Research Article Open Access
Prevalence and Perceived Financial Costs of Marijuana versus Tobacco use among Urban Low-Income Pregnant Women
Jessica R Beatty1*, Dace S Svikis2 and Steven J Ondersma11Department of Psychiatry and Behavioral Neuroscience, Wayne State University, Merrill Palmer Skillman Institute, USA
2Virginia Commonwealth University, USA
- *Corresponding Author:
- Jessica R Beatty
Wayne State University
Department of Psychiatry and Behavioral Neuroscience & Merrill Palmer Skillman Institute, Detroit, MI, USA
Tel: (313)664-2500
Fax: (313)664-2555
E-mail: jbeatty@wayne.edu, s.onderma@wayne.edu
Received September 05, 2012; Accepted September 24, 2012; Published September 30, 2012
Citation: Beatty JR, Svikis DS, Ondersma SJ (2012) Prevalence and Perceived Financial Costs of Marijuana versus Tobacco use among Urban Low-Income Pregnant Women. J Addict Res Ther 3:135. doi:10.4172/2155-6105.1000135
Copyright: © 2012 Beatty JR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Objective: To examine the relative prevalence of marijuana and tobacco use among low-income post-partum women, using self-report, urine, and hair testing data; and to further explore perceptions of the substances among postpartum women by evaluating perceived risk and monetary cost of prenatal marijuana versus tobacco use.
Methods: Data from two studies were available for a total of 100 (Study 1) and 50 (Study 2) low-income, primarily African-American post-partum women. Study 1 participants completed brief self-report measures of substance use as well as urine and hair samples; study 2 participants completed a brief opinion survey regarding the risks and monetary costs of prenatal marijuana use.
Results: In Study 1, the self-reported prevalence of any tobacco or marijuana use in the past three months was 17% and 11%, respectively. However, objectively-defined marijuana use was more prevalent than self-reported tobacco use: 14% tested positive for marijuana by urinalysis, and 28% by hair analysis. Study 2 participants were more likely to believe that there is a safe level of marijuana use during pregnancy, and nearly half believed that using marijuana during pregnancy was less expensive than smoking cigarettes.
Conclusion: Marijuana use may be as or more prevalent than tobacco use among low-income, African-American pregnant women. These findings may in part be attributable to perceptions of roughly equivalent cost and the lack of a clear public health message regarding prenatal marijuana use, combined with growing pro-marijuana advocacy. A broader public health response to address prenatal marijuana use, along with other substances of abuse, is needed.
Keywords
Substance use; Marijuana; Tobacco; Pregnancy; Public health policy
Prevalence and Perceived Financial Costs of Marijuana versus Tobacco Use among Low-Income Pregnant Women
Data from the National Survey of Drug Use and Health (NSDUH) suggests that past-month rates of tobacco and alcohol use among pregnant women are 15.6% and 10%, respectively-making them the most prevalent substances used during pregnancy [1]. However, marijuana is consistently found to be the most commonly used illicit drug during pregnancy, with prevalence much higher than that of cocaine (3.9% vs. 0.1% past-month use). However, the prevalence of marijuana use during pregnancy still falls far behind tobacco and alcohol in such surveys [1].
Such findings have influenced public health efforts. Higher prevalence rates, in combination with evidence of the teratogenicity for both tobacco and alcohol, have prompted numerous campaigns to reduce prenatal smoking and drinking by federal health agencies (e.g., the Centers for Disease Control and Prevention (CDC) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA)) as well as major professional societies (e.g., the American Congress of Obstetricians and Gynecologists (ACOG)). In addition, although much less prevalent than either tobacco, alcohol, or marijuana use, cocaine and other illicit drug use during pregnancy has been the focus of substantial attention from the media, Courts, and Child Welfare system [2-4].
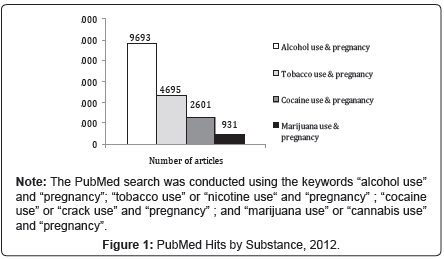
Although many studies treat marijuana as a confounding or effect modifying variable, it has received less attention as a potential teratogen than cocaine, alcohol, tobacco, or opiates. For example, as of September 4, 2012, a PubMed search revealed far fewer published studies of prenatal marijuana use than for alcohol, tobacco or cocaine (Figure 1). In addition, we are unaware of any specific education campaigns, manuals, or policy statements focusing on marijuana use during pregnancy, from any federal agency or professional society. This is in spite of (a) marijuana’s clear status as the most prevalent illicit drug; (b) evidence that tobacco and marijuana use do not decline during pregnancy to the same extent as alcohol use [5,6]; (c) evidence that marijuana contains similar levels of respiratory irritants and carcinogens as tobacco, but causes larger tar deposition and higher levels of carbon monoxide inhalation [7-9]; and (d) growing evidence that marijuana use during pregnancy is associated with deficits in growth and neurobehavioral functioning [10-12].
Further, instead of clear warnings regarding the potential risks of marijuana use during pregnancy, women may instead receive pro-marijuana messages from a range of sources. In this respect, marijuana is unique among all drugs of abuse: it is promoted by formal and informal advocacy groups as benign or even healthful. For example, many pro-marijuana sites can be easily found on the internet (one recent online review lists the “Top 50 marijuana-friendly websites” (cite http://www.marijuanareviews.com/50-marijuana-friendly-websites-828.html), some of which specifically support the use of marijuana during pregnancy (e.g., in one article appearing on a popular pro-marijuana website, a midwife referring to herself as “Dr. Kate” notes that “Marijuana is a special friend to women in their times of need . . . this good herb is a blessing, and nothing to fear at all”) [13]. Marijuana is currently the only drug of abuse that enjoys multiple, well-organized advocacy groups such as NORML (National Organization for the Reform of Marijuana Laws).
Marijuana use during pregnancy may thus merit more attention than it currently receives, even at current prevalence estimates. However, there may be reason to question current prevalence estimates among pregnant women. National surveys and most smaller-scale research studies rely on self-report measures to determine prevalence rates of substance use in pregnancy. Self-report is known to under-estimate drug use prevalence, even in anonymous national surveys [14,15], and especially with respect to drug use during pregnancy [15,16]. For example, Ostrea et al. found that 44% of three thousand women tested positive for drug use as measured by infant meconium (the infant’s first bowel movements, which can reveal drug use as far back as three months or more prior to child birth). In contrast, only 11% of these women (10% of those testing positive) admitted to drug use [17]. Because of these studies and others similar in nature, recent research has increased efforts to use biological markers of substance abuse in order to obtain more accurate prevalence rates of prenatal drug use. Evidence that marijuana is in fact more prevalent than currently thought, particularly in comparison to tobacco or alcohol, could strengthen suggestions that use of this drug during pregnancy may merit greater attention from health professionals.
The present studies had thus three specific aims. First, using data from a sample of post-partum, primarily African-American women, we sought to examine the relative prevalence of marijuana and tobacco use during pregnancy as measured by self-report, and to compare those rates to those from the NSDUH population-based sample. Second, we sought to compare prevalence of marijuana use across three methods: self-report, urine drug assay, and hair sample testing. Third, using data from a separate but similar sample of post-partum, primarily African-American women, we sought to measure the perceived risks and costs of marijuana and tobacco use during pregnancy. We predicted that (a) self-report data would roughly approximate rates of tobacco and marijuana use reported by the NSDUH; (b) rates of prenatal marijuana use as indicated by objective measures would be comparable to those of self-reported tobacco use; and (c) perceived risks and costs of prenatal marijuana use would be equivalent to those of prenatal tobacco use. Evidence that, marijuana use during pregnancy is more common than previously thought, particularly if its objectively-defined prevalence nears that of tobacco in some samples, could have significant public health implications. Similarly, evidence that increased marijuana use may be an unintended consequence of heavy tobacco taxation (as in the state of Michigan, where this study was conducted) could also have significant implications.
Study 1
As noted above, study 1 compared self-reported rates of marijuana and tobacco use during pregnancy to rates indicated by objective measures (urine and hair toxicology).
Method
Participants: Participants were 100 women recruited from their private hospital rooms, from a large urban hospital, shortly after giving birth, and after having slept. Participants in this sample were drawn from a larger study validating a drug use screening tool designed to improve identification of at-risk women by measuring risk of substance use indirectly [18]. Women were eligible to participate in the study if they were 18 years of age or older, speak english, and had no postpartum administration of narcotic pain medication.
Procedure: Participants were approached in their private hospital rooms prior to being discharged from their childbirth-related hospitalization. Those interested in participating were provided with an initial, overall consent form which was approved by the Wayne State University Institutional Review Board. Participation in all aspects of this study was completely anonymous (no names or other identifying information were recorded). All participants were asked to complete a brief computerized assessment battery that included questions regarding drug use during pregnancy, without knowledge of the pending request for hair and urine samples. After completing the computerized assessment battery, participants were recruited for a follow-up study with separate consent, involving the provision of anonymous hair and urine samples that could be used to assess recent drug use. Of those who completed the computerized assessment, 94.6% also provided a hair and urine sample. The separate consent design for the computerized assessment and the hair/urine collection was implemented to avoid creating a “bogus pipeline” response set [19].
Measures: Self-report of tobacco use was measured using audio-enhanced computer-assisted self-interview (ACASI) technology. Marijuana use was measured in three ways: self-report via ACASI, qualitative urine analysis, and hair analysis.
Self-report of tobacco and marijuana use: The ACASI software asked participants direct questions about use of tobacco and marijuana in the past three weeks and the past three months (i.e. “In the past three months have you used marijuana?”). ACASI approaches [20,21], as well as anonymity [22], have been shown to facilitate disclosure of substance use.
Objective measures of marijuana use: Objective data on recent marijuana use was obtained via qualitative urine analysis (providing a conservative estimate of marijuana use in the past 3 weeks, particularly for infrequent users; [23]), using a RediCup® instant-read device manufactured by Redwood Biotech. Objective data on the use of marijuana was also obtained via hair analysis, using a 1.5 inch sample (providing a 90-day window of detection) tested by Psychemedics, Inc., with gas chromatography/mass spectrometry confirmation of all positive results. Hair testing is an ideal “gold standard” criterion measure of drug use because of its well-established validity and long window of detection [24,25].
Results
Participants were primarily African American and low SES, with well over half reporting less than a high school education and the majority receiving public assistance of some kind (Table 1). Participants positive for marijuana use (either through hair toxicology positive result or self-report) tended to be slightly younger, to be less likely to have graduated high school, and more likely to be receiving public assistance (Table 1) similar to findings of a larger national sample of women [26]
| Study 1 Total | Study 1 Marijuana Positive | Study 1 Marijuana Negative | Study 2 Total | |
|---|---|---|---|---|
| (n = 100) | (n = 34) | (n = 66) | (n=50) | |
| Age | ||||
| 18 - 21 | 30 | 11(32.4) | 19 (28.8) | 8 (16) |
| 22 - 25 | 29 | 14 (41.2) | 15( 22.7) | 16 (32) |
| 26+ | 41 | 9 (26.5) | 32 (48.5) | 26 (52) |
| Race | ||||
| African American | 94 | 33 (97.1) | 61 (92.4) | 46 (92) |
| First Pregnancy | 25 | 9 (26.5) | 16 (24.2) | - |
| Legally Married* | 25 | 6 (17.6) | 21 (31.8) | 3 (6.3) |
| No High School Diploma or GED* | 72 | 27 (79.4) | 45 (68.2) | 21 (46.7) |
| Currently Receiving Public Assistance* | 86 | 31 (91.2) | 55 (83.3) | 43 (95.6) |
| Smoked Tobacco in Past Three Months | 17 | 11 (32.4) | 6 (10) | - |
Note: Public Assistance refers to receipt of food stamps, Woman Infant and Child food supplements (WIC), or Temporary Assistance for Needy Families (TANF). *n =45 for study 2.
Table 1: Participant Characteristics for study 1 and study 2 (Percentage in Parentheses).
Rates of use for the past three weeks: A total of 11 participants (11%) reported tobacco use in the past three weeks, a rate slightly lower than that reported by pregnant women in the 2008 NSDUH for past month tobacco use (16%). A total of 4 participants (4%) reported marijuana use in the past three weeks, a rate that again was comparable to that reported in the 2008 NSDUH for marijuana use among pregnant women (3.9%). However, the prevalence of marijuana use as measured by qualitative urine toxicology, at 14%, was higher than the self-reported rates of both tobacco and marijuana use (Figure 2). A total of 14 participants were positive for marijuana use during the past three weeks: 10 by urine toxicology results only and 4 by both self-report and urine toxicology results.
Rates of use for the past three months: A total of 17 participants (17%) reported tobacco use during the past three months, and 11 participants (11%) reported marijuana use during the past three months. However, hair testing results were marijuana-positive for 28 participants (28%). An additional 6 participants (6%) reported marijuana use despite a negative hair sample, for a total of 34 participants (34%) with some evidence of marijuana use in the past three months (Figure 2).
Co-occurrence of marijuana and tobacco use: Sixty participants (60% of the sample) showed no evidence of tobacco or marijuana use, by either self-report or toxicology. Of the 40 participants who used either tobacco (per self-report) or marijuana (per self-report or hair toxicology results), 23 (57.5%) used marijuana only, 6 (15%) used tobacco only, and 11 (27.5%) used both marijuana and tobacco for the past three months.
Discussion study 1
Rates of current self-reported tobacco and marijuana use in this sample were similar to rates of current use of tobacco and marijuana from the 2008 NSDUH. However, objective measures (urine and hair toxicology results) of recent and longer-term marijuana use revealed rates of marijuana use to be three times higher than was indicated by self-report. Further, this revised rate was in both cases higher than the rate of self-reported tobacco use; this was true despite the likelihood that urine testing missed marijuana use in the past three weeks among women whose use was relatively light or infrequent.
Study 2
Study 2 sought potential explanations for the above findings, particularly by exploring perceptions of the relative risks and relative costs of marijuana and tobacco use during pregnancy. We therefore added questions to this effect to an ongoing study of a similar sample.
Method
Participants: Participants were 50 women recruited from their private hospital room shortly after giving birth and having an opportunity to sleep; all were participants in a larger randomized control trial of the efficacy of computer-delivered brief interventions. Women were eligible to participate in the study if they were 18 years of age or older, had no postpartum administration of narcotic pain medication, and reported either illicit drug use in the month prior to pregnancy, binge drinking in the month prior to the pregnancy, or reported smoking ten or more cigarettes per day; they were excluded from the study if they were not able to understand English.
Procedure: Participants were recruited for a trial of a computer-delivered brief motivational intervention from a large urban hospital prior to being discharged from their childbirth-related hospitalization. Those interested in participating were provided with an initial, overall consent form which was approved by the Wayne State University Institutional Review Board. Of those eligible to participate, 80% agreed to participate in the study. Data utilized for Study 2 reflects items added to the 6 month follow-up observation of this study; 69% of the participants returned for the 6 month follow-up.
Measures: All questions for Study 2 were developed by our research team for this study. Again using ACASI technology, respondents answered a total of 15 items examining perceptions of the risks and costs of marijuana and tobacco use during pregnancy. Items measuring perceived risks included a request to choose the first and second most harmful (to the fetus) substance of abuse during pregnancy, as well as ordinal ratings on a 1 (not dangerous at all) to 10 (extremely dangerous) scale for each substance of abuse separately. Third, participants were asked two questions about what is a safe amount of marijuana and tobacco to be used while pregnant. Lastly, participants were asked the following question separately for cigarettes, marijuana and alcohol: “I know people who believe that (smoking cigarettes/smoking marijuana/drinking alcohol) while pregnant is really not very dangerous for the baby;” yes or no response.
Three items tapped perceived financial costs. The first item was a forced choice question about whether marijuana or tobacco costs more money to use for most pregnant women. The second and third questions asked, “How much do you think most women who smoke tobacco cigarettes/marijuana during pregnancy spend on it each day?” There were five response options: probably free for most of them (for example, others share it), $1 or $2 a day, $3-5 a day, $6-10 a day, and more than $10 a day.
Analyses: Most results from this survey are presented descriptively. When comparisons are conducted, chi-square analyses were used for comparisons of dichotomous variables and Kendall’s co-efficient of concordance and Cochran’s Q analyses were used for group comparisons between rated level of dangerousness of alcohol, tobacco and marijuana for three sets of ordinal variables.
Results
Participants were primarily African American and low SES, with the majority receiving public assistance of some kind and about half reporting less than a high school education (Table 1).
Perceived risks of marijuana versus tobacco and other substances: When forced to select the substance most likely to harm the baby if used during pregnancy, a total of 35 participants (70%) chose alcohol, 8 (16%) chose tobacco, and only one participant (2%) chose marijuana. When asked to rate separately the level of dangerousness of each substance for the developing fetus on a 1 to 10 scale (with higher scores indicating greater perceived danger), all substances were rated as highly dangerous, with mean ratings greater than 9 for all substances. Marijuana received a mean rating of 9.46 (sd=2.04), compared to 9.58 (sd=1.81) for tobacco and 9.60 (sd=1.81) for alcohol (W=0.01, X2 [2, 50]=1.0, ns). Similarly, the overwhelming majority of participants indicated that there is no safe amount of either tobacco or marijuana use during pregnancy (43, or 86% for marijuana; and 47, or 94%, for tobacco). However, significantly more women were willing to report a safe amount of marijuana than tobacco (X2 [3, 50]=14.95, p<0.01); with two women reporting half a joint, four women reporting one joint, and one woman reporting two to three joints as safe amounts to use while pregnant.
With respect to perceptions of community norms, a total of 38 participants (76%) reported knowing people who felt the use of marijuana during pregnancy was not very dangerous for the baby. A total of 36 (72%) reported knowing people who felt use of cigarettes was not very dangerous, and 26 (52%) reported knowing people who felt use of alcohol during pregnancy was not very dangerous (Q [2]=14.6, p<0.01). The proportion of the latter was lower than that for marijuana (Q [1] = 12.0, p < .01) or tobacco (Q [1]=8.3, p<0.01).
Perceived financial cost of marijuana versus tobacco and other substances: A total of 22 participants (44%) reported that marijuana costs less to use during pregnancy than cigarettes. Similarly, when asked separately about money spent per day by women using marijuana or tobacco during pregnancy, the median response for both marijuana and tobacco was six to ten dollars.
Overall Discussion
Taken together, study 1 and study 2 provide preliminary evidence that (a) although self-reported rates of marijuana use in this sample of pregnant, low-SES African-American women were similar to those reported in the NSDUH, evidence from urine and hair samples suggested that marijuana use was much higher; (b) these objectively-defined rates of marijuana use were equivalent to or greater than that for tobacco use; and (c) compared to tobacco use, marijuana is seen as roughly equivalent in cost and as equivalent or perhaps somewhat less harmful to the developing fetus. Importantly, a very high proportion of participants in study 2 (75%) reported knowing someone who believed that marijuana use during pregnancy was not harmful.
Limitations
These findings should be considered in light of this study’s limitations. For example, objective measures of tobacco use (urine toxicology measures of cotinine) were not available for study 1. Despite the relative lack of stigma associated with tobacco, a legal substance, it will nevertheless be important for future research to compare rates of tobacco and marijuana use using objective measures in order to address the possibility of under-reporting of tobacco use as well. In addition, participants in both studies were from a small and relatively homogenous sample of urban low-SES African-American post-partum women, who may have been unique in their level of substance use during pregnancy, openness in admitting to their use, and opinions on safety of use during pregnancy. Although it is crucial to better understand the behavior and opinions of this high-risk group, findings from this homogenous and unique sample may not generalize to other groups of pregnant women.
Implications
In spite of these limitations, these findings appear to have at least two clear implications. First, although under-reporting is a well-known phenomenon, these findings highlight a specific possible consequence of under-reporting: marijuana use, previously thought to be much less prevalent than tobacco use during pregnancy, may actually have similar prevalence in some samples. Consistent with recent NSDUH data regarding pregnant African-American women (7.0% reported marijuana use and 13.5% reported tobacco use in the 2009-2010 NSDUH), overall rates of marijuana use in this sample were high, and eclipsed those for self-reported tobacco use. The relative prevalence of marijuana use as compared to tobacco use in this sample-along with the perceptions of lower risk and equivalent cost to tobacco-provides further evidence that the status of current efforts to reduce marijuana use during pregnancy must be re-evaluated. The teratogenicity of marijuana is less clear than that of tobacco, perhaps more because of the paucity of research than because of a consistent lack of positive findings. There is a need for (a) more studies of the effects of prenatal marijuana exposure; and (b) greater attention to educating women of the potential risks of prenatal marijuana use. As noted earlier, efforts regarding the latter will face the unique challenge of counteracting broad formal and informal messages that marijuana is benign or even healthy for pregnant women.
Second, the perception of roughly equivalent costs raises the possibility that larger political and cultural factors may be causing a change in patterns of prenatal substance use. Considering the US as a whole, the average state tax on cigarettes increased from 32.7 cents in 1995 to about $1.20 a pack in 2009 [27]. Michigan’s excise tax on cigarettes, at $2.00 per pack, ties it with four other states for the 11th highest rate among the 50 states. At the same time, Michigan is one of 15 states to have legalized medical marijuana, as openness to decriminalization of marijuana continues to grow nationwide [28]. Recent findings from the Monitoring the Future survey has shown similar trends in teenagers: 2011 data indicate that past month marijuana use (22.6%) surpassed past month tobacco use (18.7%) in high school seniors [29]. These factors, together with the above-noted consistency of public health messages regarding prenatal tobacco use and the relative silence of public health services regarding marijuana use, may be facilitating a shift from one substance to the other.
More research is needed, particularly with regard to whether the relative neglect of marijuana as a potential teratogen, combined with tobacco-oriented public health and taxation policies, could be facilitating a shift toward marijuana use among some pregnant women. Great insight regarding relative prevalence, relative harm, and possible unintended consequences of some prevention efforts would help public health efforts to effectively target prevention strategies.
Acknowledgements
Funding support for this project was provided by NIDA grants DA R21 018975 and DA R01 021329. The authors would like to thank Dr. Phebe Lam and Veronica Connors-Burge for their assistance with recruitment and data collection.
References
- Substance Abuse and Mental Health Services Administration (2009) Results from the 2008 National Survey on Drug Use and Health: National Findings. Substance Abuse and Mental Health Services Administration, Rockville, MD
- Ginsburg HJ, Raffeld P, Alanis KL, Boyce AS (2006) Comparing attitudes about legal sanctions and teratogenic effects for cocaine, alcohol, tobacco and caffeine: a randomized, independent samples design. Subst Abuse Treat Prev Policy 1: 4.
- Lewis D (2005) We were wrong about "crack babies": are we repeating our mistake with "meth babies"? MedGenMed 7: 30.
- Minnes S, Singer LT, Humphrey-Wall R, Satayathum S (2008) Psychosocial and behavioral factors related to the post-partum placements of infants born to cocaine-using women. Child Abuse Negl 32: 353-366.
- Moore DG, Turner JD, Parrott AC, Goodwin JE, Fulton SE, et al. (2010) During pregnancy, recreational drug-using women stop taking ecstasy (3,4-methylenedioxy-N-methylamphetamine) and reduce alcohol consumption, but continue to smoke tobacco and cannabis: initial findings from the Development and Infancy Study. J Psychopharmacol 24: 1403-1410.
- Bailey JA, Hill KG, Hawkins JD, Catalano RF, Abbott RD (2008) Men's and women's patterns of substance use around pregnancy. Birth 35: 50-59.
- Moolchan ET, Zimmerman D, Sehnert SS, Zimmerman D, Huestis MA, et al. (2005) Recent marijuana blunt smoking impacts carbon monoxide as a measure of adolescent tobacco abstinence. Subst Use Misuse 40: 231-240.
- Wu TC, Tashkin DP, Djahed B, Rose JE (1988) Pulmonary hazards of smoking marijuana as compared with tobacco. N Engl J Med 318: 347-351.
- World Health Organization (WHO) Division of Mental Health and Prevention of Substance Abuse (1997) Cannabis: A health perspective and research agenda.
- Fried PA (2002) The consequences of marijuana use during pregnancy: A review of the human literature. In: Russo E, Dreher M, Mathre ML (eds.). Women and cannabis: Medicine, science, and sociology. Haworth Press, New York 85-104.
- El Marroun H, Tiemeier H, Steegers EA, Jaddoe VW, Hofman A, et al. (2009) Intrauterine cannabis exposure affects fetal growth trajectories: the Generation R Study. J Am Acad Child Adolesc Psychiatry 48: 1173-1181.
- Gray TR, Eiden RD, Leonard KE, Connors GJ, Shisler S, et al. (2010) Identifying prenatal cannabis exposure and effects of concurrent tobacco exposure on neonatal growth. Clin Chem 56: 1442-1450.
- Dr. Kate (1998) Pregnancy and pot.
- Fendrich M, Johnson TP, Sudman S, Wislar JS, Spiehler V (1999) Validity of drug use reporting in a high-risk community sample: a comparison of cocaine and heroin survey reports with hair tests. Am J Epidemiol 149: 955-962.
- Derauf C, Katz AR, Easa D (2003) Agreement between maternal self-reported ethanol intake and tobacco use during pregnancy and meconium assays for fatty acid ethyl esters and cotinine. Am J Epidemiol 158: 705-709.
- Markovic N, Ness RB, Cefilli D, Grisso JA, Stahmer S, et al. (2000) Substance use measures among women in early pregnancy. Am J Obstet Gynecol 183: 627-632.
- Ostrea EM Jr, Brady M, Gause S, Raymundo AL, Stevens M (1992) Drug screening of newborns by meconium analysis: a large-scale, prospective, epidemiologic study. Pediatrics 89: 107-113.
- Ondersma SJ, Svikis DS, Lebreton JM, Streiner DL, Grekin ER, et al. (2012) Development and preliminary validation of an indirect screener for drug use in the perinatal period. Addiction.
- Lowe JB, Windsor RA, Adams B, Morris J, Reese Y (1986) Use of a bogus pipeline method to increase accuracy of self-reported alcohol consumption among pregnant women. J Stud Alcohol 47: 173-175.
- Murphy DA, Durako S, Muenz LR, Wilson CM (2000) Marijuana use among HIV-positive and high-risk adolescents: a comparison of self-report through audio computer-assisted self-administered interviewing and urinalysis. Am J Epidemiol 152: 805-813.
- Turner CF, Villarroel MA, Rogers SM, Eggleston E, Ganapathi L, et al. (2005) Reducing bias in telephone survey estimates of the prevalence of drug use: a randomized trial of telephone audio-CASI. Addiction 100: 1432-1444.
- Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC (2007) Discrepancies in estimates of prevalence and correlates of substance use and disorders between two national surveys. Addiction 102: 623-629.
- Wolff K, Farrell M, Marsden J, Monteiro MG, Ali R, et al. (1999) A review of biological indicators of illicit drug use, practical considerations and clinical usefulness. Addiction 94: 1279-1298.
- Kintz P, Villain M, Cirimele V (2008) Chemical abuse in the elderly: evidence from hair analysis. Ther Drug Monit 30: 207-211.
- Wada M, Nakashima K (2006) Hair analysis: an excellent tool for confirmation of drug abuse. Anal Bioanal Chem 385: 413-415.
- van Gelder MM, Reefhuis J, Caton AR, Werler MM, Druschel CM, et al. (2010) Characteristics of pregnant illicit drug users and associations between cannabis use and perinatal outcome in a population-based study. Drug Alcohol Depend 109: 243-247.
- Centers for Disease Control and Prevention, MMWR weekly (2009) Federal and state cigarette excise taxes --- United States, 1995--2009. 58: 524-527.
- Pew Research Center (2010) Public support for legalizing medical marijuana: Modest rise in percentage favoring general legalization.
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE (2012) Monitoring the Future. National results on adolescent drug use: Overview of key findings, 2011. The National Institute on Drug Abuse, National Institutes of Health, Institute for Social Research, The University of Michigan Institute for Social Research.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 16600
- [From(publication date):
October-2012 - Dec 07, 2025] - Breakdown by view type
- HTML page views : 11797
- PDF downloads : 4803