Review Article Open Access
Role and Progression of Radiotherapy for Locally Advanced Esophageal Cancer
Takeo Takahashi*, Keiichiro Nishimura and Takafumi Yamano
Department of Radiation Oncology, Saitama Medical Center, Saitama Medical University, Japan
- Corresponding Author:
- Takeo Takahashi, MD, PhD
Department of Radiation Oncology
Saitama Medical Center
Saitama Medical University
1981, Kamoda, Kawagoe
Saitama 350-8550, Japan
Tel: +81-49-228-3441
Fax: +81-49-228-3753
E-mail: taketaka@saitama-med.ac.jp
Received Date: May 20, 2013; Accepted Date: July 03, 2013; Published Date: July 05, 2013
Citation: Takahashi T, Nishimura K, YAmano T (2013) Role and Progression of Radiotherapy for Locally Advanced Esophageal Cancer. J Gastroint Dig Syst S1:005. doi: 10.4172/2161-069X.S1-005
Copyright: © 2013 Takahashi T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Radiotherapy plays an important role in the treatment of locally advanced esophageal cancer. And, definitive chemoradiotherapy is widely accepted treatment methods for advanced esophageal cancer. Radiation dose-escalation has failed to improve local control or survivals. However, irradiation techniques have been advancing markedly. 3-dimensional radiotherapy, intensity modulated radiotherapy (IMRT), and particle beam therapy is a highly precise radiotherapy in which the dose distribution can be fitted according to the shape of tumor. Future Directions will evaluate the dose-escalation using highly precise radiotherapy and adequate radiation field for locally advanced radiotherapy.
Keywords
Radiotherapy; Esophageal cancer; Chemoradiotherapy; 3-dimensional radiotherapy; Intensity modulated radiotherapy
Introduction
Esophageal cancer is often discovered at advanced stages, and is still associated with a poor prognosis. In the United States, approximately 17,360 new cases were diagnosed and 15,070 patients died of esophageal cancer in 2012 [1]. In Japan, a total of 5,066 cases were registered and more than 90% of esophageal cancer was squamous cell carcinoma [2]. In Europe and America, the rate of adenocarcinoma has risen as a result of increases in obesity and gastroesophageal reflux disease [3]. For superficial esophageal cancer, endoscopic mucosal resection is widely accepted as curative treatment option. On the other hand, there are 2 main curative treatments of esophageal cancer: surgery and radiotherapy for locally advanced esophageal cancer [4-6]. Anatomically, the esophagus is made up of squamous epithelium, and the serosa is absent in the wall structure. Accordingly, esophageal cancer readily infiltrates the adjacent great vessel (inferior vena cava), trachea, and primary bronchus, for which the application of radical surgery is difficult in many cases. Moreover, the range of advancement of lymph node metastasis has a decisive influence on deciding on a therapeutic policy for esophageal cancer. Improvement of the therapeutic outcome of surgery by 3-field lymphadenectomy has been observed. In radiotherapy, a therapeutic strategy setting an irradiation field in consideration of the ranges of local advancement and lymph node metastasis, optimal dose, and dose distribution is necessary.
Current State of Radiotherapy for Esophageal Cancer
The Radiation Therapy Oncology Group (RTOG) reported that the therapeutic outcome of chemoradiotherapy was more favorable than that of radiotherapy alone in esophageal cancer patients [7]. In a clinical study performed in Europe, the therapeutic outcome of the patients with esophageal squamous cell carcinoma was compared between those treated with definitive chemoradiotherapy followed by surgery and those treated with chemoradiotherapy alone, and it was comparable between the groups [8,9].
In Japan, more than 90 % of esophageal cancer is histologically squamous cell carcinoma, which is relatively radiosensitive. On the other hand, in western countries, one half had adenocarcinoma of the esophagus. However, RTOG 85-01 showed there were no statistical differences in survival in related to histology in patients treated with chemoradiotherapy. Data to support different treatment regimens based on histology are limited. Ohtsu et al. [10] reported that chemoradiotherapy for stage II-III esophageal squamous cell carcinoma setting a wide irradiation field corresponding to 3-field lymphadenectomy including the supraclavicular region over the upper abdominal lymph node, termed ‘super long T’, achieved an outcome equivalent to that of surgical treatment [10,11]. However, in this treatment method, chronic injury accompanying the wide irradiation field was problematic, and severe pericarditis and pleurisy occurred [12]. In current clinical studies on the current radiotherapy for esophageal cancer, 3-4 portals, not anteroposterior opposing portals, are used for irradiation. Three-dimensional (3D)-conformal radiotherapy improves the dose distribution in lesions and enables dose escalation. In addition, it reduced exposure of the lung and heart. The important point to decide on an irradiation field is accurate delineation of the target volume. In radiotherapy for esophageal cancer, delineations of the primary site of esophageal cancer and metastatic lymph node are essential. Regarding lymph nodes, metastasis was noted in about 40% of surgical cases even when the tumor size was smaller than 5 mm [13]. Since it is difficult to identify lymph node metastasis smaller than 5 mm even through FDGPET/ CT is used, clinical judgment is necessary, in addition to judgment based on the size and functional imaging findings of lymph nodes.
Current State and Future Prospects of Chemoradiotherapy
Definitive chemoradiotherapy for locally advanced esophageal cancer has been widely performed. The standard treatment is surgery due to the current level of treatment, but chemoradiotherapy is the second radical treatment following surgery. Since chemoradiotherapy was demonstrated to be superior to radiotherapy alone in a randomized controlled clinical study for esophageal cancer [14], many studies on chemoradiotherapy for esophageal cancer have been reported (Table 1). Based on the positive results of the RTOG 85-11 trial, definitive CRT might be an option for esophageal cancer patients. Many researchers reported that the rate of a complete response (CR) to chemoradiotherapy was about 60%, and the local control rate was about 40-45% [10]. However, because of high local and distant failure rates after definitive CRT, new approaches, such as the intensification of CRT and dose escalation of radiotherapy, have been attempted. To improve the therapeutic outcome, it is necessary to improve local control and reduce damage. The important point to reduce radiation-induced damage is setting of an appropriate irradiation field. Currently, exposure of the heart in treatment of the middle and lower esophagus can be decreased using 3-4 portals, which is considered to lead to reduction of chronic adverse effect. Regarding improvement of local control, it is necessary to investigate the dose of radiotherapy. Zhang et al. showed that highdose radiotherapy and favorable local tumor control were related to improved survival [15]. Minsky et al. [16] showed that concurrent high-dose (66 Gy/ 33 fractions) chemoradiotherapy provided longterm local tumor control in stage IIA-III esophageal cancer, and found that patients with squamous cell carcinomas had the same survival rate as those with adenocarcinomas. However, they did not observe a significant association between local control and survival. According to the INT 0123 study, a dose of 64.8 Gy is not superior to 50.4 Gy for esophageal squamous cell carcinoma [16]. Wu et al. [17] reported the results of radiotherapy alone at 66 Gy employing 3D-CRT, in which the local control rate was not satisfactory, showing the necessity of investigating dose escalation by combination with chemotherapy for squamous cell carcinoma of esophagus [17]. In the randomized RTOG trial, lung cancer was irradiated at the standard treatment dose, 60 Gy, and an increased dose, 74-Gy, and the outcome was poor in the 74-Gy group in interim analysis. Although it is necessary to investigate the details, such as the incidence of disorders, we should investigate dose escalation in consideration of the range of the irradiation field. The CR and local control rates of esophageal cancer after chemoradiotherapy are still not satisfactory. To further improve the local control rate, establishment of an appropriate irradiation field and modification of the irradiation method, such as dose escalation, are necessary. In chemoradiotherapy for lung cancer, involved-field irradiation omitting preventive irradiation of elective lymph nodes is becoming the standard. Zhao reported that the incidence of lymph node recurrence outside the irradiation field was low in 3D-CRT-treated esophageal squamous cell carcinoma patients, and no significant correlation was noted between the omission of elective nodal irradiation and recurrence in the lymph node region [18]. It has been reported that no significant difference was noted in the 3-year overall survival or local control rate between the involved-field and elective nodal irradiation groups in 3D-CRT for esophageal squamous cell carcinoma [19].
| study | Radiation dose | Chemotherapy | Median survival | 2-year survival | 5-year survival | local recurrence |
|---|---|---|---|---|---|---|
| (Gy) | (mo) | (%) | (%) | (%) | ||
| Herskovic [14] | 50 | CDDP+5FU | 14.1 | 38% | 26 | 46 |
| Hironaka and Ohtsu [11] | 60 | CDDP+5FU | 33 | 49(3-year) | 46 | |
| Stahl [9] | 40(+Surgery) | CDDP+5FU+Etoposide | 16.4 | 39.9 | 31.3(3-year) | |
| 65 | CDDP+5FU+Etoposide | 14.9 | 35.4 | 24.4(3-year) | 51 | |
| Minsky [16] | 50.4 | CDDP+5FU | 18.1 | 40 | 52 | |
| 64.8 | CDDP+5FU | 13 | 31 | 56 |
Table 1: Results from combined radiotherapy and chemotherapy as primary therapy for esophageal cancer.
Advanced Technologies of Radiotherapy for Esophageal Cancer
Reduction of the irradiated dose to organs at risk by concentrating irradiation on the target volume using Intensity-Modulated Radiotherapy (IMRT) has been attempted in patients with prostate adenocarcinoma and head-and-neck cancers, clarifying the clinical usefulness of IMRT, and reports on the results of IMRT applied for lung and esophageal cancers started to appear. The usefulness for headand- neck cancers has been clarified, particularly for nasopharyngeal cancer, and exposure of the organs at risk, particularly the spinal cord and salivary gland, can be reduced. In the planning of esophageal cancer treatment, it is difficult to prepare a favorable dose distribution employing conventional radiotherapy because the cervical and upper thoracic esophagus is very close to the Gross Tumor Volume (GTV) and organs at risk including the spinal cord, and a similar condition is also noted in thoracic esophageal cancer cases with markedly enlarged mediastinal lymph node metastasis. IMRT is capable of irradiating the target volume at a homogenous dose, through which normal tissue exposure can be reduced to below the tolerance dose. IMRT may be more beneficial with regard to decreasing normal tissue exposure than 3-D radiotherapy. Since IMRT is basically combined with chemotherapy, a therapeutic strategy in consideration of adverse effects on the lung is necessary.
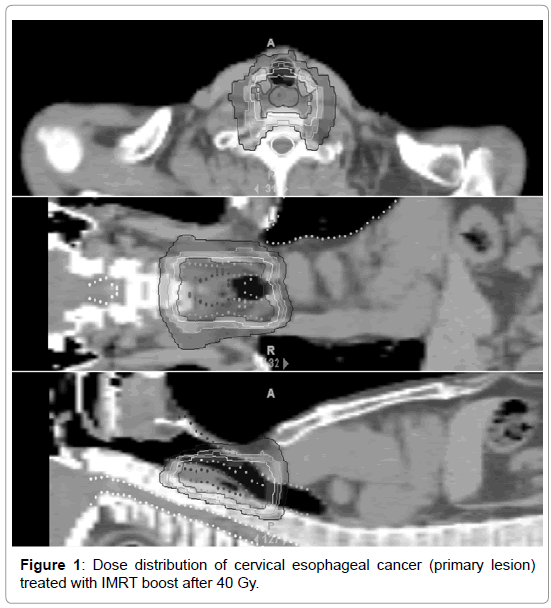
In IMRT, the dose distribution is prepared corresponding to the tumor shape by inverse planning changing the beam intensity in each direction in the irradiation field, being different from that in 3D-CRT (Figure 1). Clinical investigation of whether a localized irradiation field is sufficient or inclusion of a sufficient preventive region in the irradiation field is necessary is awaited [20,21] (Figure 1).
Currently, the regional lymph node region is generally included in the irradiation field in chemoradiotherapy in Japan, but preparation of an irradiation field is difficult in many cases of thoracic esophageal cancer if the regional lymph node area is wide, and it is likely that extensive lymph node metastases are present in a wide area from the supraclavicular fossa over the upper abdominal region. When the irradiation field is long in the cranio-caudal direction, the low dose area rate in the lung field may increase in IMRT, compared to that in the conventional irradiation method, and the risk of radiation pneumonitis may increase in patients concomitantly treated with chemotherapy. It has been reported that, when the lung volume irradiated at 20 Gy (V20) exceeds 30% in conventional chemoradiotherapy, the risk of radiation pneumonitis increases [22]. This index is very useful for lung cancer, and it is also applicable for esophageal cancer. Exposure of the heart and coronary artery is further reduced using IMRT, compared to that in 3D-CRT [23].
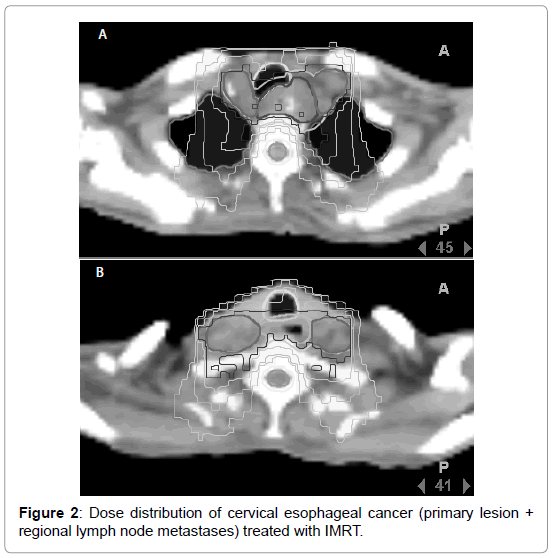
At present, cervical and upper thoracic esophageal cancers may be appropriate indications of IMRT. The dose distribution in the cervical esophagus is shown in Figure 2. Fenkell et al. reported that, for cervical esophageal cancer, IMRT is superior to 3D-CRT in concentrating the dose to the planning target volume (PTV) and homogeneity, and reduction of normal tissue exposure is also possible [24]. Zhang et al. compared 3D-CRT and IMRT of upper thoracic esophageal cancer, and observed that homogeneity of the dose in the irradiation field was favorable in IMRT, and the volume of the lung irradiated at 10 Gy or higher was small [25]. The prescription dose is determined based on that for the center of the region to be irradiated in conventional radiotherapy, whereas it is determined by 95% of the dose in highly precise radiotherapy including IMRT. Therefore, the conformity of the dose with the target volume is superior to the conventional irradiation method.
To perform IMRT, it is necessary to precisely maintain the positioning accuracy, for which evaluation of the respiratory movement of the esophagus is necessary. In a study using 4D-CT, respiratory movement of the lower thoracic esophagus was significantly larger than that of the cervical esophagus, and an about 10-mm movement in the cranio-caudal direction was noted in lower esophageal cancer patients, suggesting that the PTV and internal target volume should be carefully set in lower esophageal cancer cases. To perform highly precise radiotherapy, accurate delineation of the target volume and high positioning accuracy are essential.
Proton-beam therapy is expected to become a treatment for esophageal cancer in the near future. Tsujii and Koyama [26] reported that high-dose irradiation of esophageal cancer was possible using proton-beam therapy. Mizumoto reported that 78% of locally advanced esophageal cancer patients treated with proton-beam therapy (median dose: 79 GyE) showed a complete response, and the 5-year local control rate was 38% [27]. Lin et al. performed proton-beam therapy at 50.4 Gy, and achieved a pathological complete response (pCR) and near pCR in 50% of patients [28]. They suggested that the pathological response and clinical outcomes are encouraging. Welsh showed that exposures of the heart, lung, and liver could be reduced in intensity-modulated proton therapy compared to those in IMRT in patients with locally advanced distal esophageal cancer [29], and Lin also reported that the incidence of cardiac death was higher in the 3D-CRT than in the IMRT group [30], suggesting that highly precise radiotherapy with reduced normal tissue damage can be performed for esophageal cancer.
To improve the therapeutic outcome, investigation of a novel chemotherapy regimen for esophageal cancer is also necessary. Tanaka et al. reported that the rate of a response to a preoperative DCF regimen (5-fluorouracil and cisplatin plus docetaxel) was favorable (80%) and the survival rate was improved in patients with esophageal cancer accompanied by extended lymph node metastases [31]. The usefulness of thermotherapy for gastrointestinal cancers has also recently been reevaluated. It is possible that preoperative chemoradiotherapy is useful to conserve the larynx in surgery of the cervical esophagus [32]. Suzuki demonstrated that chemoradiotherapy for esophageal squamous cell carcinoma induced tumor antigen-specific T-cell responses. Therefore, the development of novel tumor-specific immunotherapy for combination with chemoradiotherapy is expected [33].
Conclusion
Chemo radiotherapy is an effective treatment method, as well as surgery, for locally advanced esophageal cancer. To improve the therapeutic outcome, establishment of an appropriate irradiation field and selection of an appropriate irradiation dose reducing damaging are necessary using high-precision devices. In addition, the development of novel chemotherapy and immunotherapy for combination is expected.
References
- Almhanna K, Shridhar R, Meredith KL (2013) Neoadjuvant or adjuvant therapy for resectable esophageal cancer: is there a standard of care? Cancer Control 20: 89-96.
- Ozawa S, Tachimori Y, Baba H, et al. (2012) Comprehensive registry of esophageal cancer in Japan, 2004. Esophagus 9: 75-98.
- Shridhar R, Almhanna K, Meredith KL, Biagioli MC, Chuong MD, et al. (2013) Radiation therapy and esophageal cancer. Cancer Control 20: 97-110.
- Okawa T, Kita M, Tanaka M, Ikeda M (1989) Results of radiotherapy for inoperable locally advanced esophageal cancer. Int J Radiat Oncol Biol Phys 17: 49-54.
- Sun DR (1989) Ten-year follow-up of esophageal cancer treated by radical radiation therapy: analysis of 869 patients. Int J Radiat Oncol Biol Phys 16: 329-334.
- Yamada S, Nemoto K, Ariga H, Jingu K (2012) Radiotherapy for esophageal cancer in Japan. Esophagus 9: 66-74.
- Cooper JS, Guo MD, Herskovic A, Macdonald JS, Martenson JA Jr, et al. (1999) Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group. JAMA 281: 1623-1627.
- Bedenne L, Michel P, Bouché O, Milan C, Mariette C, et al. (2007) Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 25: 1160-1168.
- Stahl M, Stuschke M, Lehmann N, Meyer HJ, Walz MK, et al. (2005) Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23: 2310-2317.
- Ohtsu A, Boku N, Muro K, Chin K, Muto M, et al. (1999) Definitive chemoradiotherapy for T4 and/or M1 lymph node squamous cell carcinoma of the esophagus. J Clin Oncol 17: 2915-2921.
- Hironaka S, Ohtsu A, Boku N, Muto M, Nagashima F, et al. (2003) Nonrandomized comparison between definitive chemoradiotherapy and radical surgery in patients with T(2-3)N(any) M(0) squamous cell carcinoma of the esophagus. Int J Radiat Oncol Biol Phys 57: 425-433.
- Ishikura S, Nihei K, Ohtsu A, Boku N, Hironaka S, et al. (2003) Long-term toxicity after definitive chemoradiotherapy for squamous cell carcinoma of the thoracic esophagus. J Clin Oncol 21: 2697-2702.
- Kato H, Kuwano H, Nakajima M, Miyazaki T, Yoshikawa M, et al. (2002) Comparison between positron emission tomography and computed tomography in the use of the assessment of esophageal carcinoma. Cancer 94: 921-928.
- Herskovic A, Martz K, al-Sarraf M, Leichman L, Brindle J, et al. (1992) Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med 326: 1593-1598.
- Zhang Z, Liao Z, Jin J, Ajani J, Chang JY, et al. (2005) Dose-response relationship in locoregional control for patients with stage II-III esophageal cancer treated with concurrent chemotherapy and radiotherapy. Int J Radiat Oncol Biol Phys 61: 656-664.
- Minsky BD, Pajak TF, Ginsberg RJ, Pisansky TM, Martenson J, et al. (2002) INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol 20: 1167-1174.
- Wu KL, Chen GY, Xu ZY, Fu XL, Qian H, et al. (2009) Three-dimensional conformal radiation therapy for squamous cell carcinoma of the esophagus: a prospective phase I/II study. Radiother Oncol 93: 454-457.
- Zhao KL, Ma JB, Liu G, Wu KL, Shi XH, et al. (2010) Three-dimensional conformal radiation therapy for esophageal squamous cell carcinoma: is elective nodal irradiation necessary? Int J Radiat Oncol Biol Phys 76: 446-451.
- Ma JB, Song YP, Yu JM, Zhou W, Cheng EC, et al. (2011) Feasibility of involved-field conformal radiotherapy for cervical and upper-thoracic esophageal cancer. Onkologie 34: 599-604.
- Onozawa M, Nihei K, Ishikura S, Minashi K, Yano T, et al. (2009) Elective nodal irradiation (ENI) in definitive chemoradiotherapy (CRT) for squamous cell carcinoma of the thoracic esophagus. Radiother Oncol 92: 266-269.
- Nemoto K, Yamada S, Hareyama M, Nagakura H, Hirokawa Y (2001) Radiation therapy for superficial esophageal cancer: a comparison of radiotherapy methods. Int J Radiat Oncol Biol Phys 50: 639-644.
- Tsujino K, Hirota S, Endo M, Obayashi K, Kotani Y, et al. (2003) Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys 55: 110-115.
- Kole TP, Aghayere O, Kwah J, Yorke ED, Goodman KA (2012) Comparison of heart and coronary artery doses associated with intensity-modulated radiotherapy versus three-dimensional conformal radiotherapy for distal esophageal cancer. Int J Radiat Oncol Biol Phys 83: 1580-1586.
- Fenkell L, Kaminsky I, Breen S, Huang S, Van Prooijen M, et al. (2008) Dosimetric comparison of IMRT vs. 3D conformal radiotherapy in the treatment of cancer of the cervical esophagus. Radiother Oncol 89: 287-291.
- Zhang WZ, Chen ZJ, Li DR, Lin ZX, Li DS, et al. (2009) Dosimetric comparison between intensity-modulated radiotherapy and conformal radiotherapy for upper thoracic esophageal carcinoma. Ai Zheng 28: 1127-1131.
- Koyama S, Tsujii H (2003) Proton beam therapy with high-dose irradiation for superficial and advanced esophageal carcinomas. Clin Cancer Res 9: 3571-3577.
- Mizumoto M, Sugahara S, Nakayama H, Hashii H, Nakahara A, et al. (2010) Clinical results of proton-beam therapy for locoregionally advanced esophageal cancer. Strahlenther Onkol 186: 482-488.
- Lin SH, Komaki R, Liao Z, Wei C, Myles B, et al. (2012) Proton beam therapy and concurrent chemotherapy for esophageal cancer. Int J Radiat Oncol Biol Phys 83: e345-351.
- Welsh J, Gomez D, Palmer MB, Riley BA, Mayankkumar AV, et al. (2011) Intensity-modulated proton therapy further reduces normal tissue exposure during definitive therapy for locally advanced distal esophageal tumors: a doseimetric study. Int J Radiat Oncol Biol Phys 81: 1336-1342.
- Lin SH, Wang L, Myles B, Thall PF, Hofstetter WL, et al. (2012) Propensity score-based comparison of long-term outcomes with 3-dimensional conformal radiotherapy vs intensity-modulated radiotherapy for esophageal cancer. Int J Radiat Oncol Biol Phys 84: 1078-1085.
- Tanaka T, Kinoshita Y, Udagawa H, Ueno M, Ehara K, et al. (2012) Efficacy and safety of docetaxel/cisplatin/5-fluorouracil preoperative combination chemotherapy in esophageal cancer patients with extended lymph node metastases. Esophagus 9: 99-104.
- Takahashi T, Saitoh J, Okonogi N, et al. (2013) Role of hyperthermia in the treatment of gastrointestinal cancers. Ther Med 29: 25-36.
- Suzuki Y, Mimura K, Yoshimoto Y, Watanabe M, Ohkubo Y, et al. (2012) Immunogenic tumor cell death induced by chemoradiotherapy in patients with esophageal squamous cell carcinoma. Cancer Res 72: 3967-3976.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14529
- [From(publication date):
specialissue-2012 - Dec 04, 2025] - Breakdown by view type
- HTML page views : 9826
- PDF downloads : 4703