Therapeutic Effects of Neuromuscular Electrical Stimulation and Hyperboloid Mastication Apparatus on Masticatory Biomechanical Function in Down Syndrome and their Influences on Saliva, Sleep Disorders and Body Adiposity
*Corresponding Author: Mônica Fernandes Gomes, Department of Biopathology and Diagnosis, Institute of Science and Technology, São José dos Campos Campus, São Paulo State University–UNESP, São José dos Campos, São Paulo, Brazil, Email: monica.gomes@unesp.brReceived Date: Nov 03, 2023 / Published Date: Dec 04, 2023
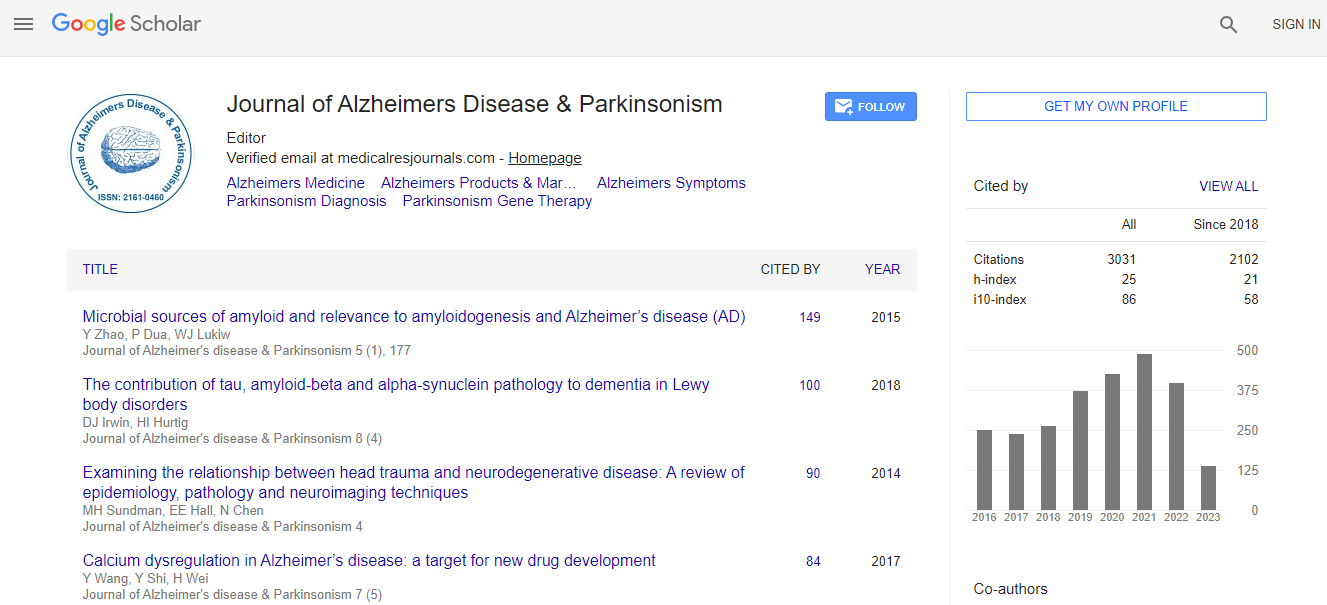
Citation: Petersen M, Ferman TJ, Zhang F, Pedraza O, Wszolek ZK, et al. (2023) Therapeutic Effects of Neuromuscular Electrical Stimulation and Hyperboloid Mastication Apparatus on Masticatory Biomechanical Function in Down Syndrome and their Influences on Saliva, Sleep Disorders and Body Adiposity. J Alzheimers Dis Parkinsonism 13:587.DOI: 10.4172/2161-0460.1000587
Copyright: © 2023 Petersen M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To evaluate the therapeutic effects of surface Neuromuscular Electrostimulation (sNMESS) and Masticatory Device with Hyperboloid (MDHB) on Masticatory Biomechanical Function (MBF) in Down Syndrome (DS). Their influences on salivary parameters, sleep disorders and body adiposity and their risks were analyzed.
Methods: Ten subjects with DS underwent the MBF evaluation and divided into two groups: sNMES and MDHB. Electrical activities of masseter and temporal muscles, maximum bite force-mBF and Maximum Mouth Opening (MMO) were investigated. Saliva testing (Salivary Flow Rate (SFR); pH value; Buffer Capacity (BC); Salivary Cortisol (SC) levels, morning and night periods; and Pseudomonas Aeruginosa-Pa identification), polysomnography type II test (Apnea-Hypoapnea Index (AHI), Snoring Index (SI) and Sleep Bruxism Index (SBI)) and anthropometric measures (Body Mass Index (BMI); Neck Circumference (NC); Abdomen Circumference (AC) and Waist-to-Hip Ratio-WHR) were done.
Results: Electrical activities were higher in sNMES than MDHB; in contrast, mBF gain and mMO reduction was enhanced in MDHB. The hyposalivation was eliminated in both the therapies. SFR was increased and BC reached normality, especially in MDHB. High levels of morning-SC were found in both therapies. PA-identification was negative. Mean AHI-SI were increased in MDHD therapy. Mean SBI was reduced in both therapies. Value means of BMI-NC-AC and BMI- AC was increased MDHB and sNMES, respectively.
Conclusion: sNMES provided better functional synergy of the masticatory muscles. MD HB substantially stimulated saliva production and intensified OSA severity. Both therapies are not recomended to treat OSA once the mean AHI >30 was maintained. SB events were markedly reduced.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi