Research Article
Who Caesarean Section Rate: Relevance and Ubiquity at the Present Day – A Review Article
| Susana Teixeira1, Humberto S Machado1,2* | |
| 1Instituto de Ciências Biomédicas Abel Salazar – Universidade Porto, Porto, Portugal | |
| 2Serviço de Anestesiologia, Centro Hospitalar do Porto, Porto, Portugal | |
| Corresponding Author : | Humberto S Machado Serviço de Anestesiologia Centro Hospitalar do Porto, Portugal Tel: +351.9358484753 E-mail: hjs.machado@gmail.com |
| Received date: Feb 14, 2016; Accepted date: Mar 12, 2016; Published date: Mar 17, 2016 | |
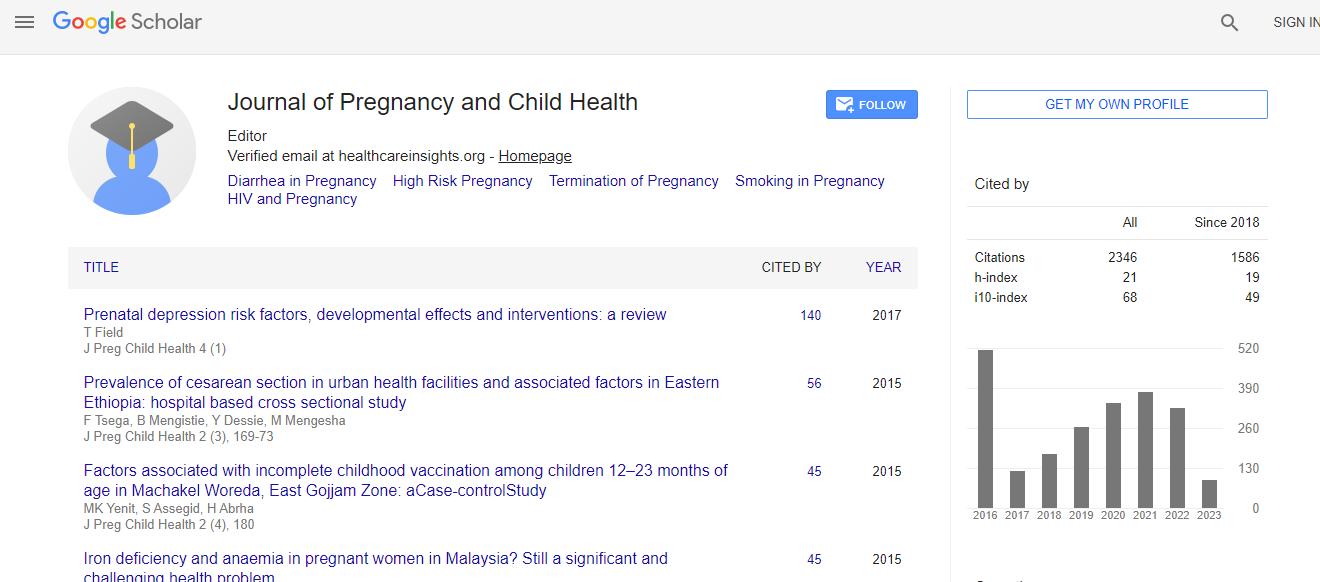
| Citation: Teixeira A, Machado HS (2016) Who Caesarean Section Rate: Relevance and Ubiquity at the Present Day – A Review Article. J Preg Child Health 3:233. doi:10.4172/2376-127X.1000233 | |
| Copyright: © 2016 Teixeira S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Background: In 1985 the World Health Organization (WHO) claimed that there were no reasons for any region in the world to have a caesarean section (CS) rate above 10-15%. Even so, many of the developed countries present superior CS rate. Although CS rate rise in countries with high maternal and neonatal morbi-mortality is benefice, doubts exist about countries that already present a high CS rate, because some concern exist that above a certain limit, the risks are superior to the benefits. The aim of this review is to analyse the CS rate in different countries and to determinate if the WHO limit can be applied to all. Also to compare the maternal and neonatal morbidity and mortality between vaginal and CS birth, trying to evaluate the best way to deliver. Methods: Data about CS rate, maternal mortality, neonatal mortality and Human Development Index (HDI) was collected from official reports and scientific papers. Results: The world CS rates varies from 1.5% in Ethiopia to 56.6% in Brazil. The rate is superior in countries with high HDI, and inferior in poor countries. In general, countries with high CS rate present a low maternal and neonatal mortality. The opposite is observed in poor countries. Conclusion: Since the WHO declaration many changes occurred in society, in the women status and in medicine, making us question if the 15% limit is still updated. The different social-economic, cultural and ethnographic reality of each country suggests that a global CS rate should not exist. Instead, each country should adjust CS rate to its necessities and focus on providing this option to any women who needs it. Some evidence suggests that CS can have a higher maternal and neonatal morbi-mortality when compared with vaginal delivery, however it has also positive aspects that should be taken in consideration.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi