Research Article Open Access
Race and Triple Negative Breast Cancer
K P Siziopikou1* and M. Cobleigh21Department of Pathology, Northwestern University /Feinberg School of Medicine, Chicago, IL, USA
2Department of Medicine, Section of Medical Oncology, Rush University Medical Center, Chicago, IL, USA
- *Corresponding Author:
- Kalliopi P. Siziopikou, MD, PhD
Professor of Pathology
Director of Breast Pathology
Northwestern University/Feinberg School of Medicine
251 East Huron Street, Galter 7-132 O, Chicago, IL 60611
Tel: 312 926 6530
E-mail: p-siziopikou@northwestern.edu
Received Date: September 12, 2011; Accepted Date: November 14, 2011; Published Date: November 15, 2011
Citation: Siziopikou KP, Cobleigh M (2011) Race and Triple Negative Breast Cancer. J Clinic Experiment Pathol S1:001 doi: 10.4172/2161-0681.S1-001
Copyright: © 2011 Siziopikou KP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Breast cancer is understood to represent not a single disease but a heterogeneous group of tumors with different biologic behavior, prognosis and response to treatment. Luminal A, luminal B, HER2 overexpressing, triple negative and basal subtypes of breast carcinomas are now considered distinct entities with unique biologic characteristics and clinical outcomes. Classic epidemiologic studies have also shown that race plays a role in the incidence and ultimate prognosis of breast cancer; specifically while the incidence of breast carcinomas is higher in Caucasian women, African-American patients have worse overall prognosis with higher breast cancer mortality rates. While the impact of socioeconomic and health care access factors is not to be dismissed, unique biologic characteristics in this patient population may play an important role in the difference in patient outcome. In this report we evaluated possible racial differences in the incidence of the basal subtype of triple negative breast carcinomas in a large cohort of consecutive breast cancer patients.
Introduction
A number of studies over the years have suggested that African– American women with breast cancer have a worse prognosis compared to Caucasian women. This difference is particularly evident among younger women diagnosed before the age of 50 [1,2]. While socioeconomic and health care access factors certainly play a role in worse survival rates in African-American women, unique biologic characteristics in this patient population may also be contributing in the observed differences in patient outcome.
Invasive breast carcinomas consist of a heterogeneous group of tumors with different biologic behavior, prognosis and response to treatment. The classic pathologic classification of breast carcinomas was recently redefined by gene microarray studies that identified distinct subtypes of breast carcinomas as follows: luminal A, luminal B, HER-2 overexpressing and basal [3-6]. These subtypes of breast carcinomas display different gene expression signatures and are associated with different clinical outcomes [4-6]. The tumors of the basal subtype of breast carcinomas express one or more of the basal cytokeratins (such as CK5/6, 14 or 17) and are histologically poorly differentiated, ERnegative, HER-2 negative ductal carcinomas with minimal or absent in situ component [7-10]. Basal subtype breast carcinomas comprise the majority of “interval” breast cancers presenting between screening mammograms and are associated with high proliferation rates and poor prognosis [3-5,11]. In addition, the majority of the BRCA1 associated breast carcinomas are thought to belong to the basal subtype of breast tumors [12-14]. We, and others, recently reported that ER-negative/ PR-negative/HER-2 negative (so called “triple negative”) breast tumors express epidermal growth factor receptor (EGFR), a member of the human epidermal growth factor family of transmembrane tyrosine kinases that activate a number of signaling pathways involved in cell proliferation and carcinogenesis [15-19]. Furthermore, a number of studies including our own, have suggested that the majority of these “triple negative”, EGFR positive tumors belong to the basal subtype and hypothesized that these tumors may be the subtype of breast carcinomas that could potentially benefit from EGFR-targeted therapeutic approaches [7,18,20-23].
Against this background, the objective of the current study was to evaluate possible racial differences in the incidence of these triplenegative/ EGFR-positive/basal subtype tumors in a large cohort of consecutive breast cancer patients.
Materials and Methods
Our study population consisted of 306 consecutive breast cancer patients. The age and race of patients and the histologic parameters of tumor type, grade and size at the time of diagnosis were recorded. The following breast cancer marker profile was obtained immunohistochemically on all patients (ER, Dako; PR, Dako; MIB- 1, Dako, EGFR, Dako, CK5/6, Zymed) and analyzed by quantitative image analysis (Chromavision, ACIS system). HER-2 amplification status was evaluated by FISH (PathVysion, Vysis).
Statistical analysis
The data were analyzed with cross tabulations and the chi-squared test was used as appropriate. P-values less than 0.05 were considered statistically significant.
Results
Correlation between race and breast tumor marker profile
Overall 61 African-American, 213 Caucasian, 5 Asian, 9 Hispanic and 18 other patients were recorded. African-American patients tended to be younger; 10/61 (16.4%) versus 15/213 (7%) were less than 40 years of age (p<0.01). African-American patients had ER-negative (30/61 versus 50/213, p<0.0005), PR-negative (41/61 versus 84/213, p<0.0005) tumors that were highly proliferative (36/61 versus 68/213 had MIB-1 values of >20%, p<0.001). In addition, most African-American patients had grade III tumors (67% versus 38%, p<0.01). No association with HER-2 gene amplification, tumor size or histologic subtype was observed. Furthermore, a much higher percentage of African-American patients expressed EGFR, 23/61 (37.7%) versus 46/213 ( 21.5%), p<0.03. Of interest, cytokeratin CK5/6 expression was high as well ( 12/57 versus 11/186, p<0.01), thus defined by immunohistochemistry to belong to the basal subtype of breast carcinomas. (Table 1).
| African-American (n=61) |
Caucasian (n=213) |
P value | |
|---|---|---|---|
| Age (<40 yo) | 10 | 15 | <0.01 |
| ER negative | 30 | 50 | <0.0005 |
| PR negative | 41 | 84 | <0.005 |
| Unfavorable MIB-1 (>20%) | 36 | 68 | <0.001 |
| High histologic grade (III) | 41 | 81 | <0.01 |
| EGFR expression | 23 | 46 | <0.003 |
| CK5/6 expression | 12 | 11 | <0.01 |
Table 1: Correlation between Race and Breast Tumor Marker Profile.
Correlation between race and triple negative/EGRF-positive phenotype
When patients were grouped by their ER-negative/PR-negative/ HER-2-negative (=triple negative)/EGFR-positive phenotype, more than double (16/61, 26%) of the African-American patients expressed this phenotype compared to only 22/213 (10.3%) of the Caucasian patients (p<0.02) (Table 2).
| Phenotype Present | Phenotype Absent | Total | |
|---|---|---|---|
| African-American | 16 (26%) | 45 (74%) | 61 |
| Caucasian | 22 (10%) | 191 (90%) | 213 |
P<0.02
Table 2: Correlation between Race and Triple Negative/EGFR-positive phenotype.
Correlation between race and triple negative/ basal phenotype
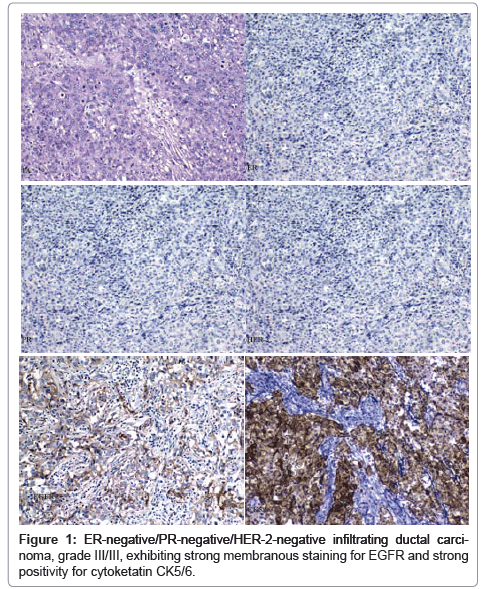
Of interest, when the incidence of the basal phenotype was examined, 19.6% (12/61) African-American patients expressed the ER-negative/PR-negative/HER-2-negative (=triple negative)/CK5/6- positive basal subtype phenotype compared to only 8% (17/213) of the Caucasian patients (p<0.007) (Table 3 and Figure 1).
| Phenotype Present | Phenotype Absent | Total | |
|---|---|---|---|
| African-American | 12 (20%) | 49 (80%) | 61 |
| Caucasian | 17 (8%) | 196 (92%) | 213 |
P<0.07
Table 3: Correlation between Race and Triple Negative/CK5/6(basal)-positive phenotype.
Discussion
Breast cancer is the most common malignancy and is second only to lung cancer as a cause of cancer related mortality of women in the United States [1]. African-American women have lower incidence of breast cancer than Caucasian women, yet are more likely to die of their disease as reported repeatedly by the National Cancer Surveillance Epidemiology and End Results (SEER) database, the Department of Defense database and many other studies [28-30]. These racial disparities in outcome have been attributed by many to socioeconomic factors, as well as access to care factors and cultural factors [31]. However, an increasing number of studies have reported racial differences in many pathologic prognostic factors and genetic factors (such as distinct BRCA1 and BRCA2 mutations) in these patients [32-34].
Following the recent redefinition of the classic pathologic classification of breast carcinomas by gene microarray studies that identified distinct subtypes of breast tumors, a number of investigators looked into the incidence of these subtypes and reported differences in different racial groups [2,24,27]. In a recently reported analysis of participants in the Carolina Breast Cancer study 64% of Caucasian patients had a luminal A breast cancer subtype compared with only 48% of African-American patients, 11% of Caucasian patients had a luminal B breast cancer subtype compared with 8% of African-American patients, 5% of Caucasian patients had a HER2 overexpressing breast cancer subtype compared with 7% of African-American patients, and only 11% of Caucasian patients had a basal breast cancer subtype compared with a 22% of African-American patients [24]. We reported previously that 64% of ER negative/PR negative/HER2 negative breast tumors express epidermal growth factor receptor (EGFR) and that 67% of this group belongs to the basal subtype of breast carcinomas [15,20]. EGFR is a member of the human epidermal growth factor family of transmembrane tyrosine kinases that activate a number of signaling pathways involved in cell proliferation and carcinogenesis [15-19]. Despite initial absence of promising results with the use of EGFR-targeted therapies in breast cancer, a growing number of studies suggested interactions of EGFR–mediated signaling and endocrine pathways [35,36]. We (and others) hypothesized that based on the high incidence of EGFR expression in basal subtype of breast carcinomas, these tumors could possibly be prime candidates for EGFR-targeted therapy.
In this study we aimed to evaluate the possible racial differences in the incidence of these triple negative/EGFR positive/basal subtype tumors in a large cohort of consecutive breast cancer patients. We report that the majority of African-American patients have ERnegative/ PR-negative, highly proliferative, poorly differentiated (grade III/III) breast carcinomas. In addition, these tumors tend to express EGFR and belong to the basal subtype of breast carcinomas that are traditionally associated with poor prognosis. Based on the high incidence of basal subtype, as well as EGFR expression in ER-negative/ PR-negative/HER-2-negative patients, we propose that triple negative patients are routinely tested for CK5/6 and EGFR expression and, within the appropriate medical context, informed decisions are made regarding follow-up genetic testing, given the known association of basal tumors with BRCA1 mutations.
These findings support the hypothesis, as other groups have suggested [24-27], that underlying biologic differences may contribute to the worse overall prognosis of breast carcinomas in African-American patients. A clinical trial of the EGFR-targeting inhibitor erlotinib in a metastatic setting in triple negative/EGFR positive African-American and Caucasian patients, coupled with pathology studies of molecular correlates of a possible effective response, has been recently completed and the results will be reported soon.
Acknowledgements
Conflict of interest statement: The authors of this paper have no conflicts of interest related to this work.
Ethical approval: There are no ethical conflicts. This work was based on review of existing records only.
References
- http://seer.cancer.gov, Bethesda, MD: National Cancer Institute.
- Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, et al. (2006) Race, breast cancer subtypes and survival in the Carolina Breast Cancer Study. JAMA 295: 2492-2502.
- Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, et al. (2000) Molecular portraits of human breast tumours. Nature 406: 747-752.
- van 't Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, et al. (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature 415: 530-536.
- Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, et al. (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. ProcNatlAcadSciUSA 98:10869-10874.
- Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, et al. (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 11: 5678-5685.
- Abd El-Rehim DM, Pinder SE, Paish CE, Bell J, Blamey RW, et al. (2004) Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 203: 661-671.
- Livasy CA, Karaca G, Nanda R, Tretiakova MS, Olopade OI, et al. (2006) Phenotypic evaluation of the basal-like subtype of invasive breast carcinoma. Mod Pathol 19: 264-271.
- Matos I, Dufloth R, Alvarenga M, Zeferino LC, Schmitt F (2005) p63, cytokeratin 5 and P-cadherin: three molecular markers to distinguish basal phenotype in breast carcinomas. Virchows Arch 447: 688-694.
- Bryan BB, Schnitt SJ, Collins LC (2006) Ductal carcinoma in situ with basal-like phenotype: a possible precursor to invasive basal-like breast cancer. Mod Pathol 19: 617-621.
- Collett K, Stefansson IM, Eide J, Braaten A, Wang H, et al. (2005) A basal epithelial phenotype is more frequent in interval breast cancers compared with screen detected tumors. Cancer Epidemiol Biomarkers Prev14: 1108-1112.
- Foulkes WD, Stefansson IM, Chappuis PO, Bégin LR, Goffin JR, et al. (2003) Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst 95: 1482-1485.
- Lakhani SR, Reis-Filho JS, Fulford L, Penault-Llorca F, van der Vijver M, et al. (2005) Prediction of BRCA1 status in patients with breast cancer using estrogen receptor and basal phenotype. Clin Cancer Res 11: 5175-5180.
- Palacios J, Honrado E, Osorio A, Cazorla A, Sarrió D, et al. (2005) Phenotypic characterization of BRCA1 and BRCA2 tumors based on a tissue microarray study with 37 immunohistochemical markers. Breast Cancer Res Treat 90: 5-14.
- Siziopikou KP, Ariga R, Proussaloglou KE, Gattuso P, Cobleigh M (2006) The challenging estrogen receptor-negative/ progesterone receptor-negative/HER-2-negative patient: a promising candidate for epidermal growth factor receptor-targeted therapy? Breast J 12: 360-362.
- Krause DS, Van Etten RA (2005) Tyrosine kinases as targets for cancer therapy. N Engl J Med 353:172-187.
- Pao W, Miller VA, et al. (2005) Epidermal growth factor receptor mutations, small-molecule kinase inhibitors, and non-small-cell lung cancer: current knowledge and future directions. J ClinOncol 23: 2556-2568.
- Sartor CI, Zhou H, Perou CM, Ethier SP. Basal-like breast tumor-derived cell lines are growth inhibited and radiosensitized by epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors. Breast Cancer Res Treat 2004; 88 Supplement S34.
- Cunliffe HE, Ringnér M, Bilke S, Walker RL, Cheung JM, et al. (2003) The gene expression response of breast cancer to growth regulators: patterns and correlation with tumor expression profiles. Cancer Res 63: 7158-7166.
- Siziopikou KP, Cobleigh M (2007) The basal subtype of breast carcinomas may represent the group of breast tumors that could benefit from EGFR-targeted therapies. Breast 16: 104-107.
- Green MR (2004) Targeting targeted therapy. N Engl J Med 350: 2191-2193.
- Spector NL, Xia W, Burris H , Hurwitz H, Dees EC, et al. (2005) Study of the biologic effects of lapatinib, a reversible inhibitor of ErbB1 and ErbB2 tyrosine kinases, on tumor growth and survival pathways in patients with advanced malignancies. J ClinOncol 23: 2502-2512.
- Lu C, Speers C, Zhang Y, Xu X, Hill J, et al. (2003) Effect of epidermal growth factor receptor inhibitor on development of estrogen receptor-negative mammary tumors. J Natl Cancer Inst 95: 1825-1833.
- O'Brien KM, Cole SR, Tse CK, Perou CM, Carey LA, et al. (2010) Intrinsic breast cancer subtypes, race and long-term survival in the Carolina Breast Cancer Study. Clin Cancer Res 16: 6100-6110.
- Goldson A, Henschke U, Leffall LD, Schneider RL (1981) Is there a genetic basis for the differences in cancer incidence between Afro-Americans and Euro-Americans? J Natl Med Assoc 73: 701-706.
- Gordon NH (2003) Socioeconomic factors and breast cancer in black and white Americans. Cancer Metastasis Rev 22: 55-65.
- Brawley OW (2010) Towards a better understanding of race and cancer. Clin Cancer Res 16: 5920-5922.
- Jatoi I, Becher H, Leake CR (2003) Widening disparity in survival between white and African-American patients with breast carcinoma treated in the US Department of Defense Healthcare system. Cancer 98: 894-899.
- Albain KS, Unger JM, Crowley JJ, Coltman CA Jr, Hershman DL (2009) Racial disparities in cancer survival among randomized clinical trials patients of the Southwest Oncology Group. J Natl Cancer Inst 101: 984-992.
- Newman LA, Griffith KA, Jatoi I, Simon MS, Crowe JP et al. (2006) Meta-analysis of survival of African American and white American patients with breast cancer: ethnicity compared with socioeconomic status. J ClinOncol 24: 1342-1349.
- Underwood SM (2003) Reducing the burden of cancer borne by African-Americans: if not now, when? CacnerEpidemiol Biomarkers Prev 12: 270s-276s.
- Ademuyiwa FO, Olopade OI (2003) Racial differences in genetic factors associated with breast cancer. Cancer Metastasis Rev 22: 47-53.
- Porter PL, Lund MJ, Lin MG, Yuan X, Liff JM, et al. (2004) Racial differences in the expression of cell cycle –regulatory proteins in breast carcinoma. Cancer 100: 2533-2542.
- Stark AT, Claud S, Kapke A, Lu M, Linden M, et al. (2005) Race modifies the association between breast carcinoma pathologic prognostic indicators and the positive status of HER-2/neu. Cancer 104: 2189-2196.
- Green MR (2004) Targeting Targeted therapy. N Engl J Med 350: 2191-2193.
- Lu C, Speers C, Zhang Y, Xu X, Hill J, et al. (2003) Effect of epidermal growth factor receptor inhibitor on development of estrogen receptor-negative mammary tumors. J Natl Cancer Inst 95: 1825-1833.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14395
- [From(publication date):
November-2011 - Dec 11, 2025] - Breakdown by view type
- HTML page views : 9714
- PDF downloads : 4681