Vascular Dementia: A Revision
*Corresponding Author: Dr. Zia Shariat-Madar, Department of Biomolecular Sciences, Division of Pharmacology, School of Pharmacy, University of Mississippi, MS 38677, US, Tel: (+1) 662-915-5150, Email: madar@olemiss.eduReceived Date: May 18, 2021 / Accepted Date: Jun 01, 2021 / Published Date: Jun 08, 2021
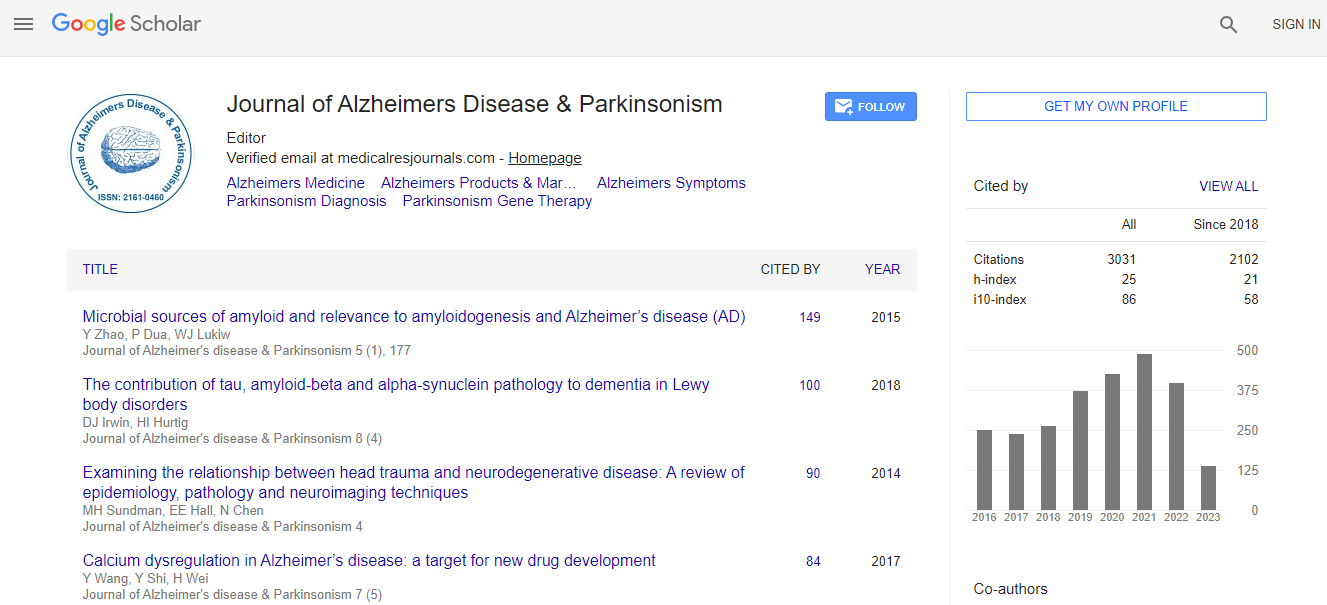
Citation: Hawkins B, Shariat-Madar Z (2021) Vascular Dementia: A Revision. J Alzheimers Dis Parkinsonism S4: 018.
Copyright: © 2021 Hawkins B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The prevalence of Alzheimer disease, a degenerative dementia, in North America is approximately twice the worldwide average. Alzheimer disease’s range is somewhere between 60 to 80 percent of all cases of dementia, whereas 15 to 34 percent of dementia cases exhibit significant vascular pathology during postmortem neuropathological examination. Prolonged persistence of reduced blood flow and microscopic bleeding in brain tissue lead to vascular dementia. The etiology and pathogenic mechanisms for vascular dementia are still an enigma, although the impaired cardiovascular and cerebrovascular systems are thought to play a role. Vascular dementia is classified as cognitive impairment induced by either cardiovascular disease, ischemia, or hemorrhagic brain injury. The vital role of both the cardiovascular and cerebrovascular system is to maintain a relatively smooth blood flow through capillaries, which infiltrate every tissue and every cell in the body. Brain capillaries are capable of adjusting blood flow to meet the metabolic needs of the brain in response to neural activity. The circulatory system has the capability to minimize functional diffusion distance within tissues. The central nervous system and endocrine system assist in making constant adjustments to the blood flow as conditions change in tissues and cells. An increase in diffusion distance or alterations in the structure of the arterioles, an important vascular resistance site within the entire vascular network, in response to long-term physiological alterations in blood flow brought about by chronic disease may be the first manifestation of the breakdown of nerve cells. Accordingly, the purpose of this review is to offer a hypothetical link between persistent peripheral cardiovascular-related diseases and vascular dementia and will present potential mechanistic connections underlying observed effects.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi