Research Article Open Access
Sexually Transmitted Diseases: Management by Urology, Emergency Medicine and Obstetrician/Gynecology Physicians does not Generally Follow CDC Guidelines
Weigler G, Perry C, Weigler A, Kim B, Yangouyian M, Vicena J and Richard Santucci*
Detroit Medical Center, Michigan State University College of Osteopathic Medicine, Michigan, USA
- *Corresponding Author:
- Richard Santucci
Specialist-in-Chief, Urology
Detroit Medical Center, Clinical Professor
Michigan State University College of Osteopathic Medicine
4160 John R. Suite 1017, Detroit, Michigan 48201, USA
Tel: 313-745-4123
Fax: 313-745-8222
E-mail: rsantucc@dmc.org
Received date: August 14, 2013; Accepted date: October 15, 2013; Published date: October 17, 2013
Citation: Weigler G, Perry C, Weigler A, Kim B, Yangouyian M, et al. (2013) Sexually Transmitted Diseases: Management by Urology, Emergency Medicine and Obstetrician/Gynecology Physicians does not Generally Follow CDC Guidelines. J Community Med Health Educ 3:244. doi:10.4172/2161-0711.1000244.
Copyright: © 2013 Weigler G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Aim: This study was designed to determine the practice habits of physicians in reporting and treating sexually transmitted diseases (STDs), which infect an estimated 15 million people each year in the United States. We hypothesize a variance in how STDs are treated among different medical specialties and the rate of adherence to CDC guidelines. Methods: Prospective study querying 125 physicians regarding STD treatment habits. Seven-question surveys were distributed among urology, ob/gyn, and emergency medicine attending and resident physicians. Results: Of the questionnaires circulated, 76 (61%) were completed. Resident physician response (87%) was higher than attending physician response (13%). 100% of EM and 85% of urology doctors administer empiric STD medications based on history and physical exam findings alone, while most obstetrician/gynecologists (62%) wait for positive cultures prior to treatment. Most physicians do not treat partners of the index patient (ob/gyn 69%, Urology 55%, EM 73%). Reasons for not treating partners were varied and included: follow up, allergies, concerns of medicolegal recourse, time, and loss of revenue and office resources. Finally, while most physicians were concerned about follow-up care, there was no consistency in follow up plans. Conclusion: Our study showed physicians vary greatly in treating and managing STDs. Despite published guidelines by the Center for Disease Control (CDC) specifying an appropriate treatment course for the index patient and their partner, the majority of physicians do not follow these CDC guidelines. This may be creating a quality of care problem for millions of American patients affected by STDs annually.
Keywords
Sexually transmitted diseases; Patient delivered partner therapy; Expedited partner therapy; Center for disease control
Introduction
STDs affect about 15 million people every year in the United States. They have serious long-term consequences including pelvic inflammatory disease, infertility, ectopic pregnancy, salpingitis, and perinatal infections [1,2]. Adolescents have the highest rates of STDs because of a higher number of sexual contacts and lower rates of condom use [3]. CDC data from 2011 estimates that even though young people aged 15-24 represent only 25% of the sexually experienced population, they acquire 50% of all new STDs.
It is important to diagnose STDs early and implement proper treatment to belay the natural sequelae of associated morbidities. Proper treatment involves more than just prescribing the correct antibiotic to the concerned patient. The CDC Sexually Transmitted Diseases Treatment Guidelines suggest five strategies for the “prevention and control” of STDs: “1) education and counseling of persons at risk on ways to avoid STDs through changes in sexual behaviors; 2) identification of asymptomatically infected persons and of symptomatic persons unlikely to seek diagnostic and treatment services; 3) effective diagnosis and treatment of infected persons; 4) evaluation, treatment, and counseling of sex partners of persons who are infected with a STD; and 5) pre-exposure vaccination of persons at risk for vaccine-preventable STDs [4].”
Our group previously investigated sexually active women presenting to the emergency department and found that a significant percentage had undiagnosed STDs [2]. Following the conclusion of that study, our institute became interested in the approach specialty physicians take in treating STDs in the infected patient, partner(s), and the follow up care of these patients. The authors of this study hypothesized there would be a wide spectrum of approaches, and suboptimal adherence to published treatment guidelines.
Methods
One hundred twenty five physicians were queried about their practice styles in respect to sexually transmitted diseases. Surveys (Appendix 1) were collected from 27 urology, 35 obstetrics/gynecology (OB/Gyn), and 14 emergency medicine (EM) attending and resident physicians. Physicians selected are members of the Michigan State University College of Osteopathic Medicine Post Graduate Training Institution (MSU-OPTI), composed of 20 member hospitals and two academic centers. Surveys were administered by paper questionnaires that were disseminated to the specialty audience and then collected at consecutive MSU-OPTI meetings. Participation was voluntary and anonymous. Student’s t test and chi square testing were used to analyze our data utilizing SPSS software.
Results
125 surveys were distributed at consecutive MSU-OPTI meetings. Seventy six or 61% of the surveys were returned for use in data collection. Resident physicians completed 87% of the returned surveys (Table 1). Table 1 also shows the training level of the respondents and the composition of respondents by specialty. In the ob/gyn, urology and EM group 100%, 70% and 85% of the responders were resident physicians. The group was composed primarily of ob/gyn physicians followed by urology and EM with the valid percents being 46, 36 and 18. It was only within the ob/gyn group that there were significant statistical variations in responses based on training year in residency (p 0.03 and 0.04) (Table 3, q3, q5-1).
| Level of Training | Urology | OB/GYN | EM | Total |
|---|---|---|---|---|
| PGY-1 | 0 | 11 | 4 | |
| PGY-2 | 1 | 9 | 4 | |
| PGY-3 | 5 | 9 | 1 | |
| PGY-4 | 5 | 6 | 3 | |
| PGY-5 | 3 | N/A | N/A | |
| PGY-6 | 3 | N/A | N/A | |
| PGY-7 | 1 | N/A | N/A | |
| No Response | 1 | N/A | N/A | |
| Total Residents | 19 | 35 | 12 | 66 |
| Attending (0-5 years) | 1 | 0 | 0 | |
| 6-10 years | 1 | 0 | 0 | |
| 10 + years | 6 | 0 | 2 | |
| Total Attending | 8 | 0 | 2 | 10 |
| Total/Frequency | 27 | 35 | 14 | 76 |
| Percent | 35.5 | 46.1 | 18.4 | 100 |
| Valid Percent | 35.5 | 46.1 | 18.4 | 100 |
| Cumulative Percent | 35.5 | 81.6 | 100 |
Table 1: Demographics of study participants.
All of the emergency physicians and most urologists (85%) administer empiric STD medication based on their historical and physical findings prior to culture results. This differs from 62% of ob/gyn physicians who wait on a positive culture prior to instituting treatment. Within the ob/gyn specialty there was a significant difference in response to item 3 in Appendix 1 in regards to administering empiric STD medication (p value 0.03) (Table 2, q3).
| Chi square test, p values shown | |||||||
|---|---|---|---|---|---|---|---|
| Difference between specialty | Difference between Res Yr for each specialty | ||||||
| Ob/Gyn | Urol | EM | Ob/Gyn | Urol | EM | ||
| q3 | 0.03 | 0.22 | q3 | 0.03 | 0.22 | ||
| q4 | 0.69 | 0.63 | 0.37 | q4 | 0.69 | 0.63 | 0.37 |
| q5-1 | 0.04 | 0.41 | 0.52 | q5-1 | 0.04 | 0.41 | 0.52 |
| q5-2 | 0.94 | 0.57 | 0.22 | q5-2 | 0.94 | 0.57 | 0.22 |
| q5-3 | 0.95 | 0.24 | 0.10 | q5-3 | 0.95 | 0.24 | 0.10 |
| q5-4 | 0.54 | q5-4 | 0.54 | ||||
| q5-5 | 0.40 | 0.35 | q5-5 | 0.40 | 0.35 | ||
| q5-6 | 0.68 | q5-6 | 0.68 | ||||
| q6-1 | 0.49 | 0.22 | q6-1 | 0.49 | 0.22 | ||
| q6-2 | 0.70 | 0.90 | q6-2 | 0.70 | 0.90 | ||
| q6-3 | 0.40 | 0.76 | q6-3 | 0.40 | 0.76 | ||
| q6-4 | 0.41 | 0.22 | q6-4 | 0.41 | 0.22 | ||
| Indicates a significant difference between specialties | |||||||
| Indicates a significant difference between resident training within the specialty | |||||||
| blank cells indicate all answered the same, i.e., there is no difference, so Chi square can't be calculated | |||||||
Table 2: Significant response variation based on specialty and level of training using SPSS software.
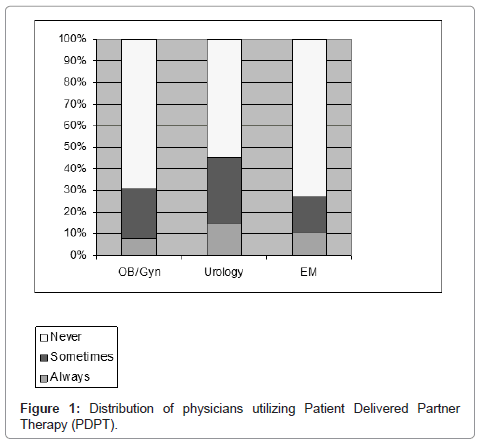
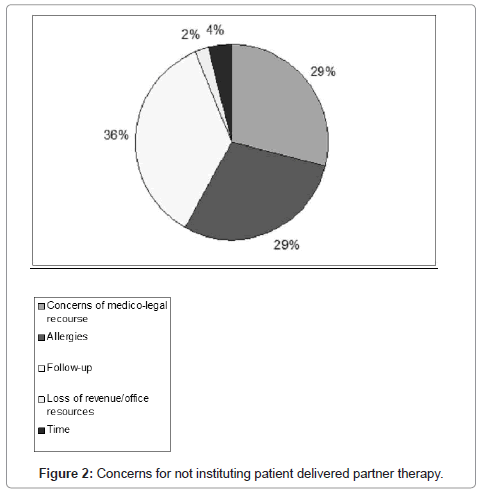
The majority of physicians - 55% urologists, 69% ob/gyn physicians, and 73% of EM physicians-do not initiate patient delivered partner therapy (PDPT) (Figure 1). Barriers to delivery of PDPT were various and related to concerns surrounding adequate follow-up, medico-legal recourse, and drug allergies (Figure 2). The only statistically significant variation was among the ob/gyn group with a p value of 0.04 in regards to item 5 from Appendix 1 (Table 2, q5-1).
Almost all physicians responding were concerned about continuity of care in the form of follow-up. However, how this was handled varied based on the specialty (Table 3). Most urologists reevaluated symptoms and physical exam; 76% of ob/gyns preferred to reculture the patient. EM physicians, because of the nature of their practice, opted to refer to the patient’s primary care physician.
| OB/Gyn | Urology | EM | |
|---|---|---|---|
| None | 0 | 7 | 16 |
| Symptom Recheck and Physical Reevaluation | 24 | 62 | 3 |
| Reculture | 76 | 28 | 0 |
| Referral to Another Physician | 0 | 3 | 81 |
Table 3: Percentage of physician’s follow-up routine.
Discussion
These data support the hypothesis that there is poor partner treatment and continuity of care in patients affected and at risk of STDs. Furthermore, not only are the standards lacking amongst specialty colleges in their approach to STD treatment, but there are significant deviations from the suggested treatment of STDs.
Observational and randomized, controlled trials have shown that PDPT is associated with a decreased risk of reinfection in women, a reduced occurrence of persistent or recurrent infections, and a trend toward a decreased morbidity [5-9]. A recent survey showed a correlation between the severity of symptoms in Chronic Pelvic Pain Syndrome (CPPS) with evidence of past and present Chlamydia infection. It is suggested in the survey that antimicrobial treatment and Chlamydia eradication may prevent the development of CPPS in some men, further emphasizing the crucial need to treat STDs and initiate PDPT [10,11].
In one of the few similar studies ever done on a national level, Patient-delivered therapy for sexually transmitted diseases as practiced by U.S. physicians [9]. Sex Transm Dis 32:101-105, 2005 demonstrated similar results; 50% and 44% of respondents in this study never instituted PDPT in gonorrhea or chlamydial infections, respectively, and less than 10% always treated the partner.
In the CDC’s Sexually Transmitted Diseases Treatment Guidelines, 2010, clinical and behavioral outcomes of available studies were integrated and the compilation of data showed that Enhanced Partner Therapy (EPT) was proven to be a useful option to facilitate partner management [10]. The CDC recommends that each case be handled on an individual basis but that every effort is made to treat the partner.
Barriers to Compliance
Physicians will continue to have a legitimate concern about medico-legal recourse until all states define policy protecting such treatment. Analysis suggests that as of 2013 expedited partner therapy is permitted in 27 states and one city, potentially permitted in 15 states, and prohibited in 8 states. The CDC maintains a web site [12,13] with information about the legal status of expedited partner therapy in all 50 states and other jurisdictions. EPT is prohibited in Arkansas, Florida, Kentucky, Michigan, Ohio, Oklahoma, South Carolina and West Virginia [14,15].
States with providers more receptive to EPT are more likely to pass a law supporting EPT; and, patients in jurisdictions with approved EPT laws receive EPT 10 fold more than patients in regions that do not have laws on EPT [13].
Additionally, many physicians have concerns with PDPT since they are unfamiliar with the medical history of many of the patients they would be treating with PDPT. Adverse reactions and allergies ranging from skin to anaphylactic reactions pose serious concerns that prevent PDPT. Minor side effects such as nausea and vomiting can also affect the success of treatment in up to five percent of patients [16].
The majority of physicians are also cautious in instituting PDPT due to poor follow up in the affected age group. Many physicians who consider utilizing PDPT question whether the partner may be co-infected with multiple STDs in the peri treatment period which is a contraindication to EPT [12,13,16]. Patients that do not follow up cannot be re-cultured or examined which is a potential hazard. However, many studies have proven that the benefits of EPT outweigh the risks including lack of follow up, allergies, and cost. States with EPT laws have laws requiring providers utilizing EPT to: advise index patients to return for medical care three months after treatment for follow-up and re-testing for STDs; counsel the patient to notify sex partner(s) that they may have been exposed to a STD and should seek evaluation and treatment; ensure that patients receive information materials for themselves and their sex partner(s); counsel patient to inform his or her sex partners that it is important to read the partner information prior to the partner or partners taking the medication [16].
Health education materials include specific guidelines to seek care if they are pregnant; develop side effects from treatment; are high risk of comorbid conditions such as HIV or other STDs; encourage partners to seek medical care regardless of whether they used EPT or not; how to prevent future STDs; and to abstain from intercourse for at least seven days in the peri treatment period. Many state laws allowing EPT have regulations protecting heath care providers and pharmacists who dispense EPT and follow the above guidelines to not be subject to liability or be deemed to have engaged in unprofessional conduct. This not only protects providers utilizing EPT but also ensures that patients receive instructions regarding the importance of follow up after treatment.
Limitations
Potential limitations of the study included that there was a disproportionate number of resident physicians who answered the survey as opposed to attending physicians in this study. Nevertheless, given the limited exposure to patient care, and current Medicare laws that govern resident autonomy, residents tend to practice similar to their mentors as evidenced by the consistent responses between resident and attending physicians.
Power analysis was not performed prior to the study. Every attempt was made to recruit as many possible physicians at the particular meetings that questionnaires were distributed. Furthermore, while the doctors surveyed attended the same meeting, they worked at different institutes composed of 20 different hospitals and two academic centers.
Conclusions
As the data show, STD treatment varies greatly amongst physicians. The majority of resident and attending physicians does not institute PDPT and do not follow CDC prescribed guidelines for STD treatment.
Effective clinical management of patients with STDs requires treatment of the patent and the patient’s recent sex partners to prevent re-infection and curtail further transmission. STD treatment is also necessary to prevent its morbid sequela, such as infertility and CPPS that can have psychosocial ramifications [11].
Perhaps in the future, governing health care associations could institute continuing medical education (CME) courses to review the latest STD treatment guidelines. These CME course should be standard across the board for all specialties. This would aid in greater reimbursement to physicians given the quickly evolving health care policies as well as decrease the epidemiology of those diseases that could be contained with EPT.
With more research and the education of health care providers, there will be more continuity among the specialties in the approach and management of STDs.
References
- Berger R, Jay L (2002) Sexually transmitted diseases: The classic diseases, in Walsh P. Philadelphia: Saunders 1: 671-687.
- Weigler A, Perry C, Weigler G (2005) Prevalence of sexually transmitted diseases in women with urinary complaints: a prospective study. Poster presentation at the American College of Osteopathic Emergency Physicians.
- Duffy E, McCollough M (2000) Sexually transmitted diseases in adolescents. The Practical J of Ped Em Med 4: 31-39.
- Centers for Disease Control and Prevention, Workowski KA, Berman SM (2006) Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep 55: 1-94.
- Kissinger P, Brown R, Reed K, Salifou J, Drake A, et al. (1998) Effectiveness of patient delivered partner medication for preventing recurrent Chlamydia trachomatis. Sex Transm Infect 74: 331-333.
- Ramstedt K, Forssman L, Johannisson G (1991) Contact tracing in the control of genital Chlamydia trachomatis infection. Int J STD AIDS 2: 116-118.
- Shillinger J, Kissinger P, Calvet H, Whittington WL, Ransom RL, et al. (2003) Patient-delivered partner treatment with azithromycin to prevent repeated Chlamydia trachomatis infection among women: A randomized, control trial. Sex Transm Dis 30: 49-56.
- Golden M, Whittington W, Handsfield H. Impact of expedited sex partner treatment on recurrent or persistent gonorrhea or chlamydial infection: A randomized, controlled trial. N Eng J Med. In Press.
- Hogben M, McCree DH, Golden MR (2005) Patient-delivered partner therapy for sexually transmitted diseases as practiced by U.S. physicians. Sex Transm Dis 32: 101-105.
- Berger R (2007) Infection and Inflammation of the Geintourinary Tract. The Journal of Urology 178: 1338-1340.
- Taylor MM, Collier MG, Winscott MM, Mickey T, England B (2011) Reticence to prescribe: utilization of expedited partner therapy among obstetrics providers in Arizona. Int J STD AIDS 22: 449-452.
- Sexually Transmitted Diseases (STDs) (2010) Centers for Disease control and prevention 60.
- Legal Status of Expedited Partner Therapy (2012) Centers for Disease control and prevention.
- Cramer R, Leichliter JS, Stenger MR, Loosier PS, Slive L; SSuN Working Group (2013) The legal aspects of expedited partner therapy practice: do state laws and policies really matter? Sex Transm Dis 40: 657-662.
- (2011) Committee opinion no. 506: expedited partner therapy in the management of gonorrhea and chlamydia by obstetrician-gynecologists. Obstet Gynecol 118: 761-766.
- Department of Health (2013) Expedited Partner Therapy Guidelines for Health Care Providers in NYS for Chlamydia trachomatis.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 16870
- [From(publication date):
November-2013 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 12247
- PDF downloads : 4623