Research Article Open Access
Ropivacaine versus Bupivacaine in Postoperative Pain Control
Noha Ahmed Mansour, Fouad A-Mahdy AL-Belasy, Mohamed Abdel-Monem Tawfik and Hamdy A Marzook*Oral Surgery Department, Faculty of Dentistry, Mansoura University, Egypt
- Corresponding Author:
- Hamdy A Marzook
Oral Surgery Department, Faculty of Dentistry
Mansoura University, Egypt
E-mail: marzook_h@hotmail.com
Received date: September 02, 2012; Accepted date: April 25, 2012; Published date: April 27, 2012
Citation: Mansour NA, Al-Mahdy Al-Belasy F, Abdel-Monem MT, Marzook HA (2012) Ropivacaine versus Bupivacaine in Postoperative Pain Control. J Biotechnol Biomater 2:137. doi:10.4172/2155-952X.1000137
Copyright: © 2012 Mansour NA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
Abstract
Objective: The aim of this study was to compare between 2 types of long acting anesthetics: bupivacaine 0.5% and ropivacaine 0.75%, in terms of their duration of anesthesia, duration of analgesia and their effect in controlling postoperative pain after surgical removal of impacted lower third molars. Material and Methods: This study was conducted on fifty subjects referred to the Oral Surgery Department, Faculty of Dentistry, Mansoura University, for surgical removal of impacted lower third molar. Subjects were randomly assigned prior to surgery into 2 nerve block injections; the first group (group A) for an inferior alveolar nerve block (IANB) using bupivacaine and the second group (group B) for an IANB using ropivacaine. In each group, the patient’s age, sex, type of impaction, severity of impaction was recorded. Time from the start of surgery till removal of impacted molar was taken as duration of surgery. Patients were instructed not to take any analgesics until numbness of lip and tongue receded.The time from onset of anaesthesia to when numbness of the lip and tongue receded as assessed by pricking is taken as the duration of anaesthesia. The time from the start of numbness to when the subject first requested a dose of oral analgesic (NSAID) was taken as duration of analgesia. Pain was assessed preoperatively and postoperatively, then patients instructed to record the extent of their pain at 3, 6, 9, and 12 hours on the day of surgery (D1), on the second (D2) and third days (D3) postoperatively. Post-operative analgesic consumption, inability to sleep because of pain, degree of overall satisfaction with the anaesthetic efficacy and postoperative pain management were considered. Results: The median duration of anaesthesia for the 7.5 mg/ml concentration of ropivacaine was approximately 6 hours, and for bupivacaine 5 mg/ml was approximately 7 hours. Bupivacaine can provide analgesia for 10.3 hours while ropivacaine can provide analgesia during the first 9.6 hours which is the period of maximum pain after third molar surgery. Conclusion: As regards a comparison of the study drugs with respect to post-operative pain experience, analgesic need and consumption, bupivacaine and ropivacaine appear to have equivalent efficacy.
Keywords
Bupivacaine; Ropivacaine; Impacted lower third molars; Long acting anesthetics; Postoperative pain
Introduction
For many years, anaesthesiologists and pharmacologists have been searching for an ideal local anaesthetic solution with prolonged action and low toxicity [1]. Experiments with the piperidine ring of cocaine combined with the xylidine component of lidocaine resulted in the pipecoloxylidine family of local anaesthetics which included the long acting local anaesthetics; mepivacaine, bupivacaine and ropivacaine [2]. These drugs possess enhanced lipid solubility characteristics (making them extremely potent) and display an increased affinity for protein binding which dramatically increases the duration of achievable anaesthesia. This biochemical trait makes this group of drugs far more superior than their short acting analogues [3].
Long acting local anaesthetics not only produce localised sensory and motor anaesthesia, but also provide effective postoperative pain relief and analgesia. Therefore, there are 2 primary indications for utilization of long acting local anaesthetics in dentistry: (1) lengthy dental procedures for which pulpal anaesthesia in excess of 90 minutes is necessary and (2) management of postoperative pain [4,5].
For several decades, bupivacaine has been the most widely used long acting local anaesthetic. However, after the report of cases of simultaneous seizure and cardiac arrest, with prolonged resuscitation and a disproportionally high number of deaths following unintended intravascular injection of bupivacaine [6], it became evident that bupivacaine differs from other local anaesthetics in that it has a narrower margin between the dose or plasma concentrations required to produce seizures and those resulting in cardiovascular collapse [7]. For this reason, there has been a search for alternative drugs with a greater margin of safety. As a result ropivacaine was introduced into clinical practice. Since then, it has been the focus of interest because of its increased cardiovascular safety compared with bupivacaine [8]. Ropivacaine, however, has not been widely used in clinical dentistry yet. Therefore, there is a need to establish a well-defined profile for this drug in the management of dental pain.
Aim of the Work
The aim of this study was to compare between two types of long acting local anaesthetics: bupivacaine 0.5% and ropivacaine 0.75%, in terms of their duration of anaesthesia, duration of analgesia and their effect in controlling postoperative pain after surgical removal of impacted lower third molars.
Materials and Methods
Materials
Bupivacaine hydrochloride (Marcaine®) 5 mg/ml (0.5%) and ropivacaine hydrochloride (Naropin®) 7.5 mg/ml (0.75%) anaesthetic solutions were supplied by AstraZeneca in sterile packs. Because these drugs were not available in the single-use dental cartridges, the injection solutions were prepared in the same way used by Kennedy et al. [9]. For ropivacaine, the anesthetic solution was drawn from a 10 mL vial of 0.75% Naropin into the conventional 1.8 mL sterile dental cartridge. For bupivacaine, each 1.8 mL of the anaesthetic solution was drawn from 4 ml vial of 0.5% Marcaine into the conventional sterile dental cartridge.
Patients
Fifty patients referred to the Oral Surgery Department, Faculty of Dentistry, Mansoura University, for surgical removal of impacted lower third molars, were recruited in this study. All subjects included were subjected to a formal case history taking as well as clinical and radiographic examinations.
Patients included were required to have no medical problems. Excluded were those with known hypersensitivity to amide type local anaesthetics, history of substance abuse, and chronic opioid intake as well as pregnant or lactating females [10]. Patients using analgesics were also instructed to stop these medications on the night before surgery [11].
For each patient, age, sex, type and severity of impaction were recorded. Type of impaction was recorded according to winter’s classification as vertical impaction (VR), mesioangular impaction (MA), distoangular impaction (DA), and horizontal impaction (HR). Severity of impaction was rated as partial soft tissue impaction (PSI), complete soft tissue impaction (CSI), partial bony impaction (PBI), and complete bony impaction (CBI) [12].
Preoperative pain was assessed using the Verbal Categorical Scale (VCS) [13]. (0) no pain, (1) mild pain or pain that was recognizable but not discomforting, (2) indicated moderate pain or pain that was discomforting but bearable and (3) indicated severe pain or pain that caused considerable discomfort and was difficult to bear. Patients were also shown how to complete a pain questionnaire to assess postoperative pain using the same VCS [14].
Surgical procedure
Patients were randomly assigned prior to surgery into 2 nerve block injections; the first group (group A) for an inferior alveolar nerve block (IANB) using bupivacaine and the second group (group B) for an IANB using ropivacaine.
Each patient received 2 cartridges of either ropivacaine or bupivacaine with a total dose of 3.6 ml, of which 3 ml was used to block the inferior alveolar and lingual nerves and 0.6 ml for infiltration of long buccal nerve opposite to lower second and third molars. Injections were done using an aspirating syringe where aspiration was made prior to each injection.
After drug administration, anaesthetic effect was subjectively monitored every 20 seconds by asking subjects whether their lip and tongue felt numb. One minute after reporting numbness, anaesthetic effect was objectively assessed by gentle pricking with a sharp dental probe. Probing is continued at one-minute interval until all areas were declared as numb. Once adequate anaesthesia was achieved, surgical removal of the lower wisdom tooth was undertaken [15]. The time from the start of surgery till removal of impacted lower third molar was taken as the duration of surgery [16].
After surgery a treatment regimen was given for each patient including amoxicillin 500 mg/8h and ketoprofen (NSAID) 50 mg/prn. Patients were advised to only take the analgesic if necessary to control pain.
Postoperative assessment
Patients were instructed to palpate the lower lip every 15 minutes to determine at what time numbness of lip completely disappeared and was there a return to normal sensation (absence of pins-and-needles sensations) [9].The time from onset of anesthesia to when numbness of the lip and tongue receded as assessed by pricking was taken as the duration of anesthesia [15].
Patients were instructed not to take any analgesics until numbness of lip and tongue receded. The time from the start of numbness to when the subject first requested a dose of oral analgesic was taken as duration of analgesia [15].
Patients were instructed to rate the extent of their pain at 3, 6, 9, and 12 h on the day of surgery (D1), on the first day after surgery (D2) and second day after surgery (D3) using the same VCS [16].
Post-operative analgesic consumption was based on the number of tablets used on a daily basis; on the day of surgery (D1), first day after surgery (D2) and second day after surgery (D3) [17]. Patients were also asked about inability to sleep because of pain on D1, D2 and D3 [17]. Each patient indicated the degree of overall satisfaction with the anaesthetic efficacy and postoperative pain management on a 4-point scale (1= poor, 2 =satisfactory, 3= good, 4= excellent), and if he/she would have a similar operation using the same type of anesthesia [17,18].
All patients were contacted by telephone the day after surgery and encouraged to complete their questionnaires. All subjects were reviewed for adverse events the next day after surgery and again 7 days after surgery to remove sutures [15].
Statistical analysis
Collected data were statistically analyzed using independent T-test for parametrical parameters and chi-square test for non parametrical parameters with a P value < 0.05 considered as statistically significant.
Results
50 subjects participated in this study; group A included 25 patients (11 females and 14 males) ranging in age from 19 to 27 years with a mean age of 23.04 years. Group B included 25 patients (13 females and 12 males) ranging in age from 19 to 29 years with a mean age of 23.4 years.
Mean duration of surgery for removal of the impacted lower wisdom was 43.40 minutes in group A and 41 minutes in group B. There was no significant difference between the 2 groups in relation to age, sex and duration of surgery (P > 0.05). In regard to type of impaction, the bupivacaine group had 6 vertical impactions, 7 mesioangular, 5 distoangular, and 7 horizontal impactions. The ropivacaine group had 7 vertical impaction, 6 mesioangular impaction, 5 distoangular impaction, and 7 horizontal impactions. Concerning the severity of impaction, there were 5 soft tissue impactions and 20 bony impactions in each group. In the bupivacaine group 3 impactions were partial soft tissue and 2 were complete soft tissue and bony impactions were 14 partial bony and 6 complete bony. In the ropivacaine group 4 impactions were partial soft tissue and 1 was complete soft tissue and bony impactions were 15 partial bony and 5 complete bony. No significant difference was noted between the 2 groups concerning the severity of impaction (P > 0.05).
Thirteen patients in bupivacaine group and 11 patients in ropivacaine group presented with no pain. Mild pain was reported by 7 patients in bupivacaine group and 10 patients in ropivacaine group. Moderate pain was reported by 4 patients in bupivacaine group and 3 patients in ropivacaine group. Only 1 patient in each group presented with severe pain. In relation to preoperative pain, there was no significant difference between the 2 patient groups (P > 0.05).
On the day of surgery (D1), assessments of postoperative pain in the 2 patient groups were comparable with no significant differences (P > 0.05). For immediate postoperative pain, 21 patients in bupivacaine group and 20 patients in ropivacaine group had no pain. 4 patients in bupivacaine group and 5 patients in ropivacaine group had mild pain. No patient in both groups had moderate or severe pain.
Three hours postoperatively, 22 patients in bupivacaine group and 20 patients in ropivacaine group had no pain. 3 patients in bupivacaine group and 5 patients in ropivacaine group had mild pain.
Six hours postoperatively, patients in ropivacaine group had higher pain ratings than patients in bupivacaine group. 19 patients in bupivacaine group and 11 patients in ropivacaine group had no pain. 4 patients in bupivacaine group and 11 patients in ropivacaine group had mild pain. 2 patients in bupivacaine group and 3 patients in ropivacaine group had moderate pain.
After 9 hours, 8 patients in bupivacaine group and 9 patients in ropivacaine group had no pain. 15 patients in bupivacaine group and 9 patients in ropivacaine group had mild pain. 2 patients in bupivacaine group and 6 patients in ropivacaine group had moderate pain. Only 1patient in ropivacaine group had severe pain.
After 12 hours, 6 patients in each group had no pain. 15 patients in bupivacaine group and 14 in ropivacaine group had mild pain. 4 patients in bupivacaine group and 5 in ropivacaine group had moderate pain. On the first day after surgery (D2), no patient had severe pain. 7 patients in bupivacaine group and 8 in ropivacaine group had no pain. 16 patients in bupivacaine group and 11 in ropivacaine group had mild pain. 2 patients in bupivacaine group and 6 patients in ropivacaine group had moderate pain.
On the second day after surgery (D3), 32 subjects had no pain, 6 patients in bupivacaine group and 8 in ropivacaine group had mild pain. 2 patients in each group had moderate pain and no one had severe pain. There was no significant difference between patients in two groups.
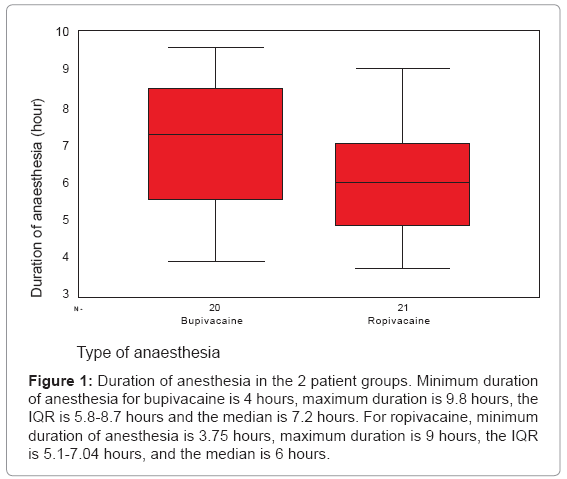
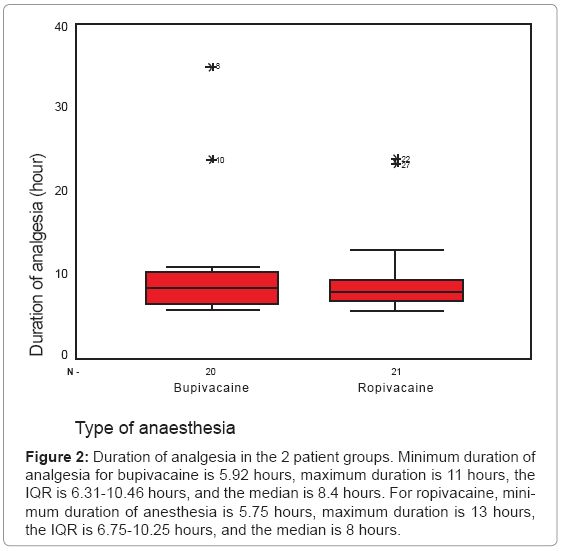
In respect to pain evaluation there was no significant difference between the 2 patient groups on D1, D2 or D3 (P > 0.05). Means of pain scores according to VCS immediately postoperatively, after 3, 6, 9, and 12 hours were (0.16, o.12, 0.32, 0.76 and 0.92) for bupivacaine and (0.20, 0.20, 0.68, 0.96, and 0.96) for ropivacaine. At D2 and D3, means of pain scores were (0.80, 0.40) for bupivacaine and (0.92, 0.48) for ropivacaine. Duration of anesthesia and analgesia were comparable for the 2 groups with no significant difference. Mean duration of anesthesia was 7.01 for bupivacaine and 6.18 for ropivacaine. Mean duration of analgesia was 10.35 for bupivacaine and 9.58 for ropivacaine (Figure 1 and 2).
Figure 1: Duration of anesthesia in the 2 patient groups. Minimum duration of anesthesia for bupivacaine is 4 hours, maximum duration is 9.8 hours, the IQR is 5.8-8.7 hours and the median is 7.2 hours. For ropivacaine, minimum duration of anesthesia is 3.75 hours, maximum duration is 9 hours, the IQR is 5.1-7.04 hours, and the median is 6 hours.
Figure 2: Duration of analgesia in the 2 patient groups. Minimum duration of analgesia for bupivacaine is 5.92 hours, maximum duration is 11 hours, the IQR is 6.31-10.46 hours, and the median is 8.4 hours. For ropivacaine, minimum duration of anesthesia is 5.75 hours, maximum duration is 13 hours, the IQR is 6.75-10.25 hours, and the median is 8 hours.
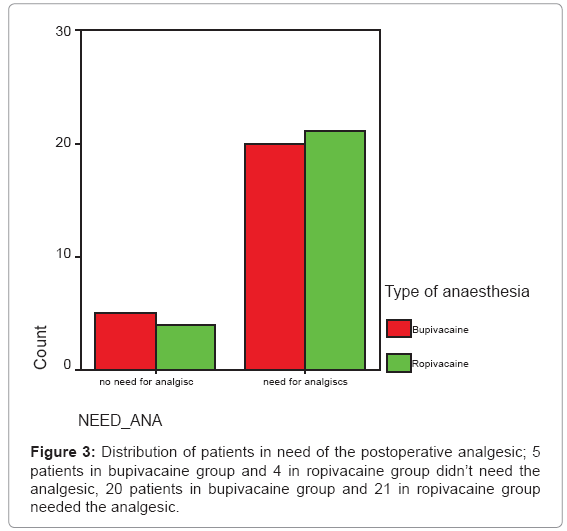
In respect to analgesic consumption, 9 patients didn’t need the analgesic drug for the whole days of assessment (5 in bupivacaine group and 4 in ropivacaine group) while 41 patients needed the analgesic (20 patients in bupivacaine group and 21 in ropivacaine group) (Figure 3).
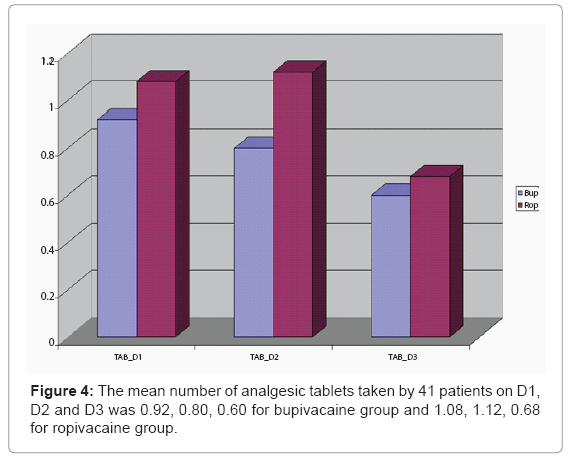
The mean number of analgesic tablets taken by the 41 patients on D1, D2 and D3 was 0.92, 0.80, 0.60 for bupivacaine group and 1.08, 1.12, 0.68 for ropivacaine group with no difference between the 2 patient groups (P > 0.05) (Figure 4).
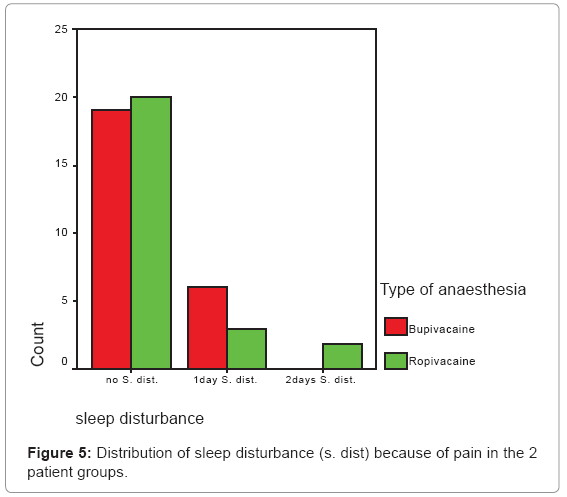
In assessment of patients’ sleep disturbance because of pain, 20 patients in ropivacaine group and19 in bupivacaine group didn’t suffer sleep disturbance. 3 patients in ropivacaine group and 6 in bupivacaine group suffered one day of sleep disturbance. Only 2 patients in ropivacaine group had 2 days of sleep disturbance with no significant difference between the 2 patient groups (P > 0.05) (Figure 5).
Concerning patient satisfaction with the type of anesthesia, the 2 patient groups showed no statistically significant difference on D1, D2, and D3 (P > 0.05). On the day of surgery (D1), patient satisfaction with ropivacaine was rated as poor in 1 patient, satisfied in 7 patients, good in 13 patients and excellent in 4 patients. With bupivacaine, patient satisfaction was rated as satisfied in 6 patients, good in 14 patients, and excellent in 5 patients.
On the first day after surgery (D2), patient satisfaction with ropivacaine was rated as poor in 3 patients, satisfied in 5 patients, good in 8 patients and excellent in 9 patients. With bupivacaine, patient satisfaction was rated as poor in 1 patient, satisfied in 6 patients, good in 9 patients and excellent in 9 patients.
On the second day after surgery (D3), patient satisfaction with ropivacaine was rated as poor in 2 patients, satisfied in 2 patients, good in 8 patients and excellent in 13 patients. With bupivacaine, patient satisfaction was rated as poor in 1 patient, satisfied in 3 patients, good in 8 patients and excellent in 13 patients.
Discussion
In dental surgical procedures, a long duration of local anaesthesia is favourable because it may reduce postoperative pain and, hence, the need of analgesic drugs [19]. Bupivacaine is widely used clinically as a potent, long-acting local anaesthetic. Its known potential for central nervous system, and especially cardiovascular system toxicity stimulated a search for new and safer agents, resulting in the introduction of ropivacaine [20]. The lesser toxicity of ropivacaine compared with bupivacaine on the central nervous system (CNS) and cardiovascular system has been confirmed in numerous animal experiments [21-23] as well as human studies [24-26]. This study was designed to compare between the two types of long acting local anaesthetics: bupivacaine 0.5% and ropivacaine 0.75%, in terms of their duration of anaesthesia, duration of analgesia and their effect in controlling postoperative pain after surgical removal of impacted lower third molars. Local signs of inflammation, including pain, usually follow the removal of impacted lower third molars. This procedure has been widely used as a model for evaluation of analgesic efficacy of various drugs. That is why the postoperative analgesic efficacy of ropivacaine and bupivacaine was evaluated after this particular kind of surgical extraction in this study.
The design of the present study comprised 50 patients referred to the Oral Surgery Department, Faculty of Dentistry, Mansoura University, for surgical removal of impacted lower third molars. They were treated without any premedication of sedatives or analgesics. Patients were randomly divided into 2 groups; the first group (group A) included 25 patients for an inferior alveolar nerve block (IANB) using bupivacaine while the second group (group B) included the other 25 patients for an IANB using ropivacaine. The duration of surgery, type and severity of impactions were similar in both groups, indicating that the surgical trauma was comparable for all the patients.
In the first group of patients, two consecutive infiltrations of 1.8 ml of 0.75% ropivacaine were performed in the pterygomandibular region. This was based on the study of Ernberg and Kopp [27] showing that lower doses did not yield an effective anesthetic effect and the success rate for lower concentrations (2.0, 5.0 mg/ml) was unsatisfactory. Ropivacaine in this study was injected alone without the addition of vasoconstrictor. This was based on the study of Lee et al. [28] showing that ropivacaine has intrinsic vasoconstrictor properties. In this regard, Oliveria et al. [29], demonstrated that 0.75% ropivacaine, with and without epinephrine, produced equally effective and well-tolerated regional anaesthesia in treated patients. In the other group of patients, 0.5% bupivacaine was used according to Markovic and Todorovic [30] who demonstrated that 0.5% bupivacaine plain has a potent postoperative analgesic effect after surgical extraction of impacted lower third molars.
Pain is subjective and experienced differently by each individual and the patient’s self report is the most reliable indicator of pain. Therefore, specific tools were developed to assess pain. In this study the parameters used to assess pain intensity were the verbal categorical scale (VCS), duration of analgesia (recorded as time to first requested dose of oral analgesic), the number of analgesic tablets taken after the surgery, sleep disturbance because of pain and patient satisfaction. Self assessment was recorded during the first 3 postoperative days, which is the period of most severe pain following surgical extraction of lower third molar as reported by Oikarinen [31].
The mean duration of anaesthesia (recorded as subjective sensation of lip paresthesia) for the 0.75% concentration of ropivacaine was 6.18 ± 1.25 hours, this was in agreement with the finding of other studies [27-29] using ropivacaine for IANB with the same dose and concentration. The duration of anaesthesia after infiltration of 0.75% ropivacaine ranged from 6 to 8 hours in these 2 studies [27-29]. This duration is several hours longer compared with Lidocaine (3.6 hours) [32], articaine (4.6 hours) and mepivacaine (3.7 hours) [33] when used for surgical removal of lower third molar. However, Axelsson and Isacsson [34] reported longer lip numbness duration (7.5-8.4 hours). They used 2 ml of 0.75 ropivacaine for IANB, assessing its anaesthetic efficacy by lower lip numbness with no surgery done for the study subjects.
The mean duration of anaesthesia for 0.5% bupivacaine was 7.01 ± 2.08 hours. This was also in agreement with other studies [35,36] using 0.5% bupivacaine in third molar surgery and reporting a mean anaesthetic duration of 7-8 hours. In contrast to this study findings, a shorter duration (4.6 ± 2.65 hours) was reported by Branco et al. [37]. However, those authors used 0.5% bupivacaine in half the dose used in this study and tested the second molar with a pulp tester to verify the anaesthesia induced by the IANB whereas this study considered the loss of sensibility of the inferior lip. Concerning the duration of anaesthesia, this study found no significant difference between the two study drugs. This was further in conformity with the study of Fawcett et al. [35].
With respect to post-operative pain experience, both drugs appeared to have equivalent efficacy as reported by Patients in both groups demonstrated a prolonged pain free interval postoperatively. The peak intensity of postoperative pain for the ropivacaine group was reported 9 hours postoperatively (mean pain scores = 0.96), but the highest postoperative pain scores were measured 9-12 hours postoperatively for bupivacaine group (mean pain scores = 0.76-0.92). At 6 hours postoperatively, the mean pain score of ropivacaine was slightly higher than that of bupivacaine (0.68 and 0.32 respectively) but no significant difference was found statistically.
The time for first analgesic request was slightly delayed in bupivacaine group than ropivacaine group. Bupivacaine can provide analgesia for 10.3 hours while ropivacaine can provide analgesia during the first 9.6 hours which is the period of maximum pain after third molar surgery. This is in concordance with evaluation of pain in this study; as the analgesic effect of study drugs decreased just at the time when the postoperative pain began to peak. Hence, additional rescue analgesics were required for good postoperative pain management.
The duration of analgesia of bupivacaine recorded in this study was in agreement with that recorded by Nayyar and Yates [10] who used 0.5% bupivacaine for IANB before third molar surgery and reported duration of analgesia of 8-12 hours. However, a study comparing the efficacy of racemic bupivacaine and S-bupivacaine in third molar surgery [35] reported short duration of analgesia (2-3 hous). The duration of analgesia of ropivacaine recorded in this study was in agreement with that of Casati et al. [38] who recorded duration of analgesia (9.8 hours) with 0.75% ropivacaine when used for axillary brachial plexus block and this duration is several hours longer than that of mepivacaine (6 hours). The present study showed that ropivacaine did not differ from bupivacaine with respect to duration of analgesia. This was in agreement with previous studies comparing the postoperative analgesic efficacy of ropivacaine and bupivacaine in different types of nerve block for knee and hand surgery [39-41].
Due to long period of pain free interval postoperatively, patients’ dependency on pain relieving medications was reduced. Nine patients didn’t need any analgesic tablets postoperatively and for three days after operation (5 subjects in bupivacaine group and 4 subjects in ropivacaine group); mean number of analgesic tablets consumed over 3 days was nearly equal for two groups. This study showed that ropivacaine did not differ from bupivacaine with respect to postoperative rescue analgesic requirement as reported by other authors [35,42-45] who found that the increased duration of analgesia with long acting anaesthetics reduces the analgesic consumption after third molar surgery. Interestingly, a study of patients undergoing lower limb surgery who received ropivacaine hydrochloride for operative anaesthesia reported no use of supplemental analgesia in the first 24 hours after surgery by 37% of the patients. This number dropped to 10% when mepivacaine was used [46].
It was stated that the pre-emptive nerve block with long acting local anaesthetic results in reduction of postoperative pain and can prevent the central hypersensitivity that occurs as a result of surgical trauma [47]. Perhaps because neural blockade prevents nociceptive impulses from entering the central nervous system during and immediately after surgery and thus suppresses formation of the sustained hyperexcitable state in the central nervous system that is responsible for the maintenance of postoperative pain [48]. In the present study, the long duration of anaesthesia and analgesia of ropivacaine was adequate to cover the pain during surgery and also the pain during postoperative period. Therefore, ropivacaine proved ideal to act in a pre-emptive manner.
As regard patient satisfaction with the efficacy of analgesia, the mean was approximately equal for the two drugs for 3 days postoperatively. Most patients recorded good satisfaction on first day and excellent satisfaction on second and third days postoperatively. It is likely that good pain relief resulted in greater patient satisfaction. Rawal and co-workers [41] reported equal patients’ satisfaction for ropivacaine and bupivacaine after hand surgery. Bertini and colleagues [49] demonstrated better patient satisfaction scores with 0.75% ropivacaine than 0.5% bupivacaine following hip replacement.
Finally, all patients were discharged within 15 minutes postoperatively, and none suffered from any significant complications. At the 24-hour telephone follow up call, patients reported no major side effects, and no evidence of toxicity was recorded in any patient.
Conclusion
Based on the results of this study it can be concluded that:
1. Both ropivacaine and bupivacaine have an identical duration of anaesthesia.
2. The efficacy of ropivacaine in controlling postoperative pain after surgery of lower third molars is not different from that of bupivacaine.
3. Both ropivacaine and bupivacaine have an identical duration of analgesia plus an equal effect in decreasing postoperative analgesic requirement after third molar surgery.
Recommendations
1. This study recommends ropivacaine 7.5 mg/ml as an alternative to bupivacaine as a long acting local anaesthetic. Not only is it possible to get sufficient anaesthesia for several hours, but also postoperative pain and analgesic consumption are reduced for a considerable time.
2. The long duration of both anaesthesia and analgesia of ropivacaine 7.5 mg/ ml after mandibular nerve block and its lower CNS and cardiovascular toxicity prompt encouragement of the pharmaceutical industry to make this drug commercially available in single-use dental cartridges.
References
- Graf BM (2001) The cardiotoxicity of local anesthetics: the place of ropivacaine. Curr Top Med Chem 1: 207-214.
- Mepivacaine (2000) In: Tetzlaff JE. Clinical pharmacology of local anesthetics. Boston (MA): Butterworth Heinemann 2: 97-102.
- Bowles P (2006) Is Ropivacaine Hydrochloride more effective than Bupivacaine hydrochloride at reducing post-operative pain levels following foot surgery?
- Doris RW, Dangler LA, Greengrass RA (2001) Update on ropivacaine. Expert Opinion on Pharmacother 2: 2051-2063.
- Malamed SF (2004) Handbook of local anesthesia. (5thedn), St. Louis, Mosby.
- Albright GA (1979) Cardiac arrest following regional anesthesia with etidocaine or bupivacaine. Anesthesiology 51: 285-287.
- Bruelle P, LeFrant JY, de La Coussaye JE, Peray PA, Desch G, et al. (1996) Comparative electrophysiologic and hemodynamic effects of several amide local anesthetic drugs in anesthetized dogs. Anesth Analg 82: 648-656.
- Hansen TG (2004) Ropivacaine: a pharmacological review. Expert Rev Neurother 4: 781-791.
- Kennedy M, Reader A, Beck M, Weaver J (2001) Anesthetic efficacy of ropivacaine in maxillary anterior infiltration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91: 406-412.
- Nayyar MS, Yates C (2006) Bupivacaine as pre-emptive analgesia in third molar surgery: Randomised controlled trial. Br J Oral and Maxillofac Surg 44: 501-503.
- Mcnamee DA, Convery PN, Milligan KR (2001) Total knee replacement: a comparison of ropivacaine and bupivacaine in combined femoral and sciatic block. Acta Anaesthesiol Scand 45: 477–481.
- Ziccardi VB, Desjardins PJ, Daly-DeJoy E, Seng GF (2000) Single-Dose Vicoprofen Compared with Acetaminophen With Codeine and Placebo in Patients with Acute Postoperative Pain After Third Molar Extractions. J Oral Moxillo fac Surg 58: 622-628.
- Chapman CR, Syrjala KL (2000) Bonica’s management of pain, (2ndedn) Philadelphia, Lippincott.
- Campbell WI, Kendrick RW (1997) Pre-emptive analgesia using local anaesthesia: a study in bilaterally symmetrical surgery. Br J Anaesth 79: 657-659.
- Fawcett JP, Kennedy JM, Kumar A, Ledger R, Kumara GM, et al. (2002) Comparative efficacy and pharmacokinetics of racemic bupivacaine and s-bupivacaine in third molar surgery. J Pharm Pharmaceut Sci 5: 199-204.
- Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Creminelli L, et al. (2007) Assessing Postoperative Discomfort After Third Molar Surgery: A Prospective Study. J Oral Maxillofac Surg 65: 901-917.
- Ng HP, Nordström U, Axelsson K, Perniola AD, Gustav E, et al. (2006) Efficacy of intra-articular bupivacaine, ropivacaine, or a combination of ropivacaine, morphine, and ketorolac on postoperative pain relief after ambulatory arthroscopic knee surgery: a randomized double-blind study. Reg Anesth Pain Med 31: 26-33.
- Tuncer B, Babacan A, Arslan M (2007) Preemptive intraarticular tramadol for pain control after arthroscopic knee surgery. Agri 19: 42-49.
- Johansson B, Glise H, Hallerbäck B, Dalman P, Kristoffersson A (1994) Preoperative local infiltration with ropivacaine for postoperative pain relief after cholecystectomy. Anesth Analg 78: 210-214.
- Nau C, Strichartz GR (2002) Drug chirality in anesthesia. Anesthesiology 97: 497–502.
- Zink W, Bohl JR, Hacke N, Sinner B, Martin E, et al. (2005) The long term myotoxic effects of bupivacaine and ropivacaine after continuous peripheral nerve blocks. Anesth Analg 101: 548-554.
- Zhang S, Yao S, Li Q (2003) Effects of ropivacaine and bupivacaine on rabbit myocardial energetic metabolism and mitochondria oxidation. J Huazhong Univ Sci Technolog Med Sci 23: 178-179.
- Danielsson BR, Danielson MK, Böö EL, Arvidsson T, Halldin MM (1997) Toxicity of bupivacaine and ropivacaine in relation to free plasma concentrations in pregnant rats: A comparative study. Pharmacol Toxicol 81: 90-96.
- Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N (1997) Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth 78: 507–514.
- Mather LE, Chang DH (2001) Cardiotoxicity with modern local anaesthetics: Is there a safer choice? Drugs 61: 333–342.
- Ryu HY, Kim JY, Lim HK, Yoon J, Yoo BS, et al. (2007) Bupivacaine Induced Cardiac Toxicity Mimicking an Acute Non-ST Segment Elevation Myocardial Infarction. Yonsei Med J 30: 331-316.
- Ernberg M, Kopp S (2002) Ropivacaine for dental anesthesia: a dose finding study. J Oral Maxillofac Surg 60: 1004-1010.
- Lee BB, Ngan Kee WD, Plummer JL, Karmakar MK, Wong AS (2002) The effect of the addition of epinephrine on early systemic absorption of epidural ropivacaine in humans. Anesth Analg 95: 1402-1407.
- Oliveira NE, Lima Filho NS, Lima EG, Vasquez EC (2006) Effects of regional anesthesia with ropivacaine on arterial pressure and heart rate in healthy subjects. Eur J Oral Sci 114: 27-32.
- Markovic AB, Todorovic L (2006) Postoperative analgesia after lower third molar surgery: contribution of the use of long-acting local anesthetics, low-power laser, and diclofenac. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102: e4-e8.
- Oikarinen K (1991) Postoperative pain after mandibular third-molar surgery. Acta Odontol Scand 49:7-13.
- Porto GG, Vasconcelos BC, Gomes AC, Albert D (2007) Evaluation of lidocaine and mepivacaine for inferior third molar surgery. Med Oral Patol Oral Cir Bucal 12: E60-64.
- Colombini BL, Modena KC, Calvo AM, Sakai VT, Giglio FP, et al. (2006) Articaine and mepivacaine efficacy in postoperative analgesia for lower third molar removal: a double-blind, randomized, crossover study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102: 169-174.
- Axelsson S, Isacsson G (2004) The efficacy of ropivacaine as a dental local anaesthetic. Swed Dent J 28: 85-91.
- Fawcett JP, Kennedy JM, Kumar A, et al. (2002) Comparative efficacy and pharmacokinetics of racemic bupivacaine and S-bupivacaine in third molar surgery. J Pharm Pharm Sci 5: 199-204.
- Danielsson K, Evers H, Holmlund A, Kjellman O, Nordenram A, et al. (1986) long acting local anaesthetics in oral surgery. Int J Oral Maxillofac Surg 15: 119-126
- Branco FP, Ranali J, Ambrosano GM, Volpato MC (2006) A double-blind comparison of 0.5% bupivacaine with 1:200,000 epinephrine and 0.5% levobupivacaine with 1:200,000 epinephrine for the inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101: 442-447.
- Casati A, Leoni A, Aldegheri G (1998) A double-blind study of ropivacaine for sciatic nerve block. Eur J Anaesthesiol 15: 549-452.
- Marret E, Gentili M, Bonnet MP, Bonnet F (2005) Intra-articular ropivacaine 0.75% and bupivacaine 0.50% for analgesia after arthroscopic knee surgery: a randomized prospective study. Arthroscopy 21: 313-316.
- Fanelli G, Casati A, Beccaria P, Aldegheri G, Berti M, et al. (1998) A double-blind comparison of ropivacaine, bupivacaine, and mepivacaine during sciatic and femoral nerve blockade. Anesth Analg 87: 597-600.
- Rawal N, Allvin R, Axelsson K, Hallén J, Ekbäck G, et al. (2002) Patient-controlled regional analgesia (PCRA) at home: controlled comparison between bupivacaine and ropivacaine brachial plexus analgesia. Anesthesiology 96: 1290-1296.
- Bouloux GF, and Punnia-Moorthy A (1999) Bupivacaine versus Lidocaine for Third Molar Surgery: A Double-Blind, Randomized, Crossover Study. J Oral Maxillofac Surg 57: 510-514.
- Chapman PJ, Macleod AW (1985) A clinical study of bupivacaine for mandibular anesthesia in oral surgery. Anesth Prog 32:69-72.
- Ozen M, Inan N, Tümer F, Uyar A, Baltaci B (2006) The effect of 3-in-1 femoral nerve block with ropivacaine 0.375% on postoperative morphine consumption in elderly patients after total knee replacement surgery. Agri 18: 44-50.
- Samoladas EP, Chalidis B, Fotiadis H, Terzidis I, Ntobas T, et al. (2006) The intra-articular use of ropivacaine for the control of post knee arthroscopy pain. J Orthop Surg Res 1: 17.
- Cappellino A, Jokl P, Ruwe PA (1999) Regional anesthesia in knee arthroscopy: a new technique involving femoral and sciatic nerve blocks in knee arthroscopy. Arthroscopy 12: 120-123.
- Gordon SM, Dionne RA, Brahim J, Jabir F, Dubner R (1997) Blockade of peripheral neuronal barrage reduces postoperative pain. Pain 70: 209-215.
- Tverskoy M, Cozacov C, Ayache M, Bradley EL Jr, Kissin I (1990) Postoperative pain after inguinal herniorrhaphy with different types of anesthesia. Anesth Analg 70: 29-35.
- Bertini L, Mancini S, Di Benedetto P, Ciaschi A, Martini O, et al. (2001) Postoperative analgesia by combined continuous infusion and patient-controlled epidural analgesia (PCEA) following hip replacement: ropivacaine versus bupivacaine. Acta Anaesthesiol Scand 45: 782-785.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 26043
- [From(publication date):
July-2012 - Nov 22, 2025] - Breakdown by view type
- HTML page views : 20711
- PDF downloads : 5332