Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
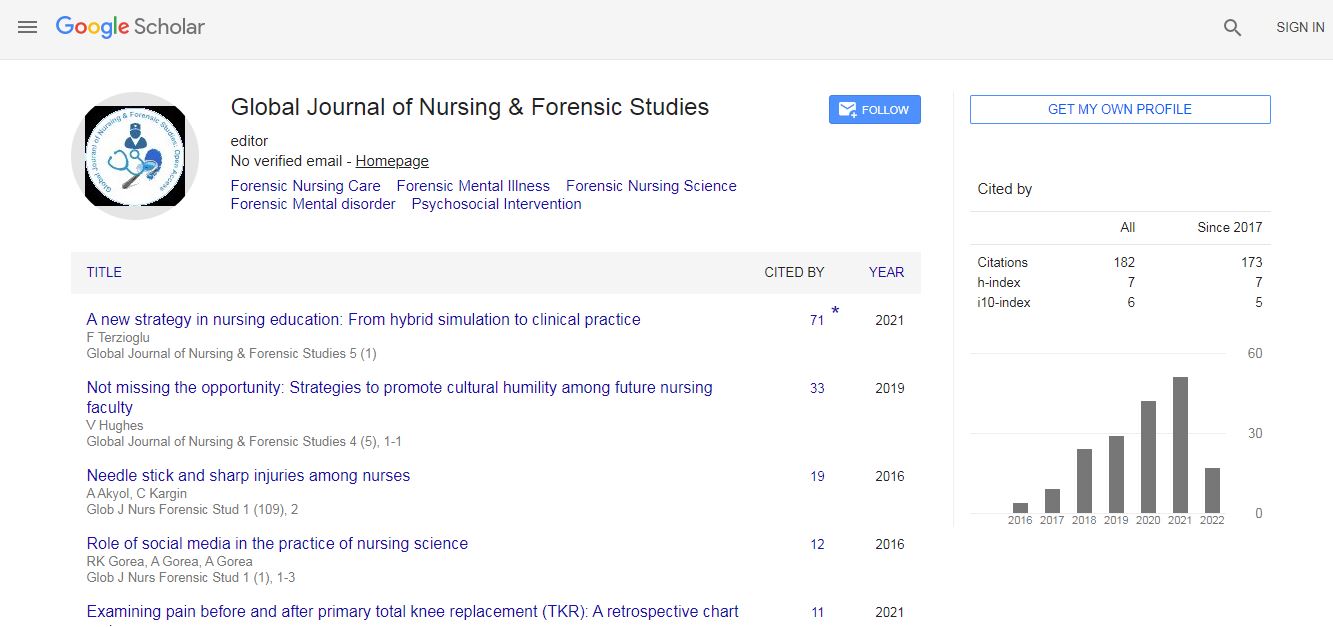
Google Scholar citation report
Citations : 82
Optometry: Open Access received 82 citations as per Google Scholar report
Indexed In
- Google Scholar
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Molecular basis of congenital glaucoma
3rd International Conference and Expo on Optometry & Vision Science
Chikezie Grand Ihesiulor and Udo A Ubani
The University of Manchester, UKAbia State University, Nigeria
ScientificTracks Abstracts: Optom open access
Abstract
Purpose: The purpose of this study was to detect pathogenic mutations in cytochrome P450, family 1, subfamily B, polypeptide 1 (CYP1B1) gene in 19 sporadic primary congenital glaucoma (PCG) cases and to identify patients lacking CYP1B1 mutations. Secondly, to conduct an in silico analysis of exome sequencing data of variants common to three related pigment dispersion syndrome (PDS) patients. Methods: CYP1B1 exon 2 and the coding part of exon 3 of 15 participants were amplified by polymerase chain reaction and amplicons were sequenced by Sanger sequencing. Sequencing data was analyzed to identify the gene mutations or SNPs. Second, the exome sequencing data of the PDS patients combined was analyzed in-house by bioinformaticians and further filtered manually to identify candidate genes for PDS. Results: Four previously reported PCG-associated CYP1B1 mutations (c.1159G>A; p.E387K, c.230T>C; p.L77P, c.1103G>A; p.R368H and c.1568G>A; p.R523K) were found in four patients out of the 15 fully ‘sequenced’ patients. Also, 10 previously reported single nucleotide polymorphisms and two novel noncoding variants were identified. Second, 21 candidate genes were found after filtering using various databases (OMIM & GeneDistiller). Nine genes (TPCN2, TYR, PAX6, DICER 1, FOXE3, TGIF1, TCF4, RPGR and CNGB3) may be of more importance since they are associated with ocular diseases. Conclusion: The relatively low percentage of PCG patients having CYP1B1 mutations (4/15=26.6%) demonstrates that other known and unknown genes may contribute to PCG pathogenesis. Lack of CYP1B1 gene mutations in some patients stresses the need to identify other responsible candidates. More analysis may be needed and the genes identified may be screened in future in other PDS patients to study PDS genetics.Biography

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi