Research Article
Viral Infections in Renal Transplant Recipients in Belarus
| Tamara Vasil’evna Amvrosieva1*, Zoya Fedorovna Bogush1, Natallia Uladzimirauna Paklonskaya1, Oleg Valentinovich Kalachik2, Elena Petrovna Kishkurno3 and Kanstantsin Leanidavich Dziadziulia1 | ||
| 1The Republican Research and Practical Center for Epidemiology and Microbiology, Minsk, Belarus | ||
| 2The Republican Scientific and Practical Center of Organ and Tissue Transplantation, Minsk, Belarus | ||
| 3Belarusian Medical Academy of Post-Graduate Education, Minsk, Belarus | ||
| Corresponding Author : | Dr. Tamara Amvrosieva The Republican Research and Practical Center for Epidemiology and Microbiology 23, Philimonov str., 220114, Minsk, Republic of Belarus Tel: +375172650896 E-mail: amvrosieva@gmail.com |
|
| Received February 20, 2015; Accepted April 24, 2015; Published April 30, 2015 | ||
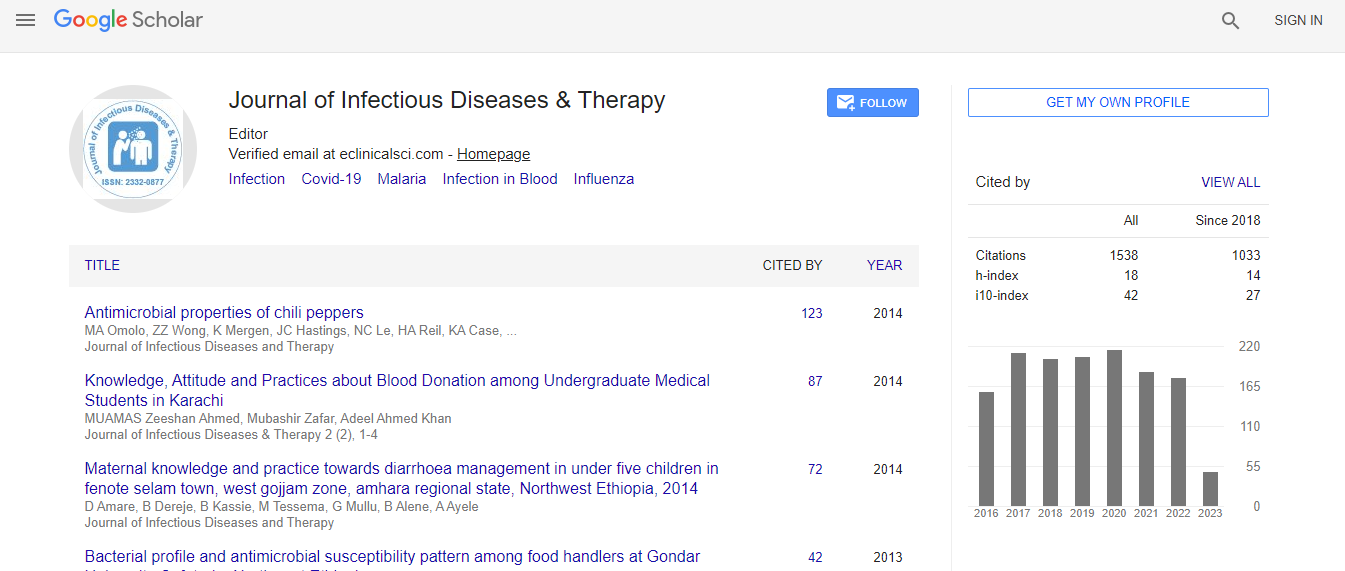
| Citation: Amvrosieva TV, Bogush ZF, Paklonskaya NU, Kalachik OV, Kishkurno EP, et al. (2015) Viral Infections in Renal Transplant Recipients in Belarus. J Infect Dis Ther 3: 212. doi: 10.4172/2332-0877.1000212 | ||
| Copyright: © 2015 Amvrosieva T et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | ||
Related article at Pubmed Pubmed  Scholar Google Scholar Google |
||
Abstract
The presented study had its aim in establishing the prevalence and etiological structure of post-transplant viral complications and the kinetics of infection development. Two groups of recipients were examined: Group 1 comprised patients without any clinical signs of infection (n=84) monitored for a year, Group 2 included recipients with a clinical presentation of infection (n=92). 591 blood samples and 446 urine samples from 196 patients (20 donors and 176 renal transplant recipients) were analyzed. All donor-recipient pairs were tested for CMV, EBV, and HSV-1, 2. Latent viral infection reactivation was detected by the presence of viraemia (DNAemia) induced by CMV, EBV, HSV-1, 2, HHV-6, VZV, PVB19, or viruria (DNAuria) induced by BKV.
The percentage of Group 1 patients with viral DNA detected amounted to 41.9% for CMV, 30.4% for EBV, 17.4% for BKV, 5.6% for HHV-6, 1.9% for AdV, and 1.7% for PVB19. HSV-1, 2 and VZV infections in this group were not observed. The rate of CMV, EBV, and BKV infection reactivation, determined by the viraemic patients percentage, increased with time and peaked 1, 1.5 and 2 months after transplantation for EBV, BKV, and CMV, respectively. Three to six months after transplantation, the percentage of patients with active CMV, EBV, or BKV infection decreased significantly; and later on, viraemia was only occasional finding in Group 1 patients. Examination of Group 2 patients revealed that the predominant etiological agents of post-transplant viral complications were CMV (24.4%), EBV (18.8%), and BKV (17.6%).
The current study is the first complex investigation into the etiological structure and activation kinetics of viral infections in renal transplant recipients in Belarus. The results have major implications for early prevention of potential viral complications and adjustment of the therapy regimens for kidney transplant recipients currently in use.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi