Research Article Open Access
Role of Laparoscopy in Changing the Management of Hepatocellular Carcinoma
Mohamed Ismail Seleem*, Mohamed Hassany, Hossam E El Shafey and Mohamed S AbdelwahedDepartment of Hepato-biliary Surgery and Tropical Medicine, National Hepatology and Tropical Medicine Research Institute, Cairo, Egypt
- *Corresponding Author:
- Dr. Mohamed Ismail Seleem
Department of Hepatobiliary Surgery and Tropical Medicine
National Hepatology and Tropical Medicine Research Institute
Nasr City, Cairo, Egypt
Tel: +201113447442
E-mail: saleem_1961@hotmail.com
Received date: September 11, 2013; Accepted date: October 15, 2013; Published date: October 20, 2013
Citation: Seleem MI, Hassany M, Shafey HEE, Abdelwahed MS (2013) Role of Laparoscopy in Changing the Management of Hepatocellular Carcinoma. J Gastroint Dig Syst 3:147. doi: 10.4172/2161-069X.1000147
Copyright: © 2013 Seleem MI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Laparoscopic approach offers the advantages of intra-operative laparoscopic ultrasonography (IOLUS), which provides better resolution of the number and location of liver tumors, and liver condition. In recent years the progress of laparoscopic procedures and the development of new and dedicated technologies have made laparoscopic hepatic surgery feasible and safe. The aim of this study is to present the results of our experience in laparoscopic management of Hepatocellular carcinoma (HCC) in cirrhotic patients.
Patients and methods: Between September 2010 and January 2013, Four hundred patients with HCC in liver cirrhosis were referred from HCC clinic at National Hepatology and Tropical Medicine Research Institute (NHTMRI). 65 patients were submitted to diagnostic laparoscopy. 33 patients had Laparoscopic Radiofrequency Ablation with IOLUS guidance and 14 patients had laparoscopic non-anatomical resection while 18 patients had been converted to open laparotomy. Operation time, hospital stay, post-procedure complications were recorded. Spiral CT scan one month postoperative was mandatory during follow up.
Results: Laparoscopic management was completed in 47 patients. The IOLUS examination identified new HCC in three patients. A total of 50 lesions were treated laparoscopically. The mean operative time was 120 ± 50 minutes; eight procedures were associated in six patients: cholecystectomy (6) and adhesiolysis (2). A complete tumor ablation was observed in treated patients by LRFA which were documented via spiral computed tomography (CT scan) one month after treatment. In resection group, histopathology was confirmed that, all tumor resection were with safety margin.
Conclusion: Laparoscopic procedure proved to have a role in changing the management of HCC either by resection or by LRFA. Laparoscopy proved to be a safe and effective technique.
Keywords
Laparoscopy; HCC; Liver resection; RFA; IOUS; Liver cirrhosis
Introduction
Th e introduction of minimally invasive surgical techniques presents the potential to avoid unnecessary laparotomies in many patients with hepatic malignant neoplasms by improving the accuracy of staging with laparoscopic inspection in addition of laparoscopic ultrasound. Laparoscopic inspection alone has proved to be a useful adjunct to pre-operative imaging studies in evaluation of hepatic malignant neoplasms for potential resection and identification of extrahepatic nodal or peritoneal involvement [1]. Hepatocellular carcinoma (HCC), the most common primary liver cancer, occurs in 90% of the cases in patients with chronic liver disease (CLD) [2]. In recent years, its incidence has increased as consequence of chronic hepatitis C virus infections [3]. The optimal treatment for hepatocellular carcinoma is surgical resection. However, only a small percentage of patients are operative candidates. Therapeutic options with curative intent for small HCC in patients with CLD include hepatic resection, local ablation (ethanol injection, microwave, radiofrequency) and liver transplantation. Laparoscopic radiofrequency ablation (LRFA) appears to be safe procedures with low rates of morbidity and mortality when indicated [4]. Laparoscopic liver resection is technically challenging, however laparoscopic liver resection has increased over the past decade, with several thousand cases now reported [5]. Liver transplantation is best theoretical treatment of those patients by removing both the tumor and underlying CLD, however it cannot be applied on large scale because of the high prevalence of HCC and donor shortage. The decision making for treatment of HCC in patient with CLD is depend on general condition of the patient, liver condition (laboratory, radiology and laparoscopic inspection) and tumor situation (size and site). Here, we present small series of patients with HCC, their management was depend on laparoscopic inspection finding.
Patient and Method
This study was conducted at the National Hepatology and Tropical Medicine Research Institute, Cairo, Egypt. It was carried out from September 2010 to January 2013 with the approval of our Institutional Research Ethics Board, 400 patients with HCC in liver cirrhosis were referred from HCC clinic. Sixty five patients with HCC who fulfilled the criteria (Table 1) were submitted to diagnostic laparoscopy and the rest of patients were not eligible for surgery. There were 48 male and 17 female. The mean age was 57.4 ± 6.4 years. Patients were classified according Child-Pugh score. Preoperative triphasic (arterial, portal and venous) spiral CT examinations through seven-millimeter slices were obtained throughout the liver in each patient represented in this group. The maximum diameter of each visible lesion was measured and the precise location of the lesion was determined with the segmental anatomic mapping system proposed by the Brisbane World Congress of IHPBA (International Hepato-Pancreato-Biliary Association), defined by the distribution of the hepatic and portal venous systems [6]. Laparoscopic exploration and Liver ultrasound was performed with a flexible linear 7.5 mHz LIOUS transducer (Courtesy of BK Medical, Copenhagen, Denmark). All ultrasound examinations were carried out and interpreted by a single surgeon and single radiologist. 33 patients had laparoscopic radiofrequency ablation with IOLUS guidance for lesions in segments VII and VIII which was difficult to resection, 14 patients had laparoscopic resection for exophytic lesions or lesions in segment V and VI or Peripheral area of segment II and III. The rest of the patients were converted to open surgery because the lesion situation was difficult to deal laparoscopically. Spiral CT scan one month postoperative was mandatory during follow up as well as level of alpha feto-protein.
| (1) HCC near to vital organs such as diaphragm or gut. |
| (2) Exophytic or subcapsular HCC. |
| (3) Patients with Child-Pugh (A and early B). |
| (4) Patients who has an additional surgical indication such as, cholelithiasis, umbilical hernia. |
| (5) Patients with hepatocellular carcinoma 5 cm or less in diameter. |
| (6) Patients with American Society of Anesthesiologists (ASA) I, II, and III patients. |
Table 1: Inclusion criteria.
Laparoscopic procedure
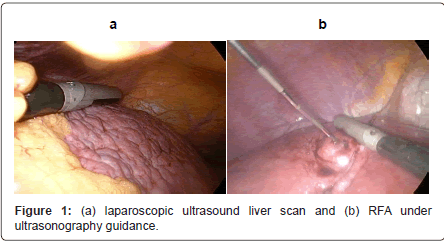
The procedure was performed with the patient under endotracheal general anaesthesia and placed in a supine position on operating table. The surgeon stood on the left side of the patient and the first assistant on the opposite side. The monitors were placed at the head of the table. Through a supra-umbilical incision, carbon dioxide pneumoperitoneum was carried out using Veress needle. Laparoscopic exploration was performed with a zero degree laparoscope. Liver condition was inspected and evaluated. Another 10 mm port was placed left to the begging of faliciform ligament for easy screening the whole liver by laparoscopic ultrasound probe. Additional insertion of 5 mm port according to the location of the HCC. Laparoscopic ultrasound carried out for whole liver followed by localization of HCC (Figure 1a).
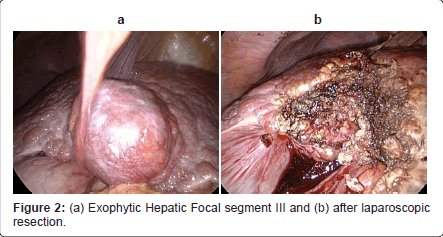
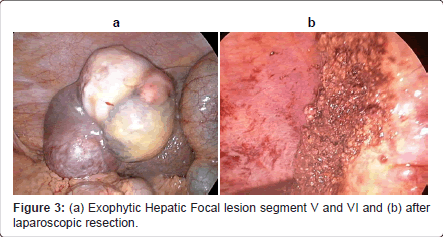
In case of exophytic, subcapsular, left segment II-III (Figure 2a) and right segment IVb-V-VI (Figure 3a) hepatocellular carcinoma associated with fair liver tissue condition. Surgical resection was recommended and proceeds using laparoscopic Habib™ 4X rediofrequency needle (Figures 2b and 3b).
In case of laparoscopic radiofrequency ablation decided to be done, the vital organs near HCC such as stomach, colon or diaphragm were protected by abdominal gauze soaked in saline solution, introduced through the 10 mm port. LRFA was performed under ultrasonography guidance, (Figure 1b) utilizing a generator providing 460 kHz alternating current and a semi-flax retractable multi-pronged curved electrode-needle (RITA medical system, Mountain View, California). The average target temperature was set at 100°C to 110°C, and ablation was continued for 25-45 minutes depending on the desired ablation size (3-5 cm in diameter). The process was monitored by real-time ultrasound to ensure 1 cm margins. The drain was left behind. Drains were removed within 24-48 hours.
Triphasic CT scan was obtained one month post-operatively and abdominal ultrasound and alpha feto-protein (AFP) were obtained every three months during follow up period. Whenever AFP reelevated, further imaging studies such as Triphasic CT scan was performed. Local recurrence was defined as tumor recurred at the treated site. Whereas new tumor which appeared in different hepatic parenchyma was defined as new HCC. For these recurrences or new HCC was treated as indicated.
Results
Sixty-five patients were included in our study. Fifty seven patients were Child-Pugh class-A and eight patients were early class-B. Laparoscopic management was completed in 47 patients. The IOLUS examination identified new HFL in three patients. A total of 50 lesions were laparoscopically treated. Eight procedures were associated in six patients: 6 cholecystectomy and 2 adhesiolysis. The mean diameter of the tumors, measured by preoperative ultrasound, was 32 ± 15 mm. Iaparoscopic ultrasound examination was attempted in all patients. In two patients (3%) the presence of adhesions prevented intraoperative scanning of the liver and adhesiolysis had been done and scanning was completed. In 47 patients (72.3%) therapeutic laparoscopic measures (laparoscopic radiofrequency in 33 patients, laparoscopic liver resection in 12 patients and combined laparoscopic radiofrequency and laparoscopic liver resection had been done for two patients) while 18 patients (27.6%) were converted to open surgery (7 patients had open RFA, 2 patients had open microwave ablation because lesion was near to major vessel, 8 patients had open resection, and one patient had combined open resection and RFA ablation). Mean operative time was 120 ± 50 minutes. Laparoscopic inspection with use of Laparoscopic ultrasound had been have a difference from conventional preoperative imaging in 42 patients (64.6%) as respect to the number, size, site of the lesions and degree of cirrhosis. This lead to change of decision intraoperatively from type of operation which planned preoperatively in 28 patients (59.5%) (Table 2 and 3). This decision was based upon an attending surgeon’s judgment on one of two primary factors: (1) the extent of neoplastic disease, and (2) the severity of nodular cirrhosis. Histopathologic examination of the resection specimen shows (HepatoCellular Carcinoma in 21 cases, Focal Nodular Hyperplasia in one patient, and Hepatocellular adenomain in one patient). The mean hospital stay was 5.14 days in laparoscopic resection group, while, in laparoscopic RFA group was 3.07 days, and in open surgery group was 6.62 days. The incidence of postoperative complications in Laparoscopic resection group was 35%, Laparoscopic RFA group was 27%, Open RFA and MVA group was 100%, and Open resection group was 60% (Table 2) Post-operative fellow up for 3 months with triphasic CT and alpha FP in all patients show no recurrence.
| Type of operation | Number of patients | |
| 1 | Laparoscopic resection | 12 |
| 2 | Laparoscopic RFA | 33 |
| 3 | Open RFA | 7 |
| 4 | Open microwave ablation | 2 |
| 5 | Open resection | 8 |
| 6 | Combined of laparoscopic resection and ablation | 2 |
| 7 | Combined of open resection and ablation | 1 |
| Total | 65 |
Table 2: Shows the type of operation and number of patients.
| Planned type of operation preoperatively | Decision intraoperatively | Number of patients |
| Laparoscopic resection or RFA | Open surgery (RFA, microwave, resection) | 18 |
| Laparoscopic resection | Laparoscopic RFA | 6 |
| Laparoscopic RFA | Laparoscopic resection | 2 |
| Laparoscopic RFA or resection | Combined by laparoscopy | 2 |
| Total | 28 |
Table 3: Show the planned type of operation and changed decisions.
Discussion
Solid visceral organs such as the liver pose a significant challenge to the laparoscopic surgeon because they have a soft parenchyma richly interspersed with vasculature [7]. Laparoscopic liver resection was first reported in the early 1990s for partial resection of segment 6 for a 6 cm focal nodular hyperplasia and wedge resection of segment 5 for colorectal liver metastases [8]. The effectiveness of laparoscopic instrumentation in maintaining a haemostatic, clear operative field has been well documented using different modalities of instruments such as LigaSure device [9]. Since then, the number of reported cases of laparoscopic liver resection has increased dramatically, especially over the last 5 years [10]. In this study we did used laparoscopic Habib™ 4X rediofrequency needle for hepatic resections. Although some surgeons are still skeptical about the oncological curative potential of laparoscopic surgery and evaluation of the long-term prognosis is required to justify the minimally invasive approaches for hepatic malignancies, several specialized centers have expanded the indications of laparoscopic hepatectomy from benign tumors to malignant tumors, including HCC [11] and from wedge resection of the anterolateral segments to major hepatectomy or resection of the posterosuperior segments, such as segment 8, 7, or 1 [12,13]. Liver resections, in our series even the most minor ones, in cirrhotic patients carried out as non anatomical resection with minor complications such as minimal collection. The aim of laparoscopic resection in cirrhotic patients was to reduce postoperative complications [14]. The most suitable candidates among HCC patients for laparoscopic hepatectomy are, in general, those with solitary lesions measuring 5 cm or less in diameter, located in the peripheral segments [15]. Several surgeons advocate laparoscopic resection for HCC, especially that in a cirrhotic liver, as the laparoscopic approach might offer an improvement, as has been suggested by several reports [16]. Possible reasons are the reduction of the parietal damage in the abdomen, which avoids interruption of large collateral veins and the exposure of abdominal viscera, with the dual benefit of less need for fluid infusion and improved reabsorption of ascites, the less liver mobilization is required [17]. This may be associated with reductions in postoperative pain and hospital stay, reduced peritoneal adhesions, and an earlier return to previous activity. A cosmetic advantage is also clear because of the absence of long abdominal incisions, and this should be taken into account, especially in young women. Patients who may require repeat procedures, such as repeat hepatectomy or subsequent transplantation, may benefit from an easier reoperation [18]. There is a debate about the specific risks of tumor seeding during laparoscopic surgery. Early attempts at laparoscopic resection of cancers were associated with high numbers of abdominal metastases, especially at port sites, but also in the peritoneal cavity [19]. The potential mechanisms for tumor seeding include direct contamination by technical hepatectomy or resection of the posterosuperior segments, such as segment 8, 7, or 1 [12,13]. Liver resections, in our series even the most minor ones, in cirrhotic patients carried out as non-anatomical resection with minor complications such as minimal collection. The aim of laparoscopic resection in cirrhotic patients was to reduce postoperative complications [14]. The most suitable candidates among HCC patients for laparoscopic hepatectomy are, in general, those with solitary lesions measuring 5 cm or less in diameter, located in the peripheral segments [15]. Several surgeons advocate laparoscopic resection for HCC, especially that in a cirrhotic liver, as the laparoscopic approach might offer an improvement, as has been suggested by several reports [16]. Possible reasons are the reduction of the parietal damage in the abdomen, which avoids interruption of large collateral veins and the exposure of abdominal viscera, with the dual benefit of less need for fluid infusion and improved reabsorption of ascites, the less liver mobilization is required [17]. This may be associated with reductions in postoperative pain and hospital stay, reduced peritoneal adhesions, and an earlier return to previous activity. A cosmetic advantage is also clear because of the absence of long abdominal incisions, and this should be taken into account, especially in young women. Patients who may require repeat procedures, such as repeat hepatectomy or subsequent transplantation, may benefit from an easier reoperation [18]. There is a debate about the specific risks of tumor seeding during laparoscopic surgery. Early attempts at laparoscopic resection of cancers were associated with high numbers of abdominal metastases, especially at port sites, but also in the peritoneal cavity [19]. The potential mechanisms for tumor seeding include direct contamination by technical from conventional preoperative imaging in 47 patients (72.3%) as respect to the number, size, site of the lesions and degree of cirrhosis [20-23]. This lead to change of decision intraoperatively from type of operation which planned preoperatively in 28 patients (43%). Our results match the work done by Bismuth and his colleagues on 210 patients with primary and secondary hepatic malignancies, they reported that intraoperative ultrasound provided additional information in 35% of cases and changed the operative plan in 20% [24]. In this study, the IOUS detected an extra-hepatic focal lesion which treated simultaneously. Montorsi et al. [25], reported on 68 patients evaluated by IOLUS revealed new malignant hepatic lesions in 15 patients (22%) not detected by Pre-laparoscopic diagnostic workup with extracorporeal ultrasound and Lipiodol or spiral CT which was considered the best procedure available. Of the 68 patients evaluated by IOLUS, 39 were considered to have a solitary HCC before IOLUS, but in five of these patients (13%) new malignant nodules were identified. However, only one (6%) of 16 patients in whom the main tumor was considered to be solitary and 2 cm or less in diameter had multicentric HCC. Soliman et al. [26], reported on 55 patients initially scheduled for hepatic resection, the decision for surgical resection was altered in 14 patients (25.45%), which were understated by the pre-operative imaging techniques and therefore would not benefit from surgical resection.
In conclusion, Laparoscopic inspection combined with a meticulously performed laparoscopic ultrasound shows great effect in detecting the features that may be lacking with the current preoperative imaging techniques as greater accuracy and better definition of the location and size of HCC lesions relative to the liver anatomy and degree of cirrhosis. In our experience, it has greatly contributed to the accurate staging of HCC in liver cirrhosis and has aided in intraoperative decision making.
References
- Weitz J, D'Angelica M, Jarnagin W, Gonen M, Fong Y, et al. (2004) Selective use of diagnostic laparoscopy prior to planned hepatectomy for patients with hepatocellular carcinoma. Surgery 135: 273-281.
- Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362: 1907-1917.
- Deuffic S, Poynard T, Buffat L, Valleron AJ (1998) Trends in primary liver cancer. Lancet 351: 214-215.
- Seleem MI, Gerges SS, Elkhouly AA, El-wakeel BA, Barbary MH (2012) Laparoscopic radiofrequency thermal ablation of hepatocellular carcinoma in liver cirrhosis patients. Gastroentrology Research 5: 232-235.
- Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250: 831-841.
- Pang YY (2002) The Brisbane 2000 Terminology of Liver Anatomy & Resections. Hepato-Pancrea to Biliary Association 2: 333-339.
- GOLDSMITH NA, WOODBURNE RT (1957) The surgical anatomy pertaining to liver resection. Surg Gynecol Obstet 105: 310-318.
- Gagner MRM, Dubuc J (1992) Laparoscopic partial hepatectomy for liver tumor. Surgical Endoscopy 6: 99.
- Constant DL, Slakey DP, Campeau RJ, Dunne JB (2005) Laparoscopic nonanatomic hepatic resection employing the LigaSure device. JSLS 9: 35-38.
- Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250: 831-841.
- Kazaryan AM, Pavlik Marangos I, Rosseland AR, Røsok BI, Mala T, et al. (2010) Laparoscopic liver resection for malignant and benign lesions: ten-year Norwegian single-center experience. Arch Surg 145: 34-40.
- Cho JY, Han HS, Yoon YS, Shin SH (2008) Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc 22: 2344-2349.
- Yoon YS, Han HS, Cho JY, Ahn KS (2010) Total laparoscopic liver resection for hepatocellular carcinoma located in all segments of the liver. Surg Endosc 24: 1630-1637.
- Bruix J, Castells A, Bosch J, Feu F, Fuster J, et al. (1996) Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 111: 1018-1022.
- Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, et al. (2009) The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 250: 825-830.
- Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, et al. (2009) Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. J Hepatobiliary Pancreat Surg 16: 433-438.
- Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, et al. (2007) “Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results,” Surgical Endoscopy 21: 2004-2011.
- Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, et al. (2000) Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 232: 753-762.
- Johnstone PA, Rohde DC, Swartz SE, Fetter JE, Wexner SD (1996) Port site recurrences after laparoscopic and thoracoscopic procedures in malignancy. J Clin Oncol 14: 1950-1956.
- Neuhaus SJ, Texler M, Hewett PJ, Watson DI (1998) Port-site metastases following laparoscopic surgery. Br J Surg 85: 735-741.
- Poulin EC, Mamazza J, Schlachta CM, Grégoire R, Roy N (1999) Laparoscopic resection does not adversely affect early survival curves in patients undergoing surgery for colorectal adenocarcinoma. Ann Surg 229: 487-492.
- Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, et al. (2009) The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg 250: 772-782.
- Pai M, Navarra G, Ayav A, Sommerville C, Khorsandi SK, et al. (2008) Laparoscopic Habib 4X: a bipolar radiofrequency device for bloodless laparoscopic liver resection. HPB (Oxford) 10: 261-264.
- Bismuth H, Castaing D, Garden OJ (1987) The use of operative ultrasound in surgery of primary liver tumors. World J Surg 11: 610-614.
- Montorsi M, Santambrogio R, Bianchi P, Opocher E, Cornalba GP, et al. (2001) Laparoscopy with laparoscopic ultrasound for pretreatment staging of hepatocellular carcinoma: a prospective study. J Gastrointest Surg 5: 312-315.
- Osama Soliman H, Samir Gad Z, Ahmed Mostafa MA, Mohamed Farahat A, Naglaa MA, et al. (2011). Laparoscopy with laparoscopic ultrasound for pretreatment staging of hepatic focal lesions: A prospective study. J Egypt Natl Canc Inst 23: 141-145.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15711
- [From(publication date):
November-2013 - Nov 22, 2025] - Breakdown by view type
- HTML page views : 11023
- PDF downloads : 4688