, Drozd A, Lichtfuss GF, Dabrowski PW, Ellerbrok H (2011) Rapid detection of anti-Vaccinia virus neutralizing antibodies. Virol J 8: 139.
- Kurth A, Achenbach J, Miller L, Mackay IM, Pauli G, et al. (2008) Orthopoxvirus detection in environmental specimens during suspected bioterror attacks: inhibitory influences of common household products. Appl Environ Microbiol 74: 32-37.
- Strikas RA, Neff LJ, Rotz L, Cono J, Knutson D, et al. (2008) US Civilian Smallpox Preparedness and Response Program, 2003. Clin Infect Dis 3: S157-S167.
- Walsh SR, Dolin R (2011) Vaccinia viruses: vaccines against smallpox and vectors against infectious diseases and tumors. Expert Rev Vaccines 10: 1221-1240.
- Artenstein AW (2008) New generation smallpox vaccines: a review of preclinical and clinical data. Rev Med Virol 18: 217-231.
- https://www.drugs.com/sfx/acam2000-side-effects.html
- McCurdy LH, Larkin BD, Martin JE, Graham BS (2004) Modified vaccinia Ankara: potential as an alternative smallpox vaccine. Clin Infect Dis 38: 1749-1753.
- Kennedy RB, Poland GA (2010) The identification of HLA class II-restricted T cell epitopes to vaccinia virus membrane proteins. Virology 408: 232-240.
- Golden JW, Hooper JW (2011) The strategic use of novel smallpox vaccines in the post-eradication world. Expert Rev Vaccines 10: 1021-1035.
- Fernández de Marco Mdel M, Alejo A, Hudson P, Damon IK, et al. (2010) The highly virulent variola and monkeypox viruses express secreted inhibitors of type I interferon. FASEB J 24: 1479-1488.
- Golden JW, Hooper JW (2010) Evaluating the orthopoxvirus type I interferon-binding molecule as a vaccine target in the vaccinia virus intranasal murine challenge model. Clin Vaccine Immunol 17: 1656-1665.
- Lu B, Yu W, Huang X, Wang H, Liu L, et al. (2011) Mucosal immunization induces a higher level of lasting neutralizing antibody response in mice by a replication-competent smallpox vaccine: vaccinia Tiantan strain. J Biomed Biotechnol.
- Nuth M, Huang L, Saw YL, Schormann N, Chattopadhyay D, et al. (2011) Identification of inhibitors that block vaccinia virus infection by targeting the DNA synthesis processivity factor D4. J Med Chem 54: 3260-3267.
- Stittelaar KJ, Neyts J, Naesens L, van Amerongen G, van Lavieren RF, et al. (2006) Antiviral treatment is more effective than smallpox vaccination upon lethal monkeypox virus infection. Nature 439: 745-748.
- De Clercq E (2002) Cidofovir in the treatment of poxvirus infections. Antiviral Res 55: 1-13.
- Langhammer S, Koban R, Yue C, Ellerbrok H (2011) Inhibition of poxvirus spreading by the anti-tumor drug Gefitinib (Iressa). Antiviral Res 89: 64-70.
- Chinsangaram J, Honeychurch KM, Tyavanagimatt SR, Leeds JM, Bolken TC, et al (2012) Safety and Pharmacokinetics of the Anti-Orthopoxvirus Compound ST-246 following a Single Daily Oral Dose for 14 Days in Human Volunteers. Antimicrob Agents Chemother 56: 4900-4905.
- Antimicrob. Agents Chemother. AAC.00904-12; published ahead of print 9 July 2012
- https://www.britannica.com/EBchecked/topic/191889/Erra
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 16159
- [From(publication date):
specialissue-2012 - Sep 29, 2025] - Breakdown by view type
- HTML page views : 11473
- PDF downloads : 4686