Reporting Results: Approaches have Implications for Prevention
Received: 08-Nov-2012 / Accepted Date: 14-Nov-2012 / Published Date: 18-Nov-2012 DOI: 10.4172/2161-1165.1000e108
159449In much of epidemiologic research we have focused on the precision of our methods, reducing bias, and uncovering the underlying truth of associations between exposures and disease. While others have written extensively about the approaches one can take to clarify writing so that it helps the reader interpret numbers and follow the results from a given study [1], less attention has been paid to the interpretation and communication of results beyond the academic journal setting. Yet, results from journal articles often appear in lay print media and web sites. Reporting of research results may thus inform their broader use. We know that publication of results alone, whether a single study, a systematic review, or guideline, does not itself lead to behaviour change among those in the community, health care providers, or policy makers [2-5].
Attention to how we present results may be one step we can take to speed translation of results into practice and so improve population health more quickly. As an example, we take the 1938 report by Pearl on smoking and longevity [6]. Using life table approaches, Pearl focused on the accuracy of the relation between habitual usage of tobacco and longevity. He constructed life tables form 2,094 non-users of tobacco; 2,814 moderate smokers, and 1,905 heavy smokers. Reporting data from age 30 to 95 he was able to show the survivorship of white males according to smoking habits. He concluded that smoking was “associated with an impairment of life duration”.
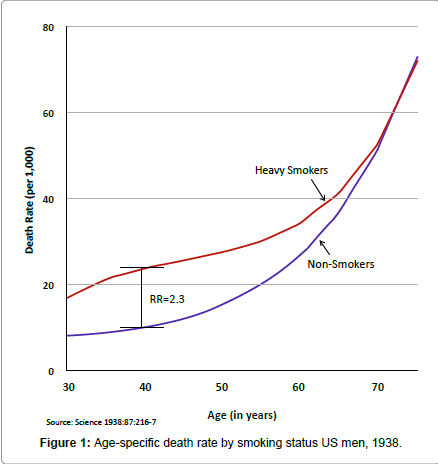
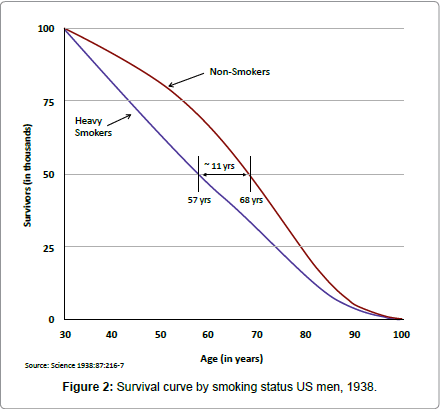
Using the data from his life table, we redraw the data as mortality curves. A relative risk of mortality for heavy smokers compared to nonsmokers ranges from 2.1 at age 30 to 2.3 at 40, and 1.8 at age 50 (Figure 1). This is consistent with recent estimates of current smokers versus non-smokers in the National Health Interview Survey from 1987 –2006, where relative risk of mortality for current smokers vs. never smokers was 2.3 to 3.1 [7]. Plotting the survival curves (Figure 2) we note that 50% of smokers are deceased at age 57 compared to mortality among non-smokers where 50% are decreased by age 68. Thus an 11- year greater life expectancy, on average, can be reported (inferred from these data).
For 80 years, epidemiology has refined the assessment of the impact of smoking on mortality and on specific diseases [8]. Yet the burden of smoking may be more clearly reported for public health impact by an 11-year shorter life expectancy, than merely a doubling in the risk of death at any given age. Since the public has poor understanding of their risk of death, doubling this poorly understood risk does not covey a message that is actionable or that warrants policy changes to remove the excess disease burden caused by smoking.
In the past, it could be argued that research results largely remained in the domain of scientific professionals. Today, data of all sorts are much more accessible, if not readily understandable, by huge swathes of the population. Should this place a greater burden on researchers to report not only accurate, detailed results but also results that are meaningful to groups outside their immediate research area?
The answer would seem a qualified “yes.” If research’s end goal is to seek out evidence that ultimately improves health and well-being, beginning to think of better ways to communicate these results in a broader, more effective manner is a shift in methods and publishing that is worth discussing. Of course, specificity and accuracy is key to solid science, but keeping an eye toward a more general, practical message in our research may not only help how our results are received but also how large an impact they ultimately have.
The benefits of prevention are often underestimated or not reported [9]. Refining our approaches to reporting data to convey the risks and benefits of prevention [10] is a priority as we move to act on what we already know [2].
References
- Mosteller F (1986) Writing about numbers. In: Bailar JC, ed Medical Uses of Statistics. NEJM Books.
- Colditz GA, Wolin KY, Gehlert S (2012) Applying what we know to accelerate cancer prevention. Sci Transl Med 4: 127rv4.
- Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, et al. (1998) Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ 317: 465-468.
- Colditz GA (2002) Disseminating research findings into public health practice. Cancer Causes Control 13: 503-504.
- Colditz G (2012) The promise and challenges of dissemination and implemtnation research. In: Brown RC, Colditz G, Proctor E, (eds) Dissemination and implementation reserch in health Translating science to practice. Oxford Univeristy Press: New York.
- Mehta N, Preston S (2012) Continued increases in the relative risk of death from smoking. Am J Public Health 102: 2181-2186.
- U.S. Department of Health and Human Services (2004) The health consequences of smoking: a report of the Surgeon General. Washington DC.
- Hemenway D (2010) Why we don't spend enough on public health. N Engl J Med 362: 1657-1658.
- Waters EA, Weinstein ND, Colditz GA, Emmons K (2006) Formats for improving risk communication in medical tradeoff decisions. J Health Commun 11: 167-182.
Citation: Colditz GA, Hank Dart SM (2012) Reporting Results: Approaches have Implications for Prevention. Epidemiol 2:e108. DOI: 10.4172/2161-1165.1000e108
Copyright: © 2012 Colditz GA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14220
- [From(publication date): 12-2012 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 9522
- PDF downloads: 4698